ABSTRACT
We aimed to study the correlation between psychosocial-economic factors among patients that underwent autologous HCT, hospitalization duration, and 6-months recurrent admissions. We performed a historical prospective study of all consecutive patients who underwent autologous HCT (myeloma, n=105; lymphoma, n=107) in our center between 2001 and 2017. Pre-admission, patients underwent a full psychosocioeconomic evaluation in which their occupation, living standards, involvement of a caregiver, coping abilities and need for further assistance were assessed by a single designated HCT coordinating nurse. Diagnosis of lymphoma, compared with myeloma, was associated with prolonged hospitalization by 3.41(p=.003) as did a pre-transplant recommendation for further social/psychologist assistance (by 1.89-fold, p=.033), while each additional point in the scale, assessing “caregiver-potency”, correlated with .835 days decrease in hospitalization duration (p=.021). A pre-transplant recommendation of assistance was also associated with 2.42-fold increase in recurrent admissions (p=.016), while patients increased coping ability of was associated with 37% reduction in the chances of recurrent admission (p=.038). We conclude that factors which reflect a patient’s support system and psychological strength are better predictors of clinical outcomes than standard factors associated with socio-economic status. Recognizing patients who require further assistance and providing them with a better support system may improve clinical outcomes.
Keywords: Autologous Hematopoietic Cell Transplantation; Lymphoma; Myeloma; Psychosocial; Socioeconomic Status; Hematopoietic Recovery
Introduction
High dose therapy and autologous hematopoietic cell transplantation (HCT) remains the standard of care for relapsed patients with non-Hodgkin Lymphoma [1], relapsed/refractory Hodgkin’s lymphoma [2], and a first line therapy for eligible patients with multiple myeloma (MM)[3]. Data about the effect of economic and psychosocial factors on clinical outcomes are scarce and only few studies have addressed this issue. While several studies demonstrated an improved clinical outcomes in patients with more favorable psychosocial factors [4-6], other studies failed to show such an effect [7,8]. We have previously shown that in patients with lymphoma ≥65 years who underwent autologous HCT, the combination of lower economic status, no social support and lower motivation were associated with prolonged hospitalization and recurrent admissions [9]. We hypothesized that a variety of socioeconomic parameters may also impact transplantation course in both younger and elderly patients with either lymphoma or myeloma and may provide further insights for pre and peri transplant interventions.
Methods
We conducted an historical prospective study of consecutive patients that were sampled from database of the Bone Marrow Transplantation Unit in the Tel Aviv Medical Center. We included both male and female patients above the age of 18 years, who were diagnosed with either lymphoma or myeloma and underwent first autologous HCT between May 2001 and December 2017. Patients were excluded if they had an allogeneic HCT, had a tandem autologous HCT (performed within 6 months apart), or if data pertaining to their transplantation or psychosocial parameters were lacking. All patients underwent a full psychosocial-economic evaluation (PSE) by a single designated bone marrow transplantation coordinating nurse, including a detailed questionnaire, prior their admission to transplant (Supplement). In our center, the absence of a caregiver does not exclude a patient from undergoing HCT. The following domains were evaluated in the interview and questioner – Occupation (Unemployed, Academic, non-academic); Ethnicity (Sephardic Jew, Ashkenazi Jew, Arabic, medical-tourism); Living standards (owning of apartment or a house); Involvement of a caregiver (a 0-5 scale where 0 is no care giver and 5 is a fully involved and dedicated care giver); Coping abilities (0-5 scale where 0 is no ability and 5 fully capable to cope with the transplantation process); and recommended assistance (yes or no recommendation of the transplantation coordinator nurse for social worker/psychologist assistance throughout the transplantation course).
We evaluated the impact of all the above mentioned domains
on the duration of hospitalization during HCT and recurrent
admissions to the hospital in the first 6 months after HCT. The
following criteria were used for referring patients for a social
worker or psychological intervention.
a) The absence of a caregiver.
b) The request of the patient/caregiver or the primary provider.
c) Subjective evaluation performed by the coordinator nurse.
This study was conducted in accordance to the declaration of
Helsinki that was approved by the Tel Aviv Medical Center ethic
committee.
Preparative Regimen and Supportive Care
Hematopoietic stem cells were either mobilized using G-CSF solely, intravenous cyclophosphamide and G-CSF, or after salvage chemotherapy, when appropriate. Hematopoietic cells were cryopreserved at −195°C using cryoprotectant mixture consisting of 5% dimethyl sulfoxide (DMSO), albumin, and saline. Preparative regimen in lymphoma patients was BEAM (carmustine - 300 mg/ m², etoposide – 200-400 mg/m² x 4 days, cytarabine – 200-400 mg/ m² x 4 days and melphalan - 140 mg/m²) or in myeloma patients (n=105) was melphlan (140-200 mg/ m²).
All patients were hospitalized in the Bone Marrow Transplantation Unit in designated rooms with high efficiency particulate air (HEPA) filters. All patients were given prophylaxis with acyclovir from starting of conditioning. In addition, patients with lymphoma were given ciprofloxacin and fluconazole on day neutrophils count decreased below 500/microL. Transfusions were given, in general, in cases hemoglobin (Hb) dropped below 7 gr/dL and platelets dropped below 10000/dL.
Statistical Analysis
Continuous variables were described as the mean, median, standard deviation and range of number observations, as applicable. Categorical data were described with contingency tables including frequency and percent. Confidence intervals were calculated at the (two-sided) 95% level of confidence. Multiple linear regression and binary logistic regression were calculated to predict the impact of the various domains of PSE on the duration of hospitalization and on recurrent admissions, respectively. Preliminary analyses were performed to ensure there was no violation of the assumption of normality, linearity and multicollinearity. Patients who died during the first month after HCT were excluded from the analyses of factors associated with duration of hospitalization, and patients who died during the first 6 months post HCT were excluded from the analyses of factors associated with recurrent admissions. A two-sided P value of <.05 was considered to be statistically significant. We used SPSS version 23 and Prism version 5.0 to perform the analyses.
Results
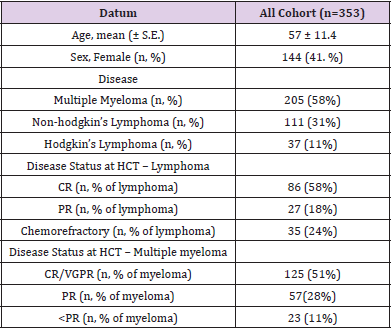
Between January 2001 and December 2017, we identified 227 patients who met the inclusion criteria and underwent autologous HCT at the Tel Aviv Medical Center. Fifteen patients were excluded because of lack of follow up data. The final dataset included 353 patients (lymphoma, n=148 and myeloma, n=205). Patients’ characteristics are elaborated in Table 1. Mean age was 57 (±11.4) years. Median durations of hospitalization for patients with multiple myeloma and lymphoma were 18 (range, 12-49) days and 24 (range, 18-62) days, respectively. By 1 month post HCT there were 10 deaths (5 because of disease progression and 5 because of non-relapse mortality). By 6 months post transplantation there were 8 additional deaths – all due to disease progression. Overall survival at 1 and 6 months were 96% (95% CI 91%-99%, and 93% (95% CI 86%-98%), respectively.
Table 1: Patients’ and Disease’s Characteristics.
Note: HCT- Hematopoietic Cell Transplant; CR – Complete Response; PR- Partial Response; VGPR -Very Good Partial Response
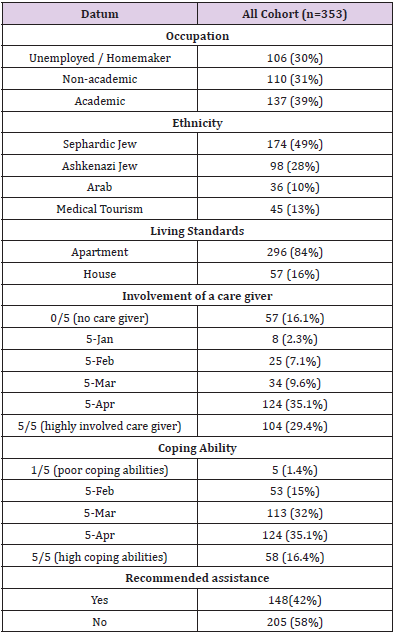
Evaluation of Psychosocial Economic Factors
Table 2 depicts the various parameters evaluated by the transplantation coordinator nurse. Regarding job employment, 70% of the patients were employed in the previous year prior to HCT. Considering the care giver, 16.1% of the patients did not have a designated transplantation caregiver. Identification of the caregiver in the majority of cases was a spouse (n=204, 76%), a parent (n=29, 9.7%), a sibling (n=23, 7.8%), a child (n=28, 9.5%), or a friend (n=12, 4%). Gender of the caregiver in majority of the cases was female (n=233, 79%). 28 patients (8%) had a psychiatric illness (majority with history of anxiety taking supplement drugs). Based on the patient’s coping ability the existence of a fair caregiver and ongoing co-morbidities, the transplant coordinator nurse, recommended a social worker/psychologist intervention and support in 42% of the patients. In 21 cases (6%) the coordinator nurse recommended intervention prior to admission because of reluctancy/incapability of the patient to continue to HCT. In all cases patients underwent intervention and eventually proceeded to HCT.
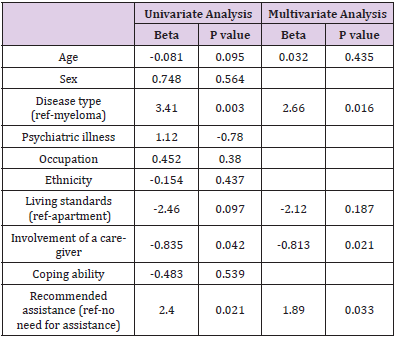
Correlation of Factors with Duration of Hospitalization
The mean duration of hospitalization was 23± 10 days. Table 3 depicts univariate and multivariate analyses of correlation between the various factors and the duration of hospitalization. In multivariate analyses lymphoma (vs. myeloma) and the recommendation of social assistance prior to HCT, were both correlated with prolonged duration of hospitalization, while a better involvement of a care giver was associated with shortening of hospitalization. Coefficient analyses showed that each point of increase in the scale of the care giver involvement was associated with a -.835 days decrease in the hospitalization duration. Recommendation for social worker/psychologist was associated with a 2.4 days increase in the hospitalization period.
Table 3: The effect of Psychosocio-economic factors on duration of hospitalization.
Note: Data are reported as beta. Beta=regression coefficient, shows the strength and the direction of the variable’s impact.
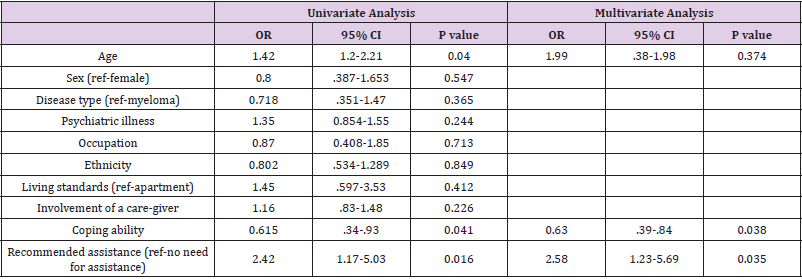
Correlation of Factors with Recurrent Hospitalization
Data for recurrent hospitalizations after HCT were available in 284 patients (80%). Of them, 71 patients (25%) were admitted to the hospital within 6 months from HCT (1 admission, n=53, 18.6%; 2 admissions, n=13, 4.6%; >2 admissions, n=5, 1.8%). Out of all admissions, majority were related to toxicity (infections, n=31, 44%, and organ dysfunction, n=7, 10%). thirty-three patients (46%) were admitted because of relapse/progression of disease.
Table 4 depicts univariate and multivariate analyses of correlation between the various factors and recurrent hospitalizations. On univariate analyses, both age and recommendation for having assistance were associated with an increased risk for hospitalization, while higher coping ability was associated with a decreased risk for recurrent hospitalization. On multivariate analyses, age lost statistically significance, while increased coping ability was associated with 37% reduction in the chances for recurrent admission (p=.038), whereas recommended assistance, was associated with 2.4 fold increase in the chances for recurrent admission (p=.035). Of note, involvement of care giver did not impact readmission rates.
Table 4: The effect of Psycho-socio-economic Factors on Recurrent Hospitalizations.
Note: OR: odds ratio.
Discussion
In this study we aimed to examine the correlation between psychosocial-economic factors and clinical outcomes, namely hospitalization length and recurrent admissions, in lymphoma and myeloma patients who underwent autologous HCT. We showed that a better caregiver involvement correlates to a -.835 days decrease in the hospitalization duration, and a referral to a social worker/ psychologist for further assistance correlates with 2.4 days increase in the hospitalization period. A recommendation of assistance was also associated with 2.4-fold increase in the chances for recurrent admission (p=.035), while increased coping ability was associated with 37% reduction in the chances for recurrent admission (p=.038). Interestingly, factors pertaining solely to socio-economic status, such as occupation, living standards and ethnic background did not have a significant effect on hospitalization duration or recurrent hospitalizations.
Patients undergoing autologous HCT experience a higher rate of fatigue, physical disability, anxiety and depression [10], which points to their need for a strong support system. The association, however, between psychosocial-economic factors, such as income rate, support of family and friends or ethnic background, is not clear. In some studies, poorer psychosocial factors were associated with worse clinical outcomes and perceived poor social support were negatively associated with survival in patients undergoing HCT4, while optimism and reduced anxiety were associated with a shorter time to neutrophil engraftment in MM patients5. A lower socioeconomic status, defined by annual household income, was found to be associated with a higher relapse mortality, and lower overall and progression free survival in patients with lymphoma who underwent autologous HCT. This correlation was not found in patients with myeloma7,8. Similarly, a large cohort study failed to show a correlation of socio-economic status and post-transplant clinical outcomes, such as day of neutrophil or platelet engraftment and overall survival6. Likewise, our study shows that factors which reflect a patient’s support system and psychological strength are better predictors of clinical outcomes, than factors describing a patient’s socio-economic status.
Psychosocial factors, specifically coping abilities and a patient’s support system, can be difficult to define and compare between patients; in the abovementioned studies, different questionnaires and scales were used to assess these factors in patients. A major power of our study is the fact that a single designated nurse performed the same evaluation for each patient undergoing autologous HCT for almost 20 years, decreasing inter-observer variability and making the assessment of patients’ coping ability or need for further assistance comparable between patients.
Our study has several limitations. First, the definition of a living standard as apartment or house might not accurately reflect socioeconomic status, which is also true for occupation; it is possible that income rate would have been a better predictor of outcomes, however these data are limited. Second, the defined categories imply to the local population and may not be generalized to other communities. Third, the fact that “Fitter” patients are selected for HCT, may be associated with a selection bias of the cohort.
Conclusion
In conclusion, in this study we demonstrated an association between psychosocial factors which include coping abilities, caregiver support and need for professional support, and clinical outcomes – hospitalization length and recurrent hospitalizations. Psychosocial factors evidently play a major role in a patient’s outcome, and the results of this study stress the importance of recognizing those patients which need further social support while going through the difficult process of autologous HCT. It also points to the importance of having well trained staff which can identify these patients and intervene on time. Future studies may prospectively focus on a larger cohort with a longer follow-up period in order to investigate the association between psychosocial factors and additional outcomes such as relapse and overall survival and to test further interventions to improve coping with the transplantation process.
Funding
None.
References
- T Philip, C Guglielmi, A Hagenbeek, R Somers, H Van der Lelie, et al. (1995) Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med 333(23): 1540-1545.
- Michaela Rancea, Bastian von Tresckow, Ina Monsef, Andreas Engert, Nicole Skoetz (2014) High-dose chemotherapy followed by autologous stem cell transplantation for patients with relapsed or refractory Hodgkin lymphoma: a systematic review with meta-analysis. Crit Rev Oncol Hematol 92(1): 1-10.
- Michele Cavo, S Vincent Rajkumar, Antonio Palumbo, Philippe Moreau, Robert Orlowski, et al. (2011) International Myeloma Working Group. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood 117(23): 6063-6073.
- E Frick, C Motzke, N Fischer, R Busch, I Bumeder (2005) Is perceived social support a predictor of survival for patients undergoing autologous peripheral blood stem cell transplantation? Psychooncology 14(9): 759-770.
- Jennifer M Knight, Jan A Moynihan, Jeffrey M Lyness, Yinglin Xia, Xin Tu, et al. (2014) Peri-transplant psychosocial factors and neutrophil recovery following hematopoietic stem cell transplantation. PLoS One 10: 9(6)
- Sanghee Hong, Lisa Rybicki, Donna Abounader, Brian J Bolwell, Robert Dean, et al. (2016) Association of Socioeconomic Status with Outcomes of Autologous Hematopoietic CellTransplantation for Multiple Myeloma. Biol Blood Marrow Transplant 22(6): 1141-1144.
- Knight JM, Syrjala KL, Majhail NS (2016) Patient-Reported Outcomes and Socioeconomic Status as Predictors of Clinical Outcomes after Hematopoietic Stem Cell Transplantation: A Study from the Blood and Marrow Transplant Clinical Trials Network 0902 Trial. Biol Blood Marrow Transplant 22(12): 2256-2263.
- Sanghee Hong, Lisa Rybicki, Donna Abounader, Brian J Bolwell, Robert Dean, et al. (2016) Association of Socioeconomic Status with Outcomes of Autologous Hematopoietic Cell Transplantation for Multiple Myeloma. Biol Blood Marrow Transplant 22(6): 1141-1144.
- Marina Davidov, Chava Perry, Yair Herishanu, Nadav Sarid, Esti Rom, et al. (2018) Toxicity and efficacy of autologous hematopoietic cell transplantation in elderly patients with aggressive lymphoma: a historical prospective study. Annals of Hematology 97(3): 459-466.
- Allen C Sherman, Stephanie Simonton, Umaira Latif, Thomas G Plante, Elias J Anaissie (2009) Changes in quality-of-life and psychosocial adjustment among multiple myeloma patients treated with high-dose melphalan and autologous stem cell transplantation. Biol Blood Marrow Transplant 15(1): 12-20.

 Research Article
Research Article