ABSTRACT
For decades, health practitioners and clinicians have been classifying people in different weight categories based on Body Mass Index (BMI) thresholds. This popular measurement, adopted by the World Health Organization (WHO), has been frequently criticized as having various deficiencies estimating obesity both for healthy and diseased populations. The main purpose of this study is to tackle this issue by proposing a new model of assessing BMI thresholds using the latest discoveries on:
a. Health risks, including COVID19, and mortality data;
b. The average of adiposity levels with the same BMI across different age and gender groups; and
c. The latest findings in the optimal timing for the brain control of weightpresetting (the fundamentals of the Lipostat theory).
This novel approach adapts WHO-defined BMI thresholds to novel calibrated thresholds by incorporating recently published multi-dimensional data from largescale worldwide studies. This novel WHO-readapted probabilistic BMI-based approach provides a more realistic weight categorization resulting in a new likelihood model of the health risks associated with adiposity. This new calibrated version of WHO-defined BMI thresholds sets up the bases for further experimental investigations aiming the application of personalized and preventive medicine, and successful long-term Weight and Health Management Programs. In addition to vaccination programs, this novel approach could be used as an “alternative method of prevention” to naturally tackle the current global situation of pandemic, and other anticipated in the future to come.
Abbreviations: BMI: Body Mass Index; WHO: World Health Organization; BF: Body Fat; HA: Healthiest Area
Introduction
The Body Mass Index (BMI) is the most frequently used method to measure adiposity and obesity in large epidemiological studies in both healthy and diseased populations. It was introduced by Adolphe Quetelet during the 19th century. Based on the data from the Seven Countries Study during the 70s [1], researchers found it as a good approximation for assessing adiposity and overweight related problems. The World Health Organization (WHO) estimates that more than 1.9 billion adults worldwide are overweight (BMI 25–<30), and over 650 million are obese (BMI ≥30) [2]. The worldwide prevalence of overweight and obesity is high and increasing [3]. The majority of articles reporting about the health risks of overweight and obesity have been limited to just a few. However, like in the -omics (disciplines in biology such as genomics, proteomics, metabolomics and glycomics), utilizing different multidimensional data sources could be the best and most efficient way to show the impact of complex biological processes in human health such as overweight and obesity. Recent large-scale analyses followed by a prolonged follow-up [4] indicate that underweight (BMI <18.5), overweight and obesity are associated with increased mortality, challenging previous studies [5]. This is consistent with 10 years of follow-up studies showing that the incidence of diabetes, hypertension, heart disease, colon cancer, and stroke increased with the degree of overweight [6].
Studies conducted during Coronavirus pandemics have shown that patients at risk for COVID19 have been characterized as having preexisting diseases, such as hypertension, cardiovascular disease, diabetes, chronic respiratory disease, or cancer [7]. And a recent study [8] has investigated the association between BMI, clinical characteristics, and the need for invasive mechanical ventilation in patients admitted to intensive care due to COVID19, suggesting that obesity may be also an independent risk factor for this rapidly spreading disease. Despite the wide use of BMI and its important health implications, this measurement is not perfect because it is only dependant on height and weight and it does not take into consideration different levels of adiposity based on age, physical activity levels, and gender. For this reason, the BMI has been frequently criticized as having various deficiencies as a measure of obesity both for healthy and diseased populations [9]. Furthermore, the BMI by itself can not anticipate any changes in weight category in the future, which can be one of the reasons why ~80% of people succeeding in short-term weight loss are not able to maintain it long term [10]. Successful weight management programs should also consider the required timing for feedback signals originating in adipose tissue to influence the brain centers that control eating behavior and activity (metabolic and motor), the fundamental of the Lipostat theory [11], which has been for the very first time studied in humans [12]. Despite all the above caveats, yet the BMI remains a widely used screening tool amongst health practitioners.
The last WHO actualization of BMI thresholds happened in 2004 [2]. The availability of newly published meta-data from various sources provide an opportunity for revisiting current adopted BMI thresholds. This study suggests a novel probabilistic approach consisting of WHO-readapted BMI thresholds aiming to accurately reflect the impact of:
1. Adiposity in disease and mortality rates [4,6], in order to readapt thresholds;
2. Race, gender, and age variables in adiposity [13], in order to diminish false positive and negative rates; and
3. The potential influence of the “Lipostat” in facilitating longterm weight-presetting, in order to allow probability BMI thresholds better associated with weight and health risks [12].
Methods
WHO-defined BMI thresholds were readapted by following a 3-steps procedure: BMI thresholds with the lowest health-risk(%) from the Global BMI Mortality project (from over 10 million people across 4 continents) [4], the Nurses’ Health (from 121,701 female registered nurses), and the Health Professionals Follow-up Studies (from 51,529 men) [6], the UK Biobank (from 22 research assessment centers in the United Kingdom) [14], and the Centre Hospitalier Universitaire de Lille, France (obesity frequency among 124 patients admitted in intensive care for SARS- CoV- 2) [8] were displayed on a Health-Risk vs BMI graph. The BMI thresholds with the lowest health risk from the Allied Dunbar National Fitness Survey (4,316 randomly selected healthy participants from different gender and age groups) [13] were used to readapt the overweight and obese BMI (averaged and rounded) thresholds and displayed on the graph. Finally, the probabilistic BMI thresholds from the first reported long-term human study [12] involving metabolic adaptation, weight-presetting (consistent with the Lipostat theory), and successful long-term weight loss were displayed on the graph.
Results
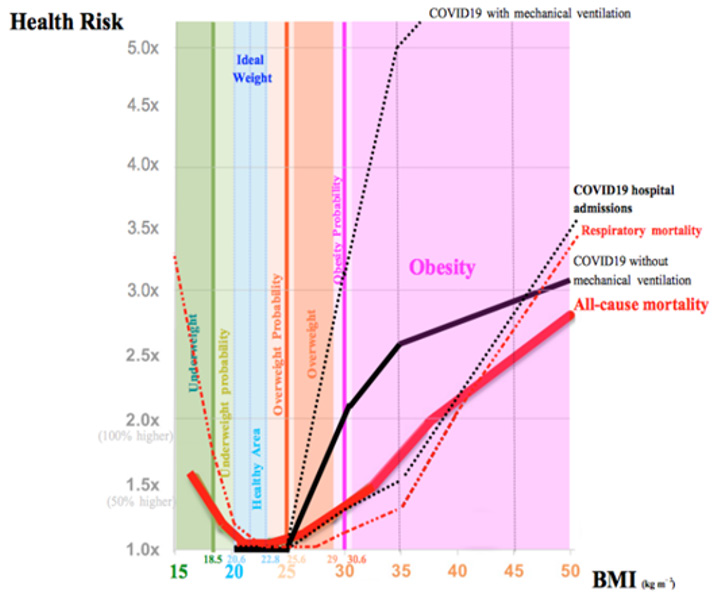
The weight relevance to disease, including COVID19 data, and mortality in different populations was assessed [4,6]. The novel WHO-readapted BMI thresholds take into account that having overweight increases mortality risk until 35-40%, compared to reference healthy individuals, and as much as 100% and until 3 times more than the reference in individuals with coronavirus disease, not requiring and requiring mechanical ventilation, respectively (Figure 1). Obesity is also a major risk factor, increasing mortality risk until 3 times more, compared to the reference, and until more than 3 times and more than 5 times in coronavirus patients, not requiring and requiring mechanical ventilation, respectively. Having underweight also increases the mortality risk to as much as 50% more than the reference, and, surprisingly, slightly in the BMI range 18.5-<20 (Normal BMI category), suggesting that both excessively and nearly lean adults should be also considered of health concern.
For underweight individuals, an estimation of mortality risk due to coronavirus is not currently possible due to lack of data but it was approximated by respiratory disease data (Figure 1). Having overweight and obesity increases the risk of type 2 diabetes, high blood pressure, heart disease, and other cancer diseases such as colon, breast, esophagus, gallbladder, pancreas, uterus, ovaries, kidney, and liver [5] (not shown for clarity). The relationship between BMI and the risk of developing chronic diseases is evident even among adults in the upper half of the BMI range 22.0-<25, considered as Normal category. This is consistent with recent studies suggesting a BMI between 18.5 and 21.9 minimizes the risk of high cholesterol, hypertension, type 2 diabetes, heart disease, stroke, and colon cancer [6]. However, a more recent study shows that there is a slightly increased mortality risk (13%) in the lower half of the Normal BMI range 18.5 - <20 compared to the reference [4]. Thus, the WHO-defined BMI thresholds were readapted (1st time) accordingly, based on mortality risk as this was considered the most important health parameter.
A recent study has anchored the overweight BMI threshold 25 for the 40–49 years old group, all other age group and gender differences estimated for the same BodyFat (BF)%=25.3 and 34.8 for all male and female participants, respectively. The same study anchored the obese BMI threshold 30 for the 40–49 years old group, all other age groups and gender differences estimated for the same BF%=34.1 and 43.5 for all male and female participants, respectively [13]. WHO-readapted BMI thresholds were further readapted (2nd time) by taking into account the changes in adiposity composition occurring in different age and gender groups (Figure 1). Finally, a study supporting the Lipostat theory in humans has shown “the healthiest area” (HA), a narrower area (20.6 - 22.8) of the WHO-defined Normal BMI thresholds (18.5<25), may represent a better BMI threshold and a healthier reference for long-term weight loss [12]. This was achieved by considering three novel probabilistic BMI thresholds to classify under-, over-weight, and obese. Interestingly, the lowest mortality risk overlapped HA and was not overlapping BMI thresholds of age and gender adiposity differences, supporting HA thresholds for successful long-term weight and health management programs. Thus, the WHOreadapted BMI thresholds were further readapted again to account for metabolic adaptation and weight-presetting. Altogether, this resulted in the final WHO-readapted (3rd time) BMI thresholds to assess the health risk associated with weight (Figure 1).
Note: The figure indicates the level of health risk (1x – 5x) with each 5-unit increase in WHO- defined BMI thresholds together with the readapted colored ones. Health risk (1.5x - 5.0x) represents the increase in health risk ratio (from 1.5 to 5 times) compared to reference healthy individuals (1x). Colour coding: Red lines = Global BMI Mortality data [4]; Black lines = UK Biobank [14] and SARS- CoV- 2 intensive care data [8] (other diseases not shown for clarity). Sub-lines are proportional to the information content. Newly proposed thresholds and probability color-coded areas (Green, orange, and pink) are calculated by taking into account the human Lipostat theory [12], the Global Mortality data, and the recently proposed redefinition of BMI thresholds [13]. Green, orange and pink lines = WHO-defined BMI thresholds for under-, over-weight, and obesity, respectively. “Ideal Weight” and blue lines are defined according to the lowest health risk of all-cause mortality.
Figure 1: The BMI as a predictor of disease.
Discussion
A low health risk occurs for individuals with a BMI 20-<25 (Normal BMI category). However, this study shows that the lowest mortality risk approximately occurs for individuals with BMI 20.6 - 22.8 (sky blue “Healthy Area”). Outside this BMI thresholds, there is an increased risk of diseases and mortality, and outside the Normal BMI thresholds, the risk of disease, including coronavirus, and mortality is more dramatic. It is estimated that if the WHO-defined Normal BMI thresholds, was applied to the world’s overweight and obese population, the proportion of premature deaths that could be avoided would be approximately 1/5 in North America, 1/6 in Australia & New Zealand, 1/7 in Europe, and 1/20 in east Asia, assuming that the associations of overweight and obesity with mortality mostly reflect causal effects. Nonetheless, if the novel WHO-readapted “Healthy” BMI thresholds were instead to be applied to the world’s overweight and obese population, the proportion of premature deaths would be higher. This novel approach also highlights how BMI thresholds act as a factor in COVID-19 severity. Thus, overweight and obese patients, especially severely obese, should take extra precautionary measures to avoid COVID- 19 contamination [8]. Since over 2/3 of the western society are overweight/obese, this potentially presents a major risk factor for severe COVID-19 infection and may have implications in governments policies [14]. Allowing age- and gender-specific BMI thresholds, this novel WHO-readapted approach reflects the same levels of adiposity, eventually reducing the number of false-positive and negative associated to wrong BMI categories [13].
Finally, including probabilistic BMI and HA thresholds provides additional advantages:
1. Predict new potential weight risks scenarios, such as under-, over-weight and obesity, and their associated health risks;
2. Reduce the rate of BMI misclassification; and
3. It is consistent with metabolic adaptation and weightpresetting (the Lipostat theory), allowing long term weight loss, and maintenance [12].
In summary, this study highlights the need for an adaptation and redefinition of the current WHO-BMI thresholds. The proposed novel approach is consistent with the up-to-date disease and mortality data, changes in adiposity composition, and time-based weight-presetting, providing a novel predictive dimension, with automation potential, to WHO-defined BMI thresholds. Due to the current stage of pandemic worldwide and the difficulties shown at accessing effective therapeutics, especially in poor economies, the “Healthy Area” proposed here could complement current vaccination programs, acting as “an alternative preventive measure”, without any secondary effects, for the prevention of COVID-19 and other diseases [4-8], and, ultimately, death by increasing life span. Given the time and cost estimate for the discovery and supply of new antiviral therapeutics (~10 years and US$500 million in average [15]), the “Healthy Area” proposed here could be achieved in a much shorter time (from weeks to months), even for the most extreme cases of obesity, and at no cost. An automatic web application [16] intuitively driving any individual into a customized “Healthy Area” has been created. A healthy weight by calorie restriction enhances healthspan (the length of time that an individual remains healthy) and increases longevity across species [17]. This study also suggest that even limited weight loss could improve the metabolic health of a person with overweight and obesity, reducing the chance of developing numerous diseases, something particularly important during pandemic times [4,6]. This study sets up the bases for the systematic implementation of efficient personalized and preventive medicine, and weight and health management programs. With sufficient funding, the results presented here can be tested and validated at a larger scale.
Acknowledgment
I thank I Peregrin-Alvarez, MD at Cleveland Clinic for reviewing this manuscript, helpful comments, and support.
Conflict of Interest
The author declares no conflict of interest.
References
- Keys A, Aravanis C, Blackburn H, Buzina R, Djordjević BS, et al. (1980) Seven Countries Study: a multivariate analysis of death and coronary heart disease. Cambridge, England: Harvard University Press.
- (2016) World Health Organization (2016) Obesity and overweight.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 384: 766-781.
- (2016) The Global Mortality Collaboration. Body-mass index and all-cause mortality: individual participant-data meta-analysis of 239 prospective studies in four continents. The Lancet 388: 776-786.
- Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309(1): 71-82.
- Field AE, Coakley EH, Must A, Spadano JL, Laird N, et al. (2001) Impact of Overweight on the Risk of Developing Common Chronic Diseases During a 10-Year Period. Arch Intern Med 161(13): 1581-1586.
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID- 19 in Wuhan, China: a retrospective cohort study. The Lancet 2020 395: 1054-1062.
- Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, et al. (2020) High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus- 2 (SARS- CoV- 2) Requiring Invasive Mechanical Ventilation. Obesity.
- Rothman KJ (2008) BMI-related errors in the measurement of obesity. Int J Obes 32(3): S56-59.
- Wing RR, Phelan S (2005) Long-term weight loss maintenance. Am J Clin Nutr 82: 222S 225S.
- Kennedy GC (1953) The role of depot fat in the hypothalamic control of food intake in the rat. Proc R Soc Lond B Biol Sci 140(901): 578-96.
- Peregrin Alvarez JM (2016) Self-experiencing the healthiest weight. J Obes Overweig 2: 304.
- Nevill AM, Metsios GS (2015) The need to redefine age- and gender-specific overweight and obese body mass index cutoff points. Nutrition & Diabetes 5(11): e186.
- Gale CR, Kivimäki M, Batty GD (2020) Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. PNAS 117(35): 21011-21013.
- Plotkin S, Robinson JM, Cunningham G, Iqbal R, Larsen S (2017) The complexity and cost of vaccine manufacturing – An overview. Vaccine 35(33): 4064-4071.
- One Click to Health web tool.
- Guijas C, Montenegro Burke JR, Cintron Colon R, Domingo Almenara X, Sanchez Alavez M, et al. (2020) Metabolic adaptation to calorie restriction. Science Signaling 13(648): eabb2490.

 Mini Review
Mini Review