Abstract
Primary idiopathic intracranial hypertension (IIH), previously termed pseudotumor cerebri, is characterized by an elevated cerebrospinal fluid pressure of no identified cause. IIH is essentially a diagnosis of exclusion, suspected by clinical signs and supported by imaging findings with additional tests to rule out secondary causes of raised intracranial pressure. IIH occurs mainly in adults and may also be found in adolescents. Data on IIH in children remain sparse. The aim of this report was to describe the clinical picture and outcome of 5 young children (age <1-4 years) who presented to our tertiary medical center with various complaints and were found on comprehensive evaluation to have IIH. We found that IIH in this age group poses a diagnostic challenge. It often has a different clinical picture from adult IIH, follows a more complicated course, and responds poorly to treatment with Acetazolamide. Larger prospective studies are needed.
Keywords: Idiopathic Intracranial Hypertension; Pseudotumor; Papilledema; Toddlers
Abbreviations: IIH: Idiopathic Intracranial Hypertension; CSF: Cerebrospinal Fluid; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; LP: Lumbar Puncture; INR: International Normalized Ratio; ANA: Antinuclear Antibody Test; VP: Ventriculo- Peritoneal; OCT: Optical Coherence Tomography; EVOH: Extraventricular Obstructive Hydrocephalus
Introduction
Idiopathic Intracranial Hypertension (IIH), previously termed pseudotumor cerebri or benign intracranial hypertension, is characterized by an increase in intracranial pressure of no identified cause. It occurs predominantly in adults, particularly young overweight women of childbearing age. The overall annual incidence is 2.4 per 100,000 [1]. IIH is essentially a diagnosis of exclusion, suspected by clinical signs and normal findings on imaging studies, in accordance with the revised modified Dandy criteria, with additional tests to rule out secondary causes of raised intracranial pressure (brain parenchymal lesion, vascular malformations, hydrocephalus, central nervous system infections etc). IIH is rare in children and adolescents, with an estimated reported incidence of 0.5 per 100,000 [2]. Studies in this age group have found that the most common presenting symptom of IIH is headache, documented in up to 91% of cases [3]. Nausea and vomiting may occur as well, and less often, blurred, or double vision, transient visual obscurations, tinnitus, and neck stiffness [4]. In younger patients, IIH may present only with irritability [5]. The diagnostic process follows that in adults. In children, a cerebrospinal fluid (CSF) opening pressure of ≥25 cmH2O is diagnostic of IIH; in obese or sedated children, the cutoff is ≥28 cmH2O [6].
The specific incidence and clinical picture of IIH in very young children has rarely been reported. In Schneider Children’s Medical Center of Israel, children admitted with papilledema undergo an ophthalmic examination by a neuro-ophthalmologist and imaging, usually Magnetic Resonance Imaging (MRI) or, if unfeasible, Computed Tomography (CT). If findings on physical examination and imaging are normal and IIH is suspected, the children are referred for Lumbar Puncture (LP) under sedation. To exclude secondary causes of increased intracranial pressure the following blood parameters are tested: complete blood count, chemistry and electrolyte levels, C-reactive protein level, blood gases, thyroid stimulating hormone level, International Normalized Ratio (INR), Antinuclear Antibody Test (ANA), and vitamin A and D levels. The aim of this report was to describe the clinical course and outcome of 5 children from 10 month to 3 years and 9 month who were diagnosed with IIH.
Methods
This study was approved by the Institutional Review Board of Schneider Children’s Medical Center of Israel. The hospital’s healthcare database was reviewed for all children aged 3 years or less who were diagnosed with IIH from 2013 to 2020, and their clinical and laboratory data were extracted.
Results
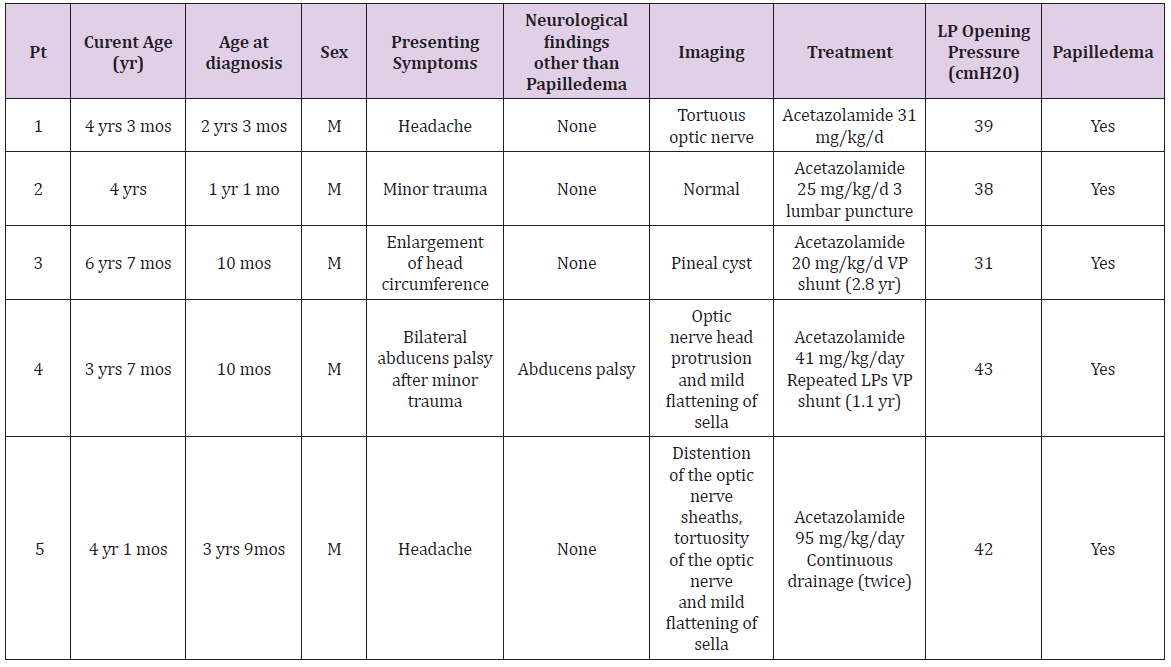
Five young children diagnosed with IIH were identified. Their clinical characteristics are summarized in Table 1 and their clinical course is described below.
Case 1
A boy aged 2 years and 3 months presented to the emergency department with his parents who explained that they had recently caught the child grabbing his head during activities or while running and they suspected he might be having headaches. His body temperature was normal, and he was not waking up or vomiting during the night. They denied any use of medications including vitamins. The child’s medical history was remarkable for the diagnosis of autistic spectrum disorder. Physical examination including neurological examination was normal, albeit finding bilateral papilledema on ophthalmic examination prompted evaluation with MRI+Magnetic Resonance Venography (MRV) which demonstrated tortuosity of the optic nerve. Based on a working premise of IIH, LP was performed. Opening pressure was 39 cmH2O with no cells. A regimen of Acetazolamide 21 mg/kg/day was started. When the child’s symptoms failed to resolve and the parents complained of new onset of arousals in the early morning hours, the dose was increased to 31 mg/kg/day. Treatment was continued for one year under ophthalmologic and neurologic follow-up until resolution of symptoms. The child is currently 4 years and 3 months old and has no complaints of headache or visual problems.
Case 2
A boy aged 1 year and one month presented to the emergency department with minor head trauma near the orbit. Physical and neurologic examinations were unremarkable, but ophthalmic examination revealed asymptomatic bilateral papilledema which prompted a referral to complete head CT, with normal findings. LP was performed, with an opening pressure of 38 cmH2O. A diagnosis of IIH was made, and treatment with Acetazolamide 25 mg/kg/day was started. To complete the evaluation, MRI+MRV was performed along with blood tests to rule out secondary causes of increased intracranial pressure, in accordance with the hospital protocol. The only remarkable finding was normocytic anemia, with hemoglobin 9.5 g/dl, normal ferritin level, and low iron levels, which was treated with oral iron supplementation. The papilledema failed to improve, and two more LPs were performed. Acetazolamide treatment was continued for 2 years. Other than a language delay, development was normal. The child is currently 4 years old and is undergoing genetic evaluation for suspected skeletal dysplasia. On continued biannual ophthalmologic follow-up, the optic disc is normal, and the patient denies any headaches or visual deficits.
Case 3
A 10-month-old otherwise healthy boy with normal development was admitted to the pediatric ward for evaluation of an increase in head circumference to 95% from 50% at birth. The child was born at 34 weeks’ gestation after a normal pregnancy and delivery. Immediately after delivery, he was admitted to the neonatal intensive care unit because of hypocalcemia and hypomagnesemia which were corrected orally. Developmental milestones were achieved with no delay. There were no prior hospitalizations. His parents denied any medications except for iron and vitamin D according to the recommendations of the Israeli Pediatric Health Association. Findings on physical and neurologic examinations where within normal limits, except for head circumference at the 95th percentile with frontal bossing. There were no hemodynamic signs of increased intracranial pressure. Fundoscopic examination revealed bilateral papilledema. MRI of the whole neuroaxis showed no abnormalities except for an incidental finding of a small pineal cyst. LP was performed, with opening pressure 24 cmH2O. Despite the borderline pressure, because of the finding of papilledema, treatment with Acetazolamide 15 mg/kg/day was started. Blood tests performed according to our protocol to identify secondary causes of increased intracranial pressure were negative. When the papilledema failed to improve, two more LPs were performed, with opening pressures of 27 and 31 cmH20, and the Acetazolamide regimen was increased to 20 mg/kg/day. Nevertheless, the papilledema still did not improve. At age 2.8 years, following multidisciplinary consultation, the patient was referred for insertion of a Ventriculo-Peritoneal (VP) shunt. The procedure was uneventful. Postoperative follow-up revealed normalization of the optic nerve width on ultrasound and normal visual acuity. The child is currently 6 years and 7 months old and has no headaches or visual complaints.
Case 4
A 10-month-old otherwise healthy boy with normal development presented to the emergency department for evaluation of a minor head trauma sustained when he fell backwards. His parents reported that he began vomiting but did not lose consciousness. Findings were normal or negative on neurologic examination, abdominal ultrasound to rule out intussusception, and fundoscopic examination. The patient was treated with fluids and antiemetics for 2 days and discharged home. The next day, the patient again presented to the emergency department because of 4-5 episodes of vomiting and new-onset strabismus. Neurologic examination revealed bilateral abducens palsy, and fundoscopic examination demonstrated bilateral papilledema. Head CT with contrast was normal, MRI+MRV+MRA (magnetic resonance angiography) showed mild changes characteristic of IIH (Table 1). On the working premise of IIH, LP was performed, with opening pressure 43 cmH2O. Detailed laboratory investigation for secondary causes of increased intracranial pressure according to our protocol was negative. Treatment with Acetazolamide was started. When the ophthalmic findings failed to improve, the dose was increased to 41 mg/kg/day concurrent with repeated LPs until opening pressure decreased to 23 cmH2O. Three months after discharge, the child returned to the emergency department after falling from a toy car while his brother fell on his head.
His parents reported that he vomited 8 times. On presentation, the neurologic examination revealed no abnormalities other than an increase in head circumference from the 50th percentile 2 months previously to the 97th percentile. Head CT without contrast demonstrated bilateral subdural collections which had not been found on the MRI scan performed 3 months previously. Ophthalmic examination demonstrated papilledema with no deterioration from the last follow-up but with new bilateral retinal bleeding. These findings prompted a skeletal survey to rule out non-accidental injury, a metabolic survey to rule out metabolic disturbances that may present with a similar picture (e.g., glutaric aciduria), and hematologic evaluation to rule out bleeding disorders. No abnormalities were found. After consultation with neurosurgeons, the child (now 1 year and 1 month old) was referred to bilateral subduro-peritoneal shunt insertion. This led to improvement in the ophthalmologic parameters and stepwise resolution of the subdural collections. At age 2 years, MRI showed complete resolution of the subdural collections, and the shunts where removed. The child is currently 3 years and 7 months old, healthy, with normal development.
Case 5
An otherwise healthy boy aged 3 years and 9 months presented to the emergency department complaining of headache. According to his parents, the headache had started 2 weeks before and was located frontally bilaterally, without nausea or vomiting, visual disturbance, or night arousal. The headaches had initially resolved without treatment, but lately, paracetamol was needed to reduce the pain. Neurologic examination was unremarkable, except for fundoscopic examination that revealed bilateral papilledema. MRI+MRV+MRA yielded findings characteristic of IIH (Table 1). Opening pressure on LP was 34 cmH2O. Detailed laboratory investigation for secondary causes of increased intracranial pressure according to our protocol was negative. Acetazolamide 20 mg/kg/day was started, leading to resolution of the headaches and improvement in the papilledema. Two month later, on ophthalmologic follow-up, Optical Coherence Tomography (OCT) demonstrated worsening of the papilledema. A second LP was performed, with opening pressure 42 cmH2O, and the Acetazolamide dose was gradually increased gradually to 38 mg/kg/day. When the papilledema failed to resolve, the multidisciplinary team recommended insertion of a continuous drainage tube for 5 days. Opening pressure was 32 cmH2O.
OCT initially showed improvement, but 5 days after the intervention, worsening of the papilledema was noted on OCT and ultrasound of the optic nerve, and the Acetazolamide regimen was gradually increased to 95 mg/kg/day, with no side effects, except for a lactic acidosis with PH- 7.27 and HCO3-18, that was treated with sodium bicarbonate. Ophthalmologic follow-up with OCT demonstrated injury to the optic nerve. A team of pediatric neurologists, neurosurgeons and an ophthalmologist decided to hold off on a VP shunt and referred the child for a second continuous drainage for a longer period. Opening pressure was 29 cmH2O, with an improvement in signs. However, after 6 days, the drain was removed due to the appearance of Staphylococcus haemolyticus meningitis which was treated with vancomycin. At the end of the child’s hospitalization, partial improvement was noted on OCT, and on follow-up 2 months later, at age 4 years and 1 month, fundoscopic examination showed marked improvement.
Discussion
The present report describes the clinical course of 5 young children (aged 10 months-3 years and 9 month) diagnosed with IIH. IIH is a rare neurologic disorder in children. Studies of affected adults and adolescents reported a background of obesity or intake of medications. However, the literature does not show any risk factors in children. The children in our series underwent comprehensive workup to rule out possible secondary causes of IIH, and all findings were normal or negative. The most common presenting symptom of IIH in children is headache [3], followed by nausea, vomiting, and visual disturbances [4]. In a summary of 26 cases of infantile IIH, Boles, et al. [7] found that the most prevalent symptoms were bulging fontanelle, irritability, vomiting, and cranial nerve palsies. In our series, the two older children (aged more than 2 to nearly 4 years) presented with headache; in the others, IIH was an incidental finding on evaluation of increasing head circumference in one child and minor head trauma in 2 children. It is noteworthy that only one of the children, with abducens palsy after minor head trauma, had abnormal neurologic signs at presentation. Brain imaging in cases of IIH should be normal, with an absence of signs of secondary causes of increased intracranial pressure. Owing to ongoing advances in neuroimaging techniques, however, subtle findings suggestive of IIH have emerged, such as empty sella, flattening of the posterior globes, optic nerve head protrusion, distension of the optic nerve sheaths, tortuosity of the optic nerve, cerebellar tonsillar herniation, meningoceles, CSF leaks, and transverse venous sinus stenosis [8].
In our study, 3 of the 5 children had an MRI finding suggestive of IIH. IIH is a neurologic emergency, as it can result in irreversible deficits in visual acuity and cranial nerve palsies due to mechanical compression of the optic nerve [9]. Therefore, prompt treatment is needed. There are no current studies of treatment or treatment guidelines in the pediatric population. Adult data suggest that Acetazolamide is an acceptable first-line medication at dosages of 15- 20 mg/kg/day. A single-center study showed that less than 10% of children either fail to respond to pharmacological treatment or cannot tolerate it and therefore require surgical intervention, such as serial LP, optic nerve sheath fenestration, and insertion of a VP shunt [10]. In another study, Hacifazlioglu Eldes, et al. [11] found that among 12 cases of intracranial hypertension in children, 6 were idiopathic and 6 were attributable to secondary causes. Two children in the latter subgroup, with sinus vein thrombosis, required a VP shunt, and 4 were treated with medications and LPs [11]. At present, there is insufficient available evidence to recommend or reject any of the surgical treatment modalities for IIH [12]. In contrast to these previous reports [10,11], children in our study needed increasing doses of Acetazolamide (20- 95 mg/kg/day). Four children (80%) did not respond well to medical therapy and required invasive intervention with continuous drainage, LP (all children; more than one in 4), or VP shunt (2 children).
These findings suggest that the IIH may follow a complicated course in very young children. Data on the outcomes of VP shunts in patients with IIH are variable. Some authors reported stabilization or remission of visual problems in 95-100% of cases whereas others found that vision continued to worsen in approximately 10% of cases [10,13,14]. In our study, visual acuity was preserved in all children. Extraventricular Obstructive Hydrocephalus (EVOH), defined as an imbalance between excessive production and lesser absorption of CSF, is a fairly common neuroimaging finding in young children [15]. Therefore, it is possible that the severe clinical course of IIH in the toddler age group is a consequence of superimposed pressures on a baseline state of excessive pressure within the skull. Some of the patients in our small cohort were asymptomatic, and papilledema was found incidentally on eye examination. Lee, et al. [16] retrospectively reviewed the medical charts of 1110 adult patients with optic atrophy and found that in 6.5%, isolated unexplained optic atrophy was noted on neuroimaging. Untreated IIH may result in optic atrophy, and pediatric IIH that remains undiagnosed might lead to unexplained optic atrophy in adulthood. Therefore, this study provides a practical guideline to clinicians to perform a routine neurological examination in young children.
Conclusion
The present retrospective case series adds to the limited available data on IIH in children under 5 years of age. The course of the disease was not as benign as the former name of this disorder suggests. The clinical presentation in children can be variable and less obvious than in adults. The diagnosis of papilledema can be challenging. In the absence of randomized controlled studies, evidence-based recommendations for the management of IIH in children cannot be made. Further prospective studies are needed to clarify and consolidate management approaches in this patient population.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None.
References
- Kilgore A V, Lee M S, Leavitt J A, Mokri B, Hodge D O, et al. (2017) Re-evaluating the incidence of idiopathic intracranial hypertension in an era of increasing obesity. Ophthalmology 124: 697-700.
- Tibussek D, Distelmaier F, Von Kries R, Mayatepek E (2013) Pseudotumor cerebri in childhood and adolescence-results of a Germany-wide ESPED-survey. Klin Padiatr 225(2): 81-55.
- Aylward S C, Waslo C S, Au J N, Tanne E (2016) Manifestations of pediatric intracranial hypertension from the Intracranial Hypertension Registry. Pediatr Neurol 61: 76-82.
- Phillips P H, Repka M X, Lambert S R (1998) Pseudotumor cerebri in children. J AAPOS 2: 233-238.
- Spennato P, Ruggiero C, Parlato R S, Buonocore M C, Varone A, et al. (2011) Review pseudotumor cerebri. Childs Nerv Syst 27: 215-235.
- Friedman D I, Liu G T, Digre K B (2013) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 81(13): 1159-1165.
- Boles S, Martinez Rios C, Tibussek D, Pohl D (2019) Infantile idiopathic intracranial hypertension: a case study and review of the literature. J Child Neurol 34(13): 806-814.
- Bidot S, Saindane A M, Peragallo J H, Bruce B B, Newman N J, et al. (2015) Brain imaging in idiopathic intracranial hypertension. J Neuroophthalmol 35(4): 400-411.
- Distelmaier F, Tibussek D, Schneider D T, Mayatepek E (2007) Seasonal variation and atypical presentation of idiopathic intracranial hypertension in pre-pubertal children. Cephalalgia 27(11): 1261-1264.
- Fonseca P L, Rigamonti D, Miller N R, Subramanian P S (2014) Visual outcomes of surgical intervention for pseudotumour cerebri: optic nerve sheath fenestration versus cerebrospinal fluid diversion. Br J Ophthalmol 98(10): 1360-1363.
- Hacifazlioglu Eldes N, Yilmaz Y (2012) Pseudotumour cerebri in children: etiological, clinical features and treatment modalities. Eur J Paediatr Neurol 16(4): 349-355.
- Standridge S M (2010) Idiopathic intracranial hypertension in children: a review and algorithm. Pediatr Neurol 43(6): 377-390.
- Feldon S E (2007) Visual outcomes comparing surgical techniques for management of severe idiopathic intracranial hypertension. Neurosurg Focus 23(5): E6.
- Johnston I, Besser M, Morgan M K (1988) Cerebrospinal fluid diversion in the treatment of benign intracranial hypertension. J Neurosurg 69(2): 195-202.
- Abu Kuwaik G, Abu Kuwaik F, Laughlin S, Mac Gregor D, Moharir M, et al. (2015) 197: Neurodevelopmental status of children with macrocephaly and extraventricular obstructive hydrocephalus (EVOH) at presentation. J Paediatr Child Health 20(5): e104.
- Lee A G, Chau F Y, Golnik K C, Kardon R H, Wall M, et al. (2005) The diagnostic yield of the evaluation for isolated unexplained optic atrophy. Ophthalmology 112(5): 757-759.

 Case Report
Case Report