ABSTRACT
Non-degenerative primary dysautonomia is a pathology with imprecise compensatory responses from the central regulatory centers to the autonomous nervous system, very often in the population of all ages worldwide. Unfortunately, it is not addressed from a comprehensive point of view due to the ignorance of both: the health group professionals and the patients, so the multiple signs and symptoms (syncope, dizziness, paraesthesia, dyspnea, insomnia, palpitations, constipationdiarrhea, fatigue, headache, sweating, mood disorders, chest tightness) are seen from different angles, that is, fractionated and labeled with different diagnoses, so that patients are assessed and treated by multiple medical specialties, for many years with poor or medium results, causing frustration, stress, negative impact on quality of life and the development of comorbidities. A review of the subject is carried out, for dissemination and comprehensive knowledge of the pathology and in the area of Otorhinolaryngology it can be taken into consideration as a differential diagnosis within the dizziness pathology.
Keywords: Primary Dysautonomia; Treatment; Dizziness
Introduction
Non-degenerative primary dysautonomia is a pathology with a physiology of integration of inaccurate responses between the central nervous system and the autonomic nervous system, frequent in the population of all ages worldwide, unfortunately with a lack of precise prevalence numbers since it presents with a variety of signs and symptoms that are sometimes vague, unspecific and confusing (dizziness, syncope, paresthesias, dyspnea, insomnia, palpitations, constipation-diarrhea, fatigue, headache, sweating, mood changes, chest tightness), which means that it is not fully addressed, being fragmented by different medical specialties and from the health area: otorhinolaryngologists, cardiologists, endocrinologists, gastroenterologists, neurologists, pediatricians, pulmonologists, psychiatrists, internists and without forgetting nutritionists, all of this directly affects the delay in diagnosis, non-specific therapy and poor prognosis with the development of comorbidities, causing frustration, stress, and negative impact on the quality of patient’s lives.
Theoretical Framework
Generalities
A. Definition
During the bibliographic review, different definitions were evidenced, but the majority agreed that it is a pathology where inaccurate of compensatory responses are presented from the central regulatory centers (bulbar vasomotor centers and superior nervous centers controlling the vasomotor center), towards the autonomic nervous system [1].
B. Terms and Nomenclature with which it is Cited in the Literature
As mentioned above and it became clear during the literature review, primary non-degenerative dysautonomia has been labeled under different terms such as: vertiginous syndrome, migraine, irritable bowel syndrome, gallbladder dyskinesia, fibromyalgia, chronic fatigue syndrome, anemia syndrome, hypoglycemia, irritable bladder, mitral valve prolapse syndrome, orthostatic hypotension, [2,3] among many others, resulting in confusing conceptualization, since the nomenclature is frequently selected based on the predominant symptomatology at the time of diagnosis of the disease patient, without thinking of a comprehensive approach to pathology. In relation to the synonyms used and with which the pathology is frequently confused, we have vertigo, which always refers to an alteration of the vestibular system (housed in the inner ear and whose neurological center is in the brainstem), while the dizziness is a balance disorder not always related to it, within the vertiginous pathology of the Otorhinolaryngology area, Benign Paroxysmal Postural Vertigo, is a common pathology, where in 50% or more of the cases no etiology is found, so we could consider being facing Dysautonomia [4] The pathology is also labeled as migraine, which is a chronic disorder of the nervous system, characterized by the appearance of typical and recurrent episodes of headache, which are usually associated with nausea, vomiting, photophobia and sonophobia [5].
We will also mention irritable bowel syndrome, currently defined based on the modified Rome criteria, as the manifestation of abdominal discomfort or pain for at least 12 weeks (not necessarily consecutive) in the last 12 months, which cannot be explained due to structural or biochemical abnormalities, and having at least two of the following three characteristics: the pain ceases after defecation, its onset is associated with a change in the frequency of bowel movements or a change in the defecation form [6]. For its part, we know that gallbladder dyskinesia corresponds to a gallbladder motility disorder, which manifests clinically with nausea, vomiting or both, pain in the right upper quadrant that can radiate to the right intrascapular region. This disease is diagnosed with a gallbladder scintigraphy [7] and is also confused with dysautonomia. Regarding fibromyalgia, considered a synonym for several symptoms in common, we will mention that it is a syndrome characterized by diffuse, chronic musculoskeletal pain, of nonarticular origin, which is usually accompanied by insomnia, fatigue, morning stiffness and cognitive alterations, with a neurobiological pathophysiology [8].
Chronic Fatigue Syndrome has often been used synonymously and is clinically distinguished by persistent or recurrent debilitating fatigue for more than six months in the absence of any other identifiable medical cause. From 40 to 90% of patients with chronic fatigue syndrome report syncope or dizziness and symptoms of orthostatic intolerance such as disabling fatigue, dizziness, decreased concentration, tremor and nausea [9]. For its part, we know that the anemic syndrome refers to the decrease in hemoglobin content or the number of red blood cells due to blood loss or to the alteration in the production or destruction of the erythrocytes themselves. The clinical expression of this syndrome is the result of tissue hypoxia and its specific signs and symptoms represent compensatory cardiovascular responses depending on the severity and duration of hypoxia [10]. With regard to hypoglycemia, the most correct definition corresponds to the presence of neuroglycopenic or adrenocholinergic symptoms coinciding with low capillary or plasma glucose (around 50 mg/dl) and disappearance of symptoms when blood glucose increases, which causes symptoms as diverse as tachycardia, palpitations, tremors, paleness, anxiety, sweating, nausea, hunger, dizziness, headache, weakness, blurred vision, decreased ability to concentrate, confusion, decreased level of consciousness, diplopia, seizures, behavioral disturbance, aggressiveness, incoherent conversation, delirium, among others [11]. As we can see, many of these symptoms coincide with those of Dysautonomia, but the pathophysiology is totally different. Irritable bladder, also considered a synonym, was defined in 2002 by the International Continence Society as an overactive or irritable bladder syndrome, characterized by the presence of micturition urgency alone or in combination with other symptoms, such as urge incontinence, generally associated to an increase in micturition frequency and nocturia, in the absence of other demonstrable disease, therefore it is considered a syndrome with symptoms corresponding to the filling of the lower urinary tract [12].
If we define mitral valve prolapse as the herniation of one or both mitral leaflets, usually the posterior one, into the left atrium during systole, causing frequent symptoms such as fatigue, palpitations, dyspnea, and nonspecific chest pain [13], that coincide with those presented by patients with Dysautonomia, we can understand, because these pathologies are often considered synonymous. In relation to orthostatic hypotension, whose definition corresponds to a decrease in systolic blood pressure of 20 mm Hg or diastolic blood pressure of 10 mm Hg, during the passage to the standing position, and with frequent association of arterial hypertension, we can understand why It is often considered synonymous with Dysautonomia, but the big difference is that in the second there is no history of arterial hypertension [14]. From the above, we can evidence the coincidence of Dysautonomia symptoms with those of different pathologies, but with a totally different pathophysiological origin, which explains the confusion and misdiagnosis from the initial stages.
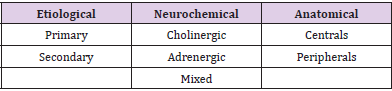
C. Classification
Dysautonomia’s are classified according to the etiology, the deficient neurotransmitter or the anatomical distribution of the affected neurons (Table 1).
1) Etiological Classification
Primary and secondary dysautonomia.
a) Primary of unknown etiology or idiopathic: characteristically, central or peripheral autonomic neurons, or both, exhibit imprecise compensatory responses from central regulatory centers to the autonomic nervous system without apparent cause, where central autonomic neurons, peripheral autonomic neurons, or both can even degenerate or die, for example, as in Parkinson’s disease.
b) Secondary: when it is the result of a disease that affects the autonomic fibers secondarily, for example, in diabetes or amyloidosis.
2) Neurochemical Classification
Cholinergic, adrenergic and mixed dysautonomia.
a) Cholinergic: Acetylcholine is the deficient neurotransmitter. Acetylcholine was one of the first neurotransmitters characterized both in the peripheral nervous system and in the central nervous system only in mammals, and participates in the regulation of various functions such as: activation phenomena of the cerebral cortex, the circadian cycle, memory, association, and higher-order thinking, among others. It is synthesized from choline, which is a dietary quaternary amine important for cell membrane integrity, neurotransmission, signaling, intracellular transport and lipid metabolism. Foods rich in choline, in addition to eggs, are liver, soybeans, meat, milk and peanuts. Acetyl - CoA also participates in the formation of acetylcholine, being a crucial intermediate molecule for various metabolic pathways of both lipids and proteins and carbohydrates. Its main functions include transferring the acetyl group to the Krebs cycle and it participates in the synthesis of acetylcholine, through a reaction catalyzed by choline acetyltransferase. There are mechanisms that precisely regulate the synthesis and release of acetylcholine, which acts on two types of receptors: ionotropic (nicotinic) and metabotropic (muscarinic) coupled to G proteins. Muscarinic receptors: M1, M2 and M3 are involved with the production of the second messenger cAMP. The M2 and M4 receptors inhibit the formation of cAMP, activate K+ channels and reduce Ca++ ion entry through voltagedependent channels, effects mediated by G proteins (Gαi and Gαo) [15]. Acetylcholine receptors are widely distributed in various areas of the central and peripheral nervous system and are responsible for the various physiological actions of acetylcholine. Its study has generated great interest, because various alterations in cholinergic transmission have been related, directly or indirectly, to severe disorders such as Alzheimer’s and Parkinson’s disease.
b) Adrenergic: Amines are the deficit neurotransmitter. Amines or catecholamines are a group of compounds that have the catechol group in their chemical structure , among the most important are adrenaline, noradrenaline and dopamine. They are synthesized from tyrosine, this amino acid can be derived directly from the diet or be synthesized in the liver from the amino acid phenylalanine. Foods rich in tyrosine are for example: meat, fish, dairy, eggs, vegetables, legumes, brown rice, seeds, whole grains, apples, asparagus, avocados, carrots, romaine lettuce, spinach, soy products, watermelon, cucumber, parsley, watercress, among others. Tyrosine enters chromaffin cells (or neurons if we are talking about the nervous system) through active transport. Adrenaline or epinephrine is synthesized and stored in the adrenal medulla and also in peripheral sympathetic nerves and released into the systemic circulation. Dopamine is found in the adrenal medulla and peripheral sympathetic nerves, but it acts primarily as a neurotransmitter in the central nervous system. Catecholamines participate in the integration mechanisms of both the central nervous system and the endocrine system. Therefore, the sympathetic nervous system and the adrenal medulla make up an anatomical and physiological unit, known as the sympathoadrenal system. This system plays a fundamental role, together with the hypothalamic-pituitaryadrenal axis, in responses to stress or injury [16].
c) Mixed when cholinergic, adrenergic, serotonergic are imprecise neurotransmissions [17,18]. Serotonin is a neurotransmitter with very important functions at the neuronal level, it regulates mood and behavior, prevents depression, anxiety and intervenes in sleep disorders. Low serotonin levels have been associated with hyperalgesia, aggression, depression and anxiety, and even the development of migraines, because when serotonin levels drop, blood vessels dilate. It is formed from tryptophan, an amino acid contained in eggs, milk, fish, meat and whole grains [19].
3) Anatomical Classification
Central and peripheral dysautonomia.
According to the anatomical distribution of the affected neurons.
a) Central: The affected neurons are preganglionic.
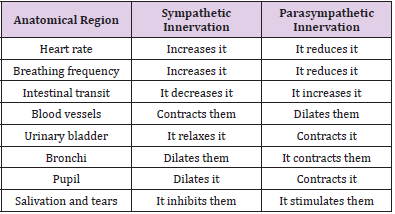
b) Peripheral: The affected neurons are ganglionic or postganglionic. It is worth mentioning that the cell body of the preganglionic neurons of both the sympathetic and parasympathetic divisions of the autonomic nervous system is located in the central nervous system (spinal cord or brain stem), and its axons synapse with the postganglionic neurons of the autonomic ganglia. These postganglionic neurons are autonomic nerve fibers from the ganglion to the effector organ (Table 2). In the previous table, a summary of the three classifications of Dysautonomies previously presented is presented.
Table 2: Synthesis of the activity of the sympathetic and parasympathetic nervous system in different anatomical regions [46].
D. Epidemiology
Dysautonomia are reported worldwide, whose most common symptoms are tachycardia, dizziness, syncope, weakness or fatigue, cognitive difficulty and blurred vision, presenting at any age [20]. In relation to syncope, which is only one of the multiple signs and symptoms of the disease, it is mentioned worldwide that approximately 37% of people suffer from it at least once in their life and 10% of adults present them recurrently, it is believed to be responsible for 3% of hospitalizations and 6% of visits to the emergency department, presenting more frequently in young women than in men. Most reports focus on relatively select populations such as the military, senior care facilities, or primary care outpatient clinics. For example, follow-up of 3,000 US Armed Forces individuals (mean age 29 years) revealed that 27% had experienced a syncopal episode during their lifetime. Extrapolation of these findings to medical practice is limited not only by the nature of the setting in which the research was conducted, but also by the variable manner in which symptoms were assessed [21]. If we add to the previous statistics the variety of symptoms that the disease, we can dimension the pathology. Dysautonomia is common at all ages, as seen in medical consultation, in Mexico it is estimated that it affects 10% of the teenagers. If we refer to epidemiology in relation to the prevalence of syndromes, is displayed:
a) Chronic Fatigue Syndrome: This syndrome is clinically distinguished for persistent or recurrent debilitating fatigue for more than six months in the absence of any other identifiable medical cause. From 40 to 90% of patients with chronic fatigue syndrome report syncope or dizziness, and symptoms of orthostatic intolerance such as disabling fatigue, dizziness, decreased concentration, tremor and nausea [9]. Irritable bowel syndrome: currently defined based on the modified rome criteria, as the manifestation of abdominal discomfort or pain for at least 12 weeks (not necessarily consecutive) in the last 12 months, which cannot be explained by structural abnormalities or biochemical, and having at least two of the following three characteristics: the pain ceases after defecation, its onset is associated with a change in the frequency of bowel movements or a change in the form of bowel movements [6]. In Mexico, it is reported that 93% of patients affected by the syndrome are women and although there are no adequate epidemiological studies, it was determined that the syndrome has an approximate prevalence of 16 to 21% among the population. The age of onset can vary from 17 to 53 years [22,23]. Benign paroxysmal positional vertigo is the most common entity within vertigo of peripheral origin. It is characterized by attacks of vertigo triggered by positional changes of the head and of short duration. It usually occurs in people over 40-50 years of age, and up to 50% of cases are not due to a known cause, which is why it is called idiopathic benign paroxysmal positional vertigo [4].
Physiology and Pathophysiology
Physiology of the Autonomic Nervous System: The autonomic or vegetative nervous system is an important component of the nervous system, made up of a complex set of neurons and nerve pathways that control the function of the different visceral systems of the body. Its global function is to maintain the state of homeostasis of the organism and carry out adaptation responses to changes in the external and internal environment. It is made up of three efferent components sympathetic, parasympathetic and enteric– innervates the heart muscle, the smooth muscle of all organs and the exocrine and endocrine glands. Thus, it regulates respiration, circulation, digestion, metabolism, glandular secretion, body temperature, reproduction and, in addition, coordinates all these vital functions to maintain body homeostasis (Table 2). It is not subject to voluntary or conscious control. The sympathetic nervous system plays a fundamental role in the integrity of the organism, since in a very fast and effective way, it emits a response to external stimuli that can threaten the integrity of the individual and for its part the parasympathetic function is oriented, contrary to that of the sympathetic, to the conservation of energy and system reset. The table above shows the participation of the two main branches of the autonomic nervous system and their influence on different anatomical regions. For example, normally 25% of the circulating blood volume is in the chest; once the upright position is assumed, gravity produces a sudden downward movement of 500 ml of blood towards the abdomen and lower limbs; approximately 50% of this volume is redistributed in the following seconds. This causes a decrease in venous return to the heart and in cardiac filling pressures, which can lead to a decrease in stroke volume by 40% [24] and in a normal subject, orthostatic stabilization is obtained in a minute or less after standing up, thanks to the correct compensation of the autonomic nervous system, since the high pressure mechanoreceptors located in the carotid sinus and the aortic arch are activated, as well as the low pressure ones located in the heart and lungs [25]. Early adaptations to taking the upright position result in an increase in heart rate of 10 to 15 beats per minute and diastolic pressure of 10 mm Hg, with little or no change in systolic pressure [26]. The inability of any of these processes to function properly or in a coordinated manner results in a failure in the normal response to sudden postural changes, which generates hypotension, elements that may be sufficient to produce cerebral hypoperfusion, hypoxia, and loss of consciousness. Autonomic nervous system dysfunctions involve multiple and variable clinical manifestations, which are often underestimated in clinical practice. However, they must always be taken into account due to their diagnostic implication, due to their impact on the patient’s quality of life and due to their prognostic influence on life expectancy [27]. Therefore, the sympathetic function plays a fundamental role in the preservation of the organism, since it quickly and very effectively causes a response to external stimuli that may threaten the integrity of the individual and, for its part, the activation of the parasympathetic system is oriented, contrary to that of the sympathetic, to the conservation of energy. This fascinating and complex interrelation can be summarized below, with regard to primary non-degenerative dysautonomia.
Pathophysiology of Primary Non-Degenerative Dysautonomia: The vasomotor center is located in the brain stem, and it sends fibers to the spinal cord and blood vessels. Within the superior nervous control centers of the vasomotor center, is the motor cortex, which through integration through fibers to the hypothalamus, participates in an important way in the regulation that includes from environmental stimuli to emotional stimuli [28]. In this pathology, we find imprecise compensating responses from the central regulatory centers (bulbar vasomotor centers and superior nervous centers controlling the vasomotor center), towards the autonomic nervous system. Also, as pointed out by Cadman [17] and the psychiatry group of Warnock and Clayton [18], serotonin could play a very important role at the central level as the origin of these disorders, by causing a state of sympathetic hyperreactivity with hypo reactivity to the phenomena of stress. In general, diseases that affect the autonomic nervous system produce symptoms due to its hypoactivity or insufficiency; less frequently there are diseases that cause hyperactivity.
Natural History of Non-Degenerative Primary Dysautonomia: The pathophysiological study and clinical characterization of dysautonomia syndromes that manifest with orthostatic intolerance have been a challenge for researchers in all areas due to their frequent presentation and the lack of therapeutic tools that allow their adequate management, this context, invariably has repercussions on the knowledge of the natural history of the disease, since we remember that hypotension and dizziness as symptoms of orthostatic intolerance, only constitute part of the symptomatology of primary non-degenerative Dysautonomia, so the conceptualization of the natural history of the disease pathology globally speaking, it is also divided [29]. For example, the mortality rate is known to be increased among persons with syncope secondary to age-related orthostatic hypotension and concomitant conditions [30]. Derived from hypotension, syncope, dizziness and fatigue, patients have a tendency to suffer falls and accidents, with the presentation ranging from simple injuries, through fractures, severe head injuries and even death. In relation to gastrointestinal symptoms, patients present anorexia, and weight loss with a tendency to malnutrition, coupled with muscle pain and paresthesias, especially in the lower limbs, immobility is triggered, with the development of frustration, social isolation, depression, anxiety and behavioral alterations with development of comorbidities.
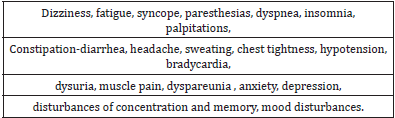
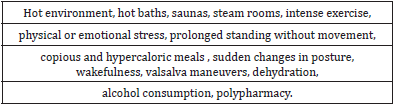
Clinical Manifestations and Diagnostic Criteria
Clinical Manifestations: The symptoms and signs are very varied and involve many organs and systems, which makes diagnosis difficult, and they can also overlap with each other. Among the most common we find (Table 3) as shown in the table above, the symptomatology involves several apparatuses and systems innervated by the autonomic nervous system, and added to the characteristic dysregulation, patients can be found in the spectrum of excess and/or deficit of innervation, usually deficit, what produces the polarity and alternation of the symptomatology. All these signs and symptoms are not standardized, there are no clinical practice guidelines for management, and treatment and consultations with other specialties are offered in relation to the findings in the clinical history and physical examination, usually at the time of diagnosis in based on the experience and individual criteria of the treating physician, often without carrying out a deep comprehensive approach and without taking into account the quality of life of the patient [14,31]. The symptoms can be triggered by different situations of daily life such as (Table 4). All the aforementioned triggers precipitate the symptomatology in proportion to the compensatory and homeostatic capacity of each patient and to the imprecise responses of the autonomic nervous system according to the course of the disease at a specific moment of the pathology [32]. We must mention the importance of the splanchnic circulation, which is the part of the systemic circulation that irrigates the abdominal portion of the digestive tube, as well as the spleen, pancreas, and liver.
It is the largest regional circulation arising from the aorta and receives more than a quarter of the left ventricular output during rest, regardless of whether the subject is freshly fed or not. This volume, for example, is equivalent to about ten times the blood flow received by the entire skeletal muscle mass at rest, an enormous figure if one takes into account that this mass has the largest vascular bed in the human body. This large size determines that the splanchnic circulation is the most important reservoir of blood in the entire body. Thus, when the systemic blood pressure tends to decrease for any reason, intestinal vasoconstriction will displace about a fifth of the blood volume towards the vital organs that require it. The most powerful stimulus to increase intestinal blood flow is the ingestion of food, so that the intestinal metabolic activity is multiplied to digest and absorb. The entry of chyme into the intestinal lumen increases, to a greater or lesser degree, the blood flow to the mucosa, depending on the type of constituents of that content and the amount. For example, in the jejunum, blood flow increases about 10 times more if it receives digested food mixed with bile compared with only bile or only amino acids. This has an important implication in the dietary recommendations as part of the initial treatment, suggesting a diet with a low carbohydrate content, in fractions and avoiding large meals [33-36].
Diagnostic Criteria: As is done with all patients, it begins with a complete clinical history, emphasizing the relevant history and the precise semiology of the symptoms. A detailed clinical history, with an adequate physical examination, and special attention in the cardiovascular and neurological areas, are invaluable for the diagnostic scope, overcoming the indiscriminate request for multiple tests. It is important to always identify any drug that the patient is taking, including non-allopathic drugs. When a young subject presents with symptoms of autonomic dysfunction, the possibility of illicit drug or alcohol abuse should be considered within the differential diagnoses. Diagnostic tests should be requested in a directed manner and determined by the findings, if necessary, laboratory tests such as complete blood count, blood chemistry, thyroid function tests, various hormonal profiles, general urine test, immunological profile, and tests cabinet that may include ultrasound, electrocardiogram, cardiac holter, echocardiogram, electroencephalogram, brain imaging studies such as tomography or magnetic resonance, in order to rule out other pathologies, integrate the probable diagnosis or diagnoses and stage them, to request consultations with other specialties, if necessary. A drop in systolic pressure of more than 20mm Hg or a drop of more than 10 mm Hg in diastolic pressure during the two minutes following standing after lying down is highly suggestive for the diagnosis, without the presence of reflex tachycardia [21,27,28]. If a negative diagnostic test is obtained and other organic alterations are ruled out, with the previously mentioned studies, the psychiatric evaluation can finally be carried out, because, as no organic alteration is found that justifies the patient’s symptoms after having carried out a complete study, specialized assessment is requested for the study of other types of pathologies with a mental and/or psychiatric context, which is not mentioned in this thesis, since it is not part of the stated objectives, as it corresponds to completely different topics.
Treatment
Therapeutic Options: Within the therapeutic options, we find general measures, diet, pharmacology and surgical treatments, according to the judgment and experience of the initial treating physician. The most commonly prescribed non-pharmacological measures are listed below [22,23] .
General measures:
i. Avoid prolonged standing.
ii. Avoid inactivity.
iii. Ambulation at a moderate pace.
iv. In a sitting position, avoid immobility for a long time.
v. Avoid extreme and sudden temperature changes (steams, saunas).
vi. Use of compressive elastic socks.
vii. Moderate aerobic exercise, as it improves venous return.
viii. Avoid high altitude cities, mountains, height and speed rides.
ix. Alterations in fluids and blood corrected as soon as possible.
x. Avoid sleeplessness, stress and Valsalva maneuvers.
xi. Sleep with the head of the bed raised (between 15 and 30cm).
xii. Use of stockings with elastic support (controlled pressure of 30 to 40mm Hg)
a) Pharmacology
Depending on the evolution, pharmacological treatment is suggested [22,23,29]:
i. Increase blood volume with the use of mineralocorticoids (Fluodrocortisone).
ii. Increase vasoconstriction with alpha agonists (Midodrine, Clonidine).
iii. Block the effect of norepinephrine with beta blockers (Propanolol, Metoprolol, Nadolol, Pindolol).
iv. The use of anxiolytics and antidepressants is sometimes necessary (Citalopram).
v. Selective serotonin reuptake inhibitors (Fluoxetine, Sertraline).
vi. Synthetic amino acid that is decarboxylated to norepinephrine without passing through the enzyme dopamine beta hydroxylase (Dihydroxyphenylserine) [37].
An interesting finding in a good number of patients with autonomic failure is the presence of anemia. In a study by Hoeldtke and Streeten , it was shown that subcutaneous injections of erythropoietin, in addition to raising cell counts, dramatically increased blood pressure [38].
b) Surgical Treatment
Pacemaker, which would only be indicated exceptionally for the management of recurrent syncope that does not respond to previous therapies. From the point of view of psychology, they propose adding to these patients, in order to provide a more comprehensive treatment, the work of emotional self-knowledge through integrative psychotherapy, and thus provide the patient with the tools to detect stress factors and their correct treatment management, promoting experiences that promote well-being, establishing as a priority the management of techniques that help identify negative emotions and address them in the best way [28].
Dietary Treatment
A diet is suggested that includes [39-44] :
i. Avoid dehydration, drink 2 to 3 liters of water a day until you achieve clear and diluted urine.
ii. Avoid copious meals.
iii. Rest 15 to 30 minutes after meals.
iv. Increase salt in meals; If there are no contraindications, 6 grams per day is recommended (place 2 level teaspoons of coffee in a salt shaker and add it to food daily).
v. Avoid alcohol.
vi. Three main fragmented meals and two intermediate snacks.
vii. Diet with carbohydrates that do not exceed 45% of the daily caloric intake [45-48].
Prognosis
There are no clinical, treatment, or prognostic pathology practice guidelines reported. As evidenced so far, the prognosis for these patients is generally good for life but guarded for function. Several daily syncopal episodes may occur, with frequent falls, exercise limitation and even mobility and independence, significantly affecting the prognosis, producing from complete recovery to a chronic debilitating course with significant residual effects. Diaphoresis and bowel and bladder function are also sometimes compromised, with bloating, nausea, vomiting, and abdominal pain being a frequent complaint. Constipation is frequent and sometimes alternates with diarrhea, all of this producing a significant impact on quality of life, which conditions the development of comorbidities, with depression and social isolation, in addition to the economic and labor cost for the patient and the health system, by referring it to multiple medical specialties, which study it in a “fractionated” manner.
In this way, the disclosure of this pathology is important, to expand the diagnostic horizons in medicine and not only in the area of Otorhinolaryngology, since it is possible that some patients diagnosed with benign paroxysmal positional vertigo and many other diagnoses of vertiginous pathology and others really correspond to Dysautonomia. It is necessary to carry out complete physical examinations visualizing the human being in an integral way, as in the old medical school, and thus avoid the division of signs and symptoms that lead us to multiple diagnoses, which unfortunately the specialization and sub specialization of medicine has focused on medicine today.
References
- Kaufmann H (2000) Primary autonomous failure: three clinical presentations of one disease? Ann Intern Med 13(5): 382-384.
- García Frade L (2015) A syndrome called dysautonomia (2nd)., In: García Frade L (Edt.)., Mexico, Bishop.
- García Frade L (2017) Proposals about functional disorders: dysautonomia? Med Int Mex 33(6): 813-817.
- Carnival C, Muñoz Proto F, Rama López J, Ferrán de la Cierva L, Rodríguez Villalba R, et al. (2014) Management of benign paroxysmal positionally vertigo at first care centers. Family medicine. SEMERGEN 40(5): 254-260.
- Goodmorning C, Buonanotte M (2013) Migraine Neuarg 5(2): 94-100.
- Horwitz B (2001) The irritable bowel syndrome. N Engl J Med 344(24): 1846-1850.
- Garcia Frade L (2016) Biliary dyskinesia syndrome. Med int Mex 32(6): 671-675.
- Garg N, Deodhar A (2012) New and modified fibromyalgia diagnosis criteria: Ambiguity , uncertainty , and difficulties complicate diagnosis and management . J Musculoskel Med 29(1): 13-15.
- Schondorf R (1999) The importance of orthostatic intolerance in the chronic fatigue syndrome. Am J Med Sci 317(2): 117-123.
- Harrison T, Resnik W, Wintrobe M, Thorn G, Adams R (1991) Anemias. Principles of internal medicine (12th)., In: Harrison T, Resnik W, Wintrobe M, Thorn G, Adams R (Eds.)., Mexico: Interamericana, Mc Graw-Hill, pp. 1757-1789.
- Domínguez R (2006) Guidelines for clinical action of diabetes mellitus. Diagnostic and therapeutic algorithm for hypoglycemia. Endocrinol nourish 53(Suppl 2): 17-18.
- Abrams P, Cardozo L, Fall M, Griffiths D Rosier P (2002) The standardization of terminology of lower urinary tract function: report desde the Standardization Subcommittee of the International Continence _ Society . Neurourol Urodyn 21: 167-178.
- Solis J, Fernández Friera L , Traveset C (2011) Mitral valve prolapse: do we know the problem we are facing? Rev fed arg Cardiolg 40(1): 5-12.
- Velarde Jurado E, Avila Figueroa C (2002) Methods for quality of life assessment. Public Health Mex 44: 349-361.
- Gutiérrez C (2020) Dysautonomia: a confused and relegated pathology. Psychosocial effects and intervention proposals.
- Flores S, Segura T (2005) Structure and function of muscarinic and nicotinic acetylcholine receptors. Rev Mex Neuroci 6(4): 315-326.
- Cadman C (2001) Medical therapy of neurocardiogenic syncope. cardiol Clin 19(2): 203-213.
- Warnock J, Kleiton A (2003) Chronic episode disorders in women. psychiatrist Clin North Am 26(3): 725-740.
- Brandan N (2010) Adrenal Catecolamina Hormones. Chair of Biochemistry. School of Medicine. 2010. UNNE.
- Dysautonomia – the failure of the central autonomic nervous system. Health Secretary. Government of Mexico.
- García Frade L, Martínez A (2006) Orthostatic intolerance.Med int Mex 22: 542-554.
- Berger M, Kimpinski K (2014) Practical Guide to the Treatment of Neurogenic Orthostatic Hypotense. Can J Neurol Sci 41: 156-163.
- Coghlan C (2001) Treatment of different autonomic syndromes failure. Medwave 1(04): e3350.
- Grubb B, Vesga B, Guzmán J, Silva F, Morillo C (2003) Autonomic dysfunction syndromes associated with orthostatic intolerance. Biomédica 23(1): 103-114.
- Bruno Estañol, Manuel Porras Betancourt, Gustavo Sánchez Torres, Raúl Martínez Memije, Oscar Infante, et al. (2009) Neural control of peripheral circulation and blood pressure. Arch Cardiol Mex 79(2): 109-116.
- Stewart J (2012) Mechanisms of sympathetic regulation in orthostatic intolerance. J Appl Physiol 113(10): 1659-1668.
- Bravo J (2004) Dysautonomia: a little-known medical problem. San Juan de Dios Hospital Bulletin. Chili 51: 64-69.
- Fernández J, Prieto M, Muñoz A, Lebrón M, Cabrera H, Quesada G (2006) Prognostic Influence and Computed tomography Findings in Dysautonomic Crises After traumatic Brain injury. J Trauma Inj infected crit Care 61(5): 1129-1133.
- González A (2020) Yesterday neurocirculatory asthenia today dysautonomia. Research Gate 2013 -2014(2): 15-27.
- Agudelo E, Agudelo J, Bolivar S, Salazar N (2016) Characterization of the population with Dysautonomia residing in the city of Medellin. Faculty of Physiotherapy. University CES.
- Cardona D, Agudelo G (2005) Cultural construction of the quality of life concept. Rev fact National Public Health 23(1): 79-90.
- Kaufmann H (2003) Most common dysautonomias . Rev Neurol 36(1): 93-96.
- García Alcalá H, Meaney Mendiolea E, Vargas Ayala G, Escalante Pulido M (2011) Current review of the knowledge on the intestinal absorption of carbohydrates and its relationship with the prevention of cardiovascular risk. Med int Mex 27(3): 270-280.
- Chou C, Coatney R (1994) Nutrient-induced changes in intestinal blood flow in the dog. Br Vet J 150(5): 423-437.
- Boushel R (2003) Metabolic control of muscle blood flow during exercise in humans. Can J Appl Physiol 28(5): 754-773.
- Marston A, Clarke J, Garcia J, Miller A (1985) Intestinal function and intestinal blood supply. Gut 26: 656-666.
- Saadia D (2019) Autonomic Dysfunction. Clinical manifestations, diagnosis and treatment. Neuromuscular Diseases and Autonomic Nervous System Section.
- FLENI Raúl Correa Neurological Research Institute, Buenos Aires, Argentina.
- Hoeldtke R, Streeton D (1993) Treatment of orthostatic hypotensive with erythropoietin. N Engl J Med 329: 611-615.
- Bravo J (2012) Difficulties in the Diagnosis and Treatment of Dysautonomia. Rev Chil Rheumatol 28(3): 152-158.
- Morillo C, Medina E (2005) Natural history, classification and epidemiology of syncope Colombian Society of Cardiology and Cardiovascular Surgery (1st).,
- Junta de Andalucía (2016) Training module. Diet and nutrition. Unit 3 Diet therapy.
- Lutz C, Przytulski K (2011) Nutrition and Diet Therapy Fifth Edition McGRAW-HILL Interamericana Editores, SA de CV 2011
- Duque R, Carvajal P, López S Cuartas A (2012) Dysautonomia: serial cases managed with magnetic mobile repolarized system. Medicine UPB 31(1): 27-33.
- Schmulson M (2000) Irritable Bowel. In: Principles of Gastroenterology. In: Méndez (Edt.)., pp. 501-510.
- Navarro X (2002) Physiology of the autonomic nervous system. Rev Neurol 35(6): 553-562.
- Feinberg A, Lane Davies A (2002) Syncope in the teen teenagers. Med 13(3): 553-567.
- Stewart J (2004) Chronic orthostatic intolerance and the postural tachycardia syndrome (POTS). J Pediatr 145(6): 725-730.

 Research Article
Research Article