Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Del Fresno I Castillo L*, Colino Paniagua C, Alvarado Lorenzo A, Alvarado Lorenzo M, Baptista Sanchez H and Colino P
Received: August 01, 2022; Published: August 18, 2022
*Corresponding author: Del Fresno I Castillo L, UCAM Catholic university of Murcia, Spain
DOI: 10.26717/BJSTR.2022.45.007248
Maxillary transverse deficiency and crowding in children are problems that are commonly encountered in orthodontists’ offices [1-5]. This maxillary volume deficiency has been related to a low tongue position in different studies, although this correlation is not clearly established. Its relation to airway volume has also been studied [6,7]. Patients with maxillary deficiency have lower nasal dimensions than usual, tend to exhibit more resistance to passage of air through the nose and are usually mouth breathers, when we compare them to patients with a normal maxillary arch [8]. Maxillary expansion is a widely used method used to fix crossbites and maxillary deficiencies, especially as early treatment in children [9]. Within the maxillary expansion we can find slow or rapid maxillary expansion. Both types of expanders have similarities, like a screw which activates the device, though slow expanders are less frequently activated than rapid expanders and have more dentoalveolar than skeletal effects [10-12]. In order to carry out the maxillary tooth-borne expansion, we should take into account the maturation of the midpalatal suture. Different authors such as Melsen [13] in 1975, Person and Thilander [14] in 1977 and Fishman [15] in 1994, made different classifications to define at what age the suture started to interdigitate and, therefore, have less capacity to be opened by maxillary expansion. Currently, the method we use the most to classify the suture stage is from Angelieri [16], who divides the midpalatal suture in 5 maturation stages. Her investigation establishes that chronological age is an unreliable parameter to determine the stage of the suture, because patients older than 11 years presented a great variability within this classification [17-19]. For this reason, it is vital to use CBCT before a rapid maxillary expansion [20].
In terms of width, Adkins observed in 1990 that, after toothborne expansion, he obtained 6,5 mm for intermolar width and 4,7 mm for arch perimeter in growing patients [21]. In 2015, D`Souza obtained 4,4 mm for intermolar width and 3,7 mm for arch perimeter, also in growing patients [22]. (Figure 1) On the other hand, rapid maxillary expansion in young adults is limited by the stage of the suture, so it is common to use other appliances to increase the arch perimeter, especially bone-borne expanders with miniscrews. In An’s article (2021), they observed that the molar width increase was similar both in patients that wore bone-borne expanders and those who wore tooth-borne expanders (5,79 vs. 5,32). However, there was a more skeletal and parallel expansion in adults who wore bone-borne expanders. In another article, it was established that with tooth-borne expanders in adults there was more tipping on the teeth where it rested, and more vertical bone resorption [23-25] (Figure 2).
a) To verify the efficiency of rapid maxillary expansion in growing patients at the skeletal level.
b) To assess nasal and maxillary width changes.
c) To evaluate what happens with regard to upper first molars in maxillary expansion.
d) Establish the differences between arch perimeter T1 and T2, both at coronal and root level.
A bibliographic search was carried out in the Medline-Pubmed and Google Scholar databases from December 2021 to May 2022 with the following key words: ‘Rapid maxillary expansion’, ‘RME’, ‘Midpalatal suture maturation’, ‘Hyrax expander’. The language used in the search was English. The selection of articles was done according to the abstracts and citations from the search.
A prospective clinical study was performed on a sample with 20 patients, 10 women and 10 men. The average age of the sample was 10,7 years old, the oldest patient being 15,8 years old and the youngest one 7,3 years old. All of them were treated with a Hyrax acrylic expander with a 0,2 mm screw cemented to the upper first premolar, upper second premolar and upper first molar, except on patients with mixed dentition. The patient records were provided by Colino Dental Clinic from Villanueva de la Serena (Badajoz, Spain). A cone beam computed tomography (CBCT) was taken before expansion (T1) and after expansion (T2). The CBCT device used was GIANO 3D ADVANCED 13x16 (WhiteFox, Satelec, Merignac, France) with these parameters of exposure: 105.0 kV. 105.0 kV peak, 8.0 mA, 7.20 s, with a 15 mm x 13 mm field of view (Table 1).
Note: *n=sample size.
▪Measured parameters
The measured parameters in each CBCT on the upper jaw were: coronal arch perimeter, root arch perimeter, palatal height, upper first molar angulation, width of the base of the nose, intermolar width and upper jaw width (JR-JL). The program used for the measurements was In Vivo Dental from Anatomage Inc. The measurement of the coronal perimeter was from mesial of the upper right first molar to mesial of the upper left first molar, passing through the vestibular face of each tooth on the arch. For the root perimeter, the same procedure was carried out but at the cementoenamel junction (CEJ) [21] (Figures 3 & 4). The palatal height was measured from the midpalatal suture, tracing a perpendicular line to the line formed from central fossa to central fossa of the upper first molars [26]. To measure the angulation of the first upper molars, a straight line was drawn parallel to the palatal base and then a perpendicular line was drawn to this one passing through the centre of the pulp chamber of both upper molars [27] (Figure 5). For the sutural opening, a straight line was drawn from right to left of the suture at the incisal level, as this is where a greater quantity of expansion is produced by the fanshaped opening pattern of the midpalatal suture after expansion [28] (Figure 6). For the width of the base of the nose, the posterior part of the nasal cavity was taken and then a straight line was traced from right to left of the base of the nose, in its lower portion [29] (Figure 7). For the width of the upper jaw JR-JL the lowest point of intersection of the zygomatic bone with the maxillary tuberosity was taken, from right (JR) to the left (JL) of the patient [30] (Figure 8) (Tables 2-5).
Table 3: Mean age, coronal perimeter, root perimeter and difference between T1 and T2.
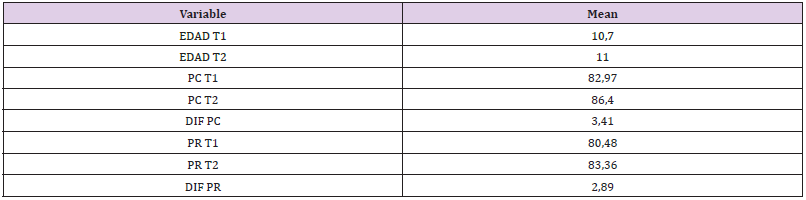
Note: **N: Patient; PC: Coronal perimeter; PR: Root perimeter.
Table 4: Data collection table B.
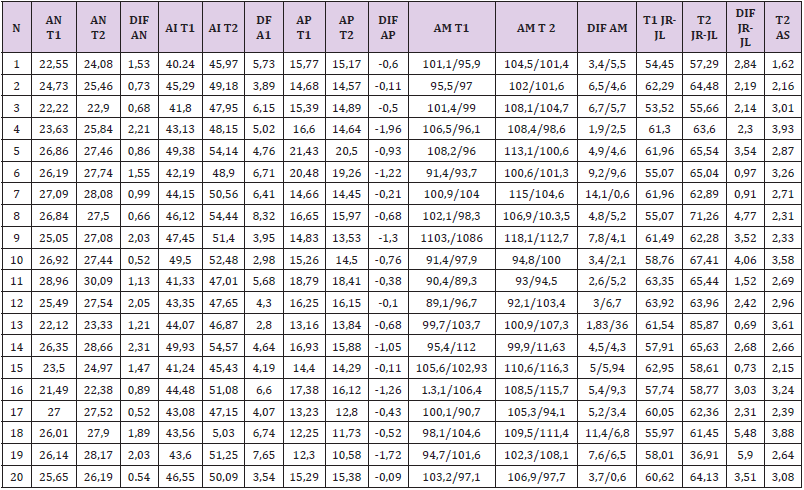
Note : **AN: nasal width; AI: intermolar width; AP: palatal height; AM: molar angulation; JR-JL: upper jaw width; AS: sutural opening.
The mean age before the treatment was 10,7 years old and 11 years old after the treatment. The arch perimeter increased after expansion, both at the coronal level, with an average of 2,93 mm, as well as root level, with an average of 1,97 mm. The width of the base of the nose increased in every patient after the expansion, the average being 1,29 mm. The intermolar width increased an average of 5,21 mm, on the other hand, palatal height decreased in 95% of the patients due to an increase of buccal torque, an average of 0,65 mm. Molar angulation was also altered by the expansion, increasing 5,65o and 4,74o respectively in terms of buccal torque. Maxillary width increased 2,79 mm in average. The mean midpalatal suture opening was 2,85 mm.
The measurement of molar angulation and intermolar width through CBCT is a novel method to analyse orthodontic cases from a more exact point of view in comparison to model analysis, as doctors Martinez Lozano and Diez Rodrigálvarez show in their article about the importance of CBCT in transversal diagnosis [27]. It is worth noting that their article is about a single case, not about a big sample that would help us understand what is going on after an expansion, because it is a case treated with fixed appliances and surgery. An article that provides similar data to our study is the one from Montes-Díaz and cols. and their investigation about 100 patients with impacted canines, where they measured the maxillary width and arch perimeter on the CBCT [31]. On this article, they show that in the control group, patients that did not have impacted canines obtained an average of 59,77 ± 4,14 mm of maxillary width. In our study, we obtained a similar result (59,68 mm). On the contrary, they obtained an average of 71,05 ± 3,25 mm for arch perimeter on the control group, and in our study, we obtained an average of 82,97 mm in T1. This difference is due to the method used to measure the arch perimeter: in Montes-Díaz’s article, they measured the arch perimeter passing through the contact points from the mesial part of the upper right first molar to the mesial part of the upper left first molar, but in our article, we measured the arch perimeter passing through the facial aspect of each tooth.
Another article with similarities is the one by Pereira and cols. article [32], that compares rapid maxillary expansion with slow maxillary expansion. They also measured molar angulation and upper jaw width (JR-JL). Unlike our study, they measured molar angulation tracing a line that passes through the mesiobuccal cuspid towards palatal root of the upper first molars, but they did not take each molar into account with the palatal plane as reference, as in our case. As for the upper jaw height at pretreatment, they obtained a similar number to ours, 60,13 mm. In post-treatment they obtained an increase in JR-JL of 1,76 mm with a standard deviation of 2,08 mm, something similar to our results (increase of 2,79 mm). An article of Abdalla and cols [33]. About the effects of rapid maxillary expansion and its influence on the airway also obtained similar data in terms of upper jaw width, but when they measured the intermolar width, it varied to a great extent. In their article, they measure from the palatal aspect of the upper first molars and we measure from the central fossa of each molar, so this is not an equivalent, although the results about the increase in the arch perimeter after expansion are similar to ours. Regarding the maxillary normal growth of the patients, in a recent study by Seubert [34] on 100 growing patients treated with fixed appliances without transversal deficiency, they took CBCT before and after the treatment. This shows us that in the skeletal aspect (the greater palatine foramina, the lateral walls of the nasal cavity, the infraorbital foramina) there is an increase of 0,5, 0,3, and 0,7 mm respectively per year. This indicates that a small part of the growth observed in the sample is due to the normal development of the patient. For example, if we take the increase of nasal width obtained after the treatment, we can say that 0,075 mm would be due to the normal skeletal development of the patient.
a. The fact that there are different ways of measuring CBCT for the same measurement, and no standardised way of doing so, makes it difficult to compare similar studies.
b. The measured parameters are reproductible, but they vary according to the operator, due to the fact that the benchmarking on CBCT is not automatic, but the operator should choose where to place them. For this reason, there will be an increase of intra-operator and inter-operator error when they study the same cases.
a. Tooth-borne expansion in growing patients is an effective method for increasing maxillary transversal distance and sutural opening.
b. Therefore, an increase in nasal width and upper jaw width take place.
c. Dental anchorage of tooth-borne expanders implies an increase of buccal torque of the upper first molar and an increase in intermolar width.
d. Arch perimeter rises, both at coronal and root level.


