Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rhea Joshi1*, Prem Periyasamy2 and Zubin J Daruwalla2
Received: February 09, 2023; Published: February 28, 2023
*Corresponding author: Rhea Joshi, PricewaterhouseCoopers USA, 300 Madison Avenue, New York, NY 10017 USA
DOI: 10.26717/BJSTR.2023.48.007730
This study describes and reviews the implementation and utility of a hardware and software solution designed by PricewaterhouseCoopers (PwC) to address a critical clinical population of migrant foreign workers living in dormitories in Singapore, the latter representing the majority of COVID-19 cases locally. Over a two-month period, the solution measured compliant and non-compliant movement of these dormitory residents via the use of wearable devices, location beacons, wave scanners, LoRAWAN gateways, and PwC’s “CONTRA” platform. The study successfully identified [1] hotspot locations for noncompliant movement and overcrowding, [2] rates of infection, [3] time periods of maximized violations, and [4] derived “infection fences” around potential clusters of infected individuals (high, medium, low risk) tailored to unique time, distance, and location parameters, each of which could be individually set. The solution was additionally able to calculate risk with proximity and time spent to infected individuals. This solution is recommended beyond the scope of this study given its accuracy of data collection (as low as 30cm between individuals), scalability and quick implementation timeline, two-year battery life span, resistance and durability to weather and water, low-cost (less than SGD $2 per user per month all-inclusive at scale), and most importantly, the ability to solve for all privacy and security concerns. This real-time solution rapidly and successfully facilitates contact tracing, location tracking and social distancing in the event of COVID-19 as well as future pandemics.
Keywords: Telehealth Solution; Covid-19; Foreign Workers; Migrant Workers; Location Tracking; Social Distancing; Contact Tracing; Singapore Dormitories
Background
Since its first reported case in late December 2019, the Coronavirus disease (COVID-19) has spread rapidly, afflicting over 101 million individuals worldwide and contributing to over 1.11 million deaths over its initial three years through till December 2022 [1]. According to the United Nations, an estimate of around 46 million foreign workers from Asia Pacific countries were reported migrating within the region in the same year, facing heightened risks of overcrowding, barriers to health, and exposure to respiratory infections due to their living conditions and worksites [2]. Within Southeast Asia, Singapore was identified as uniquely susceptible to the COVID pandemic, being one of the most densely populated countries (8385/km2) and attracting a high-volume of business and tourism-related travelers. Additionally, Singapore was and remains a major receiving country for migrant labor, with an estimate of 1,393,000 migrant workers (roughly 40% of Singapore’s total workforce) migrating largely from within the Southeast Asia region (Indonesia, Philippines, Myanmar, Vietnam, Malaysia, Thailand), South Asia (India and Bangladesh) and China [3,4]. Of these, no less than 981,000 are semi-skilled or unskilled workers, including 290,000 migrants within construction alone, over 131,000 in the shipyard sector [5]. and large clusters employed in domestic work, petrochemical marine, and other manual fields of work. While Singapore’s public health system acted quickly with their pre-existing knowledge of the SARS outbreak in 2003, their focus initially narrowed on the transmission amongst symptomatic cases within the foreign worker community, with a delayed recognition of the presence and criticality of pre-symptomatic and asymptomatic cases [6].
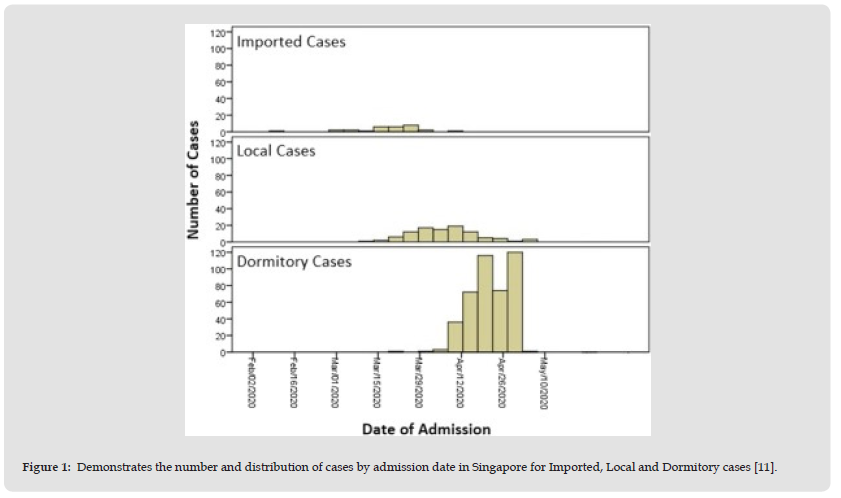
Despite being called, “The World’s Best Place to be during COVID,” [7] with one of the lowest case fatalities in the world (under 1700 deaths as of 2022) [8], migrant foreign workers were chiefly identified as a clinically vulnerable and high-risk population. By the end of the first wave in August 2020, the foreign worker population constituted over 90% of Singapore’s cases locally and over half had contracted COVID-19 [9]. Due to Singapore’s urban setting-- high land prices coupled with a high demand for employment-- migrant worker dormitories were left particularly susceptible to infections as a result of overcrowding in living structures, high staff turnover rate, and the continual arrival of workers that may have acquired undetected and asymptomatic infections from their countries of origin [2]. As a result, migrant worker dormitories and sites were quickly brought to the forefront as epicenters of infection, with the government declaring nearly a quarter of all registered dormitories in Singapore “isolation zones” by mid-April 2020 [10,11] (Figure 1).
Figure 1 Demonstrates the number and distribution of cases by admission date in Singapore for Imported, Local and Dormitory cases [11].
The Solution Landscape in Singapore
The Singapore government implemented numerous national and extensive control measures to mitigate risks. Some of these solutions involved contact tracing features, such as the voluntary Bluetoothbased contact tracing application TraceTogether [12], available to migrant workers and the general population on all smartphones, as well as Safe Entry [13], a mandatory digital check-in and check-out system that logged visitors’ entry into all venues. The application allowed for notification features in real-time, in the event that there was a close-contact exposure, by exchanging short-distance Bluetooth signals between phones. While dormitory-wide lockdowns were also implemented, enforcing social distancing and disinfection of dorms with a series of larger population circuit breaker measures [14], communal sharing of toilets and dining facilities made ad-hoc congregation and social distancing hard to limit and track, especially without compromising privacy. While the circuit breaker measures seemed to be effective for the larger population by end-May 2020, infections in foreign worker dormitories remained high, while the aforementioned solutions presented their own series of respective challenges.
Challenges with Solutions
In regard to these challenges, TraceTogether presented several that ultimately affected the extent of its effectiveness, adoptability, and accessibility within the general population [15]. From an accessibility standpoint, TraceTogether required a user to own or utilize a smart mobile phone (Android versions of 5.1 and above, or iPhones with iOS version 10 or above) to configure and download the app; all other versions of iOS, Huawei phones and Blackberry OS phones were unable to use the app or access the google play store for download [16]. Given the demographic of foreign workers, a number did not fulfill these prerequisites. From a technological standpoint, there were several challenges with the app’s reliance on Bluetooth signals for operation. As the app had to be configured to continuously run in the background of the user’s phone in order to be effective, high Bluetooth energy consumption was of concern (cite previous manuscript) affecting the longevity and durability of the tracking. In addition, Bluetooth signals risk losing connection in certain environmental conditions, have lower bandwidth than Wi-Fi, and only allow for short-range communication between devices, limitations that are especially critical when considering the manual labor settings in which the majority of Singapore’s foreign workers operate in. Privacy and security limitations were also major challenges that barred adoptability, with apprehensions about data privacy and government surveillance reaching an all-time high after the delayed public knowledge of TraceTogether data being used for a criminal investigation under the Criminal Procedure code: rather than an app used entirely for digital contact tracing as originally marketed and stated (cite here). Furthermore, an issue of inequality arose as, “Migrant workers are not subject to the same data privacy protections as Singaporean citizens and had to give up their privacy rights to participate in TraceTogether” which was made mandatory [17].
As a result of the aforementioned limitations, TraceTogether was only downloaded by about a quarter of the total population by mid-2020 (1.5 million users by June 2020) [18,19]. While studies have indicated that digital contact tracing tools can help to increase detection of cases and reduce time taken to contact-trace by 2.5 times, a minimum population adoption rate of 60% is required in order for these tools to be effective [20]. With the backdrop of this digital landscape and foreign workers at the epicenter of the virus, a strong digital solution was required to curb virus spread within dormitories, and to keep workers safe. Hence, in addition to the first pro-bono COVID-related support PricewaterhouseCoopers (PwC) Singapore provided to the Singapore government [21]. we additionally developed a collaborative but single trusted source of data collection to track workers’ location within dormitories, with a consolidated platform to support the Singapore Ministry of Health’s (MOH) identification of atrisk individuals. PwC Singapore worked pro-bono and collaborated with a dormitory and their operator, a cloud solution provider, and a third-party hardware provider to pilot a unique independent and low-powered software and hardware. The solution aimed to facilitate location tracking primarily, and in addition social distancing, and contact tracing. Furthermore, the solution aimed to accurately collect data and ensure the privacy and security of a user’s personal information, all while being scalable and low cost.
There were two key technology components involved in the pilot setup:
• Hardware - sensors, gateways, and transponders required to capture data from physical objects, including buildings and residents. Essentially, the mapping of a digital twin of the physical objects and locations within the dormitories.
• Software - data from the physical objects, processing of data, and applying business logic to report back to the central COVID-19 command centers to make critical decisions. Software components exclude the software within the hardware components.
Figure 2 Demonstrates hardware and software setup involved for the pilot study with transmission indicators.

As indicated by Figure 2 below, the hardware setup included 275 personal wrist beacons, and location beacons attached to 20 rooms, six toilets, six baths, three dining halls, and three ground floor porta cabin toilet areas. The personal wearable wrist beacons scanned for other wrist beacons and location beacons nearby exchanging Bluetooth low energy. Six wave scanners (two per floor) were also set up at exit and entry points to track and record proximity events. The LoRAWAN Gateway was installed in the building, and the data from the gateway was encrypted and transmitted via 4G/3G networks at a range of two to three Kms. Finally, the software setup included MicroShare’s (MS) Cloud based data storage, hosted by Amazon Web Services, where personal data and any other user data was purged upon transmission to PwC’s “CONTRA” data processing platform for location tracking, contact tracing and social distancing dashboards and reporting purposes. This data flowed through a data processing layer and other layers to be used for reporting and visualization purposes. Key activities and timelines for relevant stakeholders were as follows:
Day -14 (Setup)
• MOH
1. Access to the site (floor plans etc.)
2. Power & Installation Support
3. Integrating MS’ system to PwC’s platform
4. Educating users for the pilot
• PwC and MS
1. Assess and plan for the site
2. Setup and installation of hardware, configuring software
3. Providing data through APIs
4. Tagging test users and preparing for the pilot
Day 0- Pilot Live (16th July)
• MOH
1. Monitoring Pilot Launch
2. Reviewing Success criteria
3. Preparing for roll-out
• PwC & MS
1. Monitoring pilot launch
2. Providing analysis on success criteria
3. Preparing for roll-out
The pilot study ran from 16 July to 12 August 2020 and comprised 275 foreign worker residents in Tuas South, a Singapore dormitory. The dormitory had several floors, with each floor housing 200-500 residents. The study primarily aimed to measure compliant and noncompliant movement (as per prescribed medical advice) through the use of a wearable device. The study additionally aimed to identify hotspot locations for movement and overcrowding, rates of infection, time periods of maximized violations/movement, and aimed to derive an “infection fence” around potential clusters of infected individuals (by coloring high, medium, low risk users) tailored to time, distance, and location parameters, each of which could be individually set. The study aimed to utilize software to additionally calculate risk with proximity and time spent to infected individuals. With a combination of LoRaWAN and Bluetooth sensors, simple low power wide area coverage networks were set up to track proximity of two or more residents in a given physical location.
Figure 3 is a simple depiction of how three residents in a dining area with wristwatch sensors were tagged to a location. When the residents entered the door, Sensor #2 by the door recorded the resident’s entry and Sensor #1, within the room, monitored proximity of the residents. The Residents’ wrist watches, via Bluetooth, recorded proximity and reported to Sensor #2. With the combination of both the sensors, the pilot demonstrated data collection from physical location and the proximity of residents within the location. Software parameters were set to be less than two meters and interactions not longer than 2 minutes between individuals. These configurations were additionally adjusted based on requirements. For example, two residents interacting in the dining room for more than two minutes were recorded as an interaction in the COVID-19 command center. This data was merely stored until one of the residents in the interaction was found to be an infected individual.
The study successfully measured compliant and noncompliant movement (as per prescribed medical advice). In the last week of the pilot, results showed that by 5 August 2020, 28% of all movements were non-compliant to the medical advice provided at the time.
Additionally, the study successfully identified hotspot location for movement and overcrowding: a room on the second floor, communal dining areas, and porta toilets. Rates of infection, time-periods of maximized movement and infection fences were successfully defined, and the software was able to identify potential clusters of infected users based on calculations of risk with proximity and time spent to infected individuals.
Representations in the above figure (Figure 4) are as follows:
1. Fixed location landmarks represented as triangles. These location landmarks are digital twins of a physical locations at the dormitory (e.g., rooms, dining halls, toilets)
a. Hotspot location landmarks were represented as red triangles (rooms that attracted non-compliant and/or a high volume of visits)
b. Non-hotspot location landmarks were represented as grey triangles
2. Users wearing the wearable represented as circles with various colors indicating risk levels
a. No risk users that did not violate location parameters represented as grey circes
b. Medium risk users violating location movement to 1 location other than their base location were represented as an orange circle
c. High risk users moving to more than 1 location at a given time, with a higher violation rate, were represented as a red circle.
As shown in Figure 2 above, the software successfully deemed users as a “red” or “orange” level circle depending on the severity of their violation. Hence, for a set parameter of more than five minutes in an unauthorized location deemed as a violation, the red circles accurately represent people coming from more than one base location (high-risk users), whereas orange circles represented medium-risk users. This color coding was additionally applied to locations, with red triangles representing high-risk locations. Finally, the software easily adjusted for designated violations on a parameter time-constraint and physical location basis (e.g. more than X min spent in Y location separate from a user’s designated base location).
solution presented several successes, combining both hardware and software technology through the use of a Bluetooth wearable wrist beacon and a running cloud, fostering a zero-touch solution once installed. In addition, the solution was:
• Low-cost at less than SGD $2 (USD $1.50) per user per month all inclusive (software and hardware) at scale
• Easily scalable across an organization, a city, country, or region
• Quick implementation timeline
• Two-year battery lifespan
• No need to address privacy and security concerns as no personal data is stored or even acquired with standalone device not connected to mobile phone
• Standalone device does not require a mobile phone hence:
• It can be used at manual work sites (e.g., construction sites, etc.)
• Bluetooth will not drain phone battery, hindering effectiveness of solution
• It will not restrict adoption rates due to lack of IOS software/ mobile prerequisites
• Adjustable parameters for time/distance/location violations with evolving MOH guidelines
• Solution has a range accuracy of as low as 30cm between individuals
• Proximity metrics – can measure how close and long two or more residents in the dormitories are socializing
• Outbreak / Spread metrics – can measure the potential spread of COVID-19 when a single infectious individual engages in social interactions
• Customizable alerts and notifications
• All-weather and water-resistant solution (e.g. can be used in the shower)
• Sanitizable
• Strong sensory network. Low–Power, Wide-Area Networks (LPWAN)-- are projected to support a major portion of the billions of devices forecasted for the Internet of Things (IoT). LoRaWAN® was designed from the bottom up to optimize LPWANs for battery lifetime, capacity, range, and cost. The choice of LoRaWAN was considered because of the coverage and battery life given the residents of the dormitory will be mobile most of the time during the day and the technology covered large landscapes while always remaining ON.
The study was key in evaluating the effectiveness of this real-time solution in a real-world outbreak setting. In addition to resolving numerous issues experienced with alternative solutions such as data privacy and security, the key features of the hardware and software derived infection rates, infection clusters, real-time time-day trends of maximized movement, as well as location trends within the foreign worker dormitory setting. While this pilot study was used to address a specific clinical problem-- the inability to track where foreign workers were going after being allocated to specific rooms based on medical grounds-- the results of this study can be applied for far more use cases than a clinical solution for COVID-19. This solution is both relevant and pertinent with respect to location tracking, but also social distancing and contact tracing. These authors see minimal or no limitations to this solution and propose adoption at a global level. Public and private organizations alike, should consider this solution for wide-spread adoption globally in the inevitable event of a future pandemic.
Many thanks to the following persons for their pro-bono support and contributions:
1. A/Prof. Malcolm Mahadevan (NUH)
2. Dr. Julian Sham (AWS)
3. Mr. Ron Rock (Microshare)
4. Mr. Charles Paumelle (Microshare).
No known conflicts of interest exist.


