Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mohamed M Jaber*, Edward Qiao, Monte L Harvill and Farah A Nasser
Received: July 11, 2017; Published: July 19, 2017
Corresponding author: Mohamed M Jaber, Diagnostic Radiologist, Detroit Medical Center Corporation, Michigan, USA
DOI: 10.26717/BJSTR.2017.01.000203
Abbreviations: HAI: Hospital Acquired Infections; EMB: Eosin Methylene Blue; Staph A: Staphlococcus Aureus; MRSA: Methicillin Resistant Staphlococcus Aureus; E coli: Escherichia Coli
Lead radiation protection aprons and neck/thyroid shields are used by hospital personnel in rooms where ionizing radiation is present. These methods of radiation protection are used in the catheter lab by personnel such as interventional radiologists and interventional cardiologists who often perform procedures upon immunocompromised patients who are at increased risk for acquiring hospital acquired infections (HAI). In the United Kingdom, HAI constitute a substantial financial burden up to 1000 million euro per year [1]. Patients with HAI remain in the hospital 2.5 times longer and incur higher personal costs than patients without [2]. Since these radiation protective aprons are cleaned infrequently, they serve as a possible source of HAI [3,4].
Studies have shown that white coats and ties [3-6] are a reservoir for colonies of pathogens to grow and spread nosocomial infections. However, no study has been done to show whether lead shields that are worn by hospital personal, especially ones in the IR catheter labs, can be a source of nosocomial infection to their daily contacted patients and to themselves. Our study will address what types of pathogens grow on protective lead aprons and collars. Potential implications of this study include whether or not a policy should be proposed regarding protective lead maintenance and disinfection.
Twenty-five subjects, (radiology technologists, nurses, physicians, and physician assistants) were provided with a questionnaire detailing the amount of use and frequency of laundering. The study was conducted in a university hospital interventional radiology department. Two locations (Figures 1A & 1B) with potential patient contact were sampled: outer thyroid and chest shield and two locations with self body contact: inner thyroid and chest shield. The internal and external 25 cm2 surface of both the thyroid shield and shoulder of lead apron were sampled with a sterile swab and inoculated on sheep blood with novobiocin, bile esculin azide, eosin methylene blue (EMB), and sabouraud dextrose agar. These agars were specific for the identification of Staphlococcus Aureus (Staph. A), Methicillin Resistant Staphlococcus Aureus (MRSA), Escherichia Col (E. coli) and Tinea species. Studies have demonstrated that these organisms are associated with health care apparel contamination [3-5]. A CFU of 1 was considered a significant source of infection and was regarded as positive in this study. An expert microbiologist and a medical technologist were consulted with microbe interpretation. The data was analyzed using descriptive statistics methods.
Figure 1a&1b: With potential patient contact were sampled.

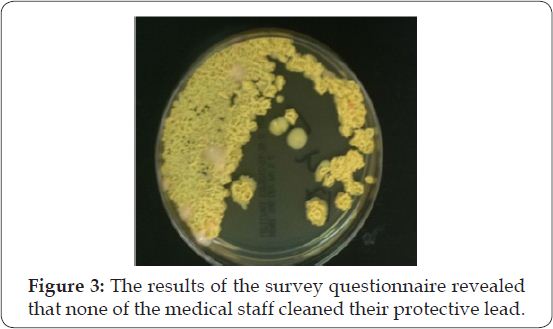
(Tables 1 & 2) The results of the survey questionnaire revealed that none of the medical staff cleaned their protective lead. Furthermore, in the last 10 years, none of the aprons were replaced. The majority of subjects wore the lead for at least 4-5 hours per day during procedures (Figure 2). Skin flora, (CoNS) were found on all lead aprons and thyroid shields, with (28%) having more than 20 CFUs. Colonies of Staph A was found on the lead aprons and thyroid shields of 21 subjects (84%); three of the isolates were resistant to methicillin (MRSA). Staph A was found on the outer protective lead of 12 subjects (48%) and interior of 11 subjects (44%). Tinea (Figure 3) species were also found on 21 lead aprons (84%). Tinea was found on the outer protective lead of 20 subjects (80%) and interior of 18 subjects (72%). E. coli and VRE were not detected on any protective lead aprons.
There was no statistically significant association with the time spent wearing protective lead and the presence of Staph A (Table 1) (Chi-Square=5.19, DF=5, p-value=.393). However, there was a statistically significant association between medical staff’s time spent wearing protective lead and the presence of Tinea species (Table 2) (Chi-Square=14.435, DF=5, p-value=.0131). Increase in Tinea colonies was related to time spent wearing protective lead aprons (Figure 2). The fellows had the highest amount of Tinea growth; 88% of sampled thyroid and lead shields showed fungal colonization, likely related to greater time of apron use. The lowest growth was found on physicians and physician assistants, both having 25% of their lead protection contaminated with Tinea species. For Staph A and Tinea species, there were no statistically significant difference between locations sampled on the thyroid and lead apron.
Table 1: Staphlococcus Aureus.
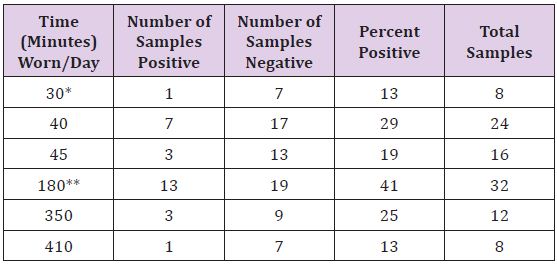
*Positive for 1 MRSA sample
**Positive for 2 MRSA samples
Table 2: Tinea Species.
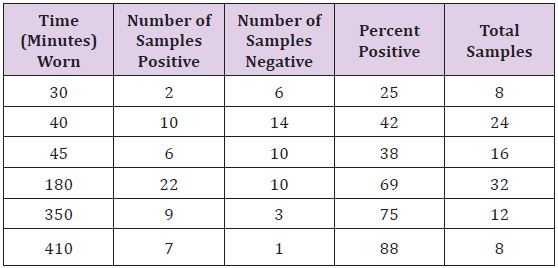
Figure 2: Tinea sp Colonization Rates.
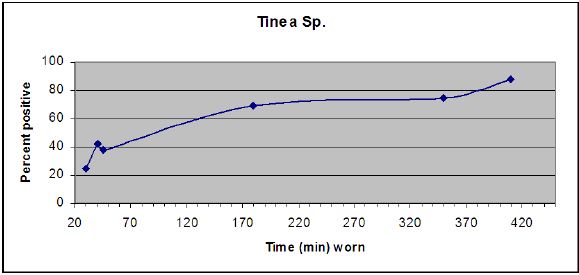
Figure 3: The results of the survey questionnaire revealed that none of the medical staff cleaned their protective lead.
Staph A and MRSA are known nosocomial pathogens that have the potential to cause significant morbidity. MRSA is one of the fastest growing hospital infections in the U.S. The number of reported infections in the U.S. hospitals grew from 2,000 in 1993 to 368,000 in 2005, according to the Agency for Healthcare Research and Quality [6]. Tinea species, such as Tinea corpus grow best in crowded, humid conditions. Perspiring excessively during long medical procedure could potentially cause growth of Tinea species [3]. Symptoms typically cause minor discomfort, such as rash and flaky skin, but can also cause significant morbidity and mortality in immune compromised individuals. The results of this study revealed that there were significant amounts of both Staph A and Tinea species residing in lead protection currently worn by interventional radiology medical staff. However, both pathogens appeared to have no predilection for a specific location on the protective lead; no significant differences were found between all four different locations on both the thyroid and lead shields. Furthermore, an almost equal number of subjects were contaminated with both pathogens on both the inner and outer surface of the protective lead.
The study showed no statistically significant differences between length of protective lead wearing and colonization with Staph A Tinea contamination was highly correlated with the length of time (Figure 1) (Pearson correlation coefficient=.946 with p-value=.002). 42% of lead aprons worn by staff that lasted less than 40 minutes were colonized with Tinea species compared with 69% of lead aprons colonized when worn for three hours or more. This may be due to the fact that Tinea species thrive in moist environment such as human skin folds [6]. As the individual wears the protective lead for a longer amount of time, body moisture builds, which leads to a more suitable environment for colonization. The study found that the majority (84%) of protective leads harbored both of these pathogens. This data warrants further action, especially given the length of time worn without cleaning. Lowered infection rates would reduce morbidity and health care costs. We propose that cleaning the leads before or after each use with a disinfectant once a day could drastically reduce the amount of pathogens present. Additionally, wearing a protective garment underneath the lead could minimize both patient and physician exposure to the pathogens.
There are a few limitations to this study. The 25 subjects were taken from a single department in one urban academic medical center. These results may not reflect the nosocomial colonization in other facilities. A future study may focus on additional and more diverse subjects across different departments and hospitals. The study was conducted in December, which according to some studies is the height of MRSA infections. Future studies may be conducted at different seasons throughout the year to minimize this effect.


