Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sumit Bhateja 1* Geetika Arora2 and Santosh Kumar Mastud3
Received: July 19, 2017; Published: August 01, 2017
Corresponding author: Sumit Bhateja, Reader(MDS), Department of Oral Medicine Diagnosis & Radiology, College of Dental Sciences & Hospital, Indore,India
DOI: 10.26717/BJSTR.2017.01.000241
Recurrent intraoral herpes (RIH) appears to be an infrequent problem. The lesions of RIH are characteristic and can usually be distinguished from others. The lesions of intra oral herpes may persist and be very serious in patients with a compromised immune system. Here we present a case of recurrent intraoral herpes infection in a young female which is uncommon.
Keywords: RIH; HSV; Infection
Abbreviations: RIH: Recurrent Intraoral Herpes; HSV: Herpes Simplex Virus
The herpes comes from greek word meaning to creep or crawl [1]. The human herpes virus family is officially known as Herpetoviridiae. Humans are only natural reservoir for these viruses, which are endemic worldwide & share many features. Best known member is Herpes Simplex Virus which exists in two types i.e. HSV -1 & HSV-2 [2]. Oral infection with herpes virus occurs in three clinical forms. The most common type consists of recurrent small blisters on the lips commonly referred to as fever blisters or secondary herpes labialis. The second type is a generalized oral infection called primary herpetic stomatitis. The third and least common form of recurrent oral herpes infection consists of small ulcers usually localized on palatal mucosa [2]. Recurrent intraoral herpes appears to be an infrequent problem. The lesions of RIH are characteristic and can usually be distinguished from others. The lesions of intra oral herpes may persist and be very serious in patients with a compromised immune system. While the virus may regress, it does not disappear [3].
A 26 year old female patient reported to the Department of Oral Medicine & Radiology with a chief complaint of soreness in the roof of mouth since 1 day (Figure 1). There is history of difficulty in swallowing food & patient finds it difficult to chew solid foods because of the burning sensation that is constantly present since 2 days. Patient also gave history of mild fever, nausea, malaise & loss of appetite since 1-2 days. Patient gave history of emotional stress due to family feuds since 3-4 months. Patient also reported a history of recurrent ulcers in mouth with fever & chills about 1-1.5 years back for which patient took medications from a local practitioner & practitioner informed patient it to be a viral infection. Anamnesis was non contributory. On intra oral examination multiple crops of thin walled vesicles surrounded by an inflammatory base each measuring to about 1-5 mm in size having round shape present all over left half of hard palate extending beyond midline of palate. On palpation vesicles were tender & firm in consistency & rupture on digital pressure discharging fluid from within (Figure 2).

figure 1:Front View Profile.
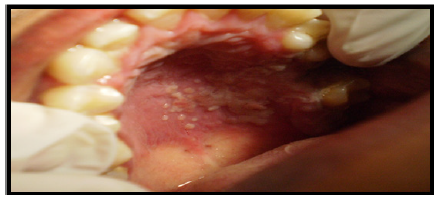
Figure 2:Recurrent Intraoral herpes involving hard palate.
Investigations carried out were routine hematological tests (within normal range except Hb% which was low), HIV 1&2(nonreactive) & exfoliative cytology. Then smear was sent for histopathologic examination which revealed clusters of altered epithelial cells that show balloning degeneration with enlarged nuclei, condensed chromatin & multinucleation, features suggestive of Herpes Simplex Virus infection (Figure 3). Based on history, clinical & histopathological examination a final diagnosis of Recurrent Intraoral Herpes Simplex Virus infection was put forth. Treatment plan for the patient included, oral hygiene instructions, soft bland diet advised & Paracetamol 500mg tablet on SOS basis. Followup was done after 1 week (Figure 4).
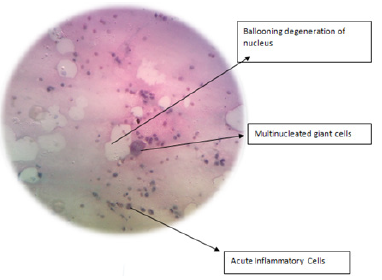
Figure 3:Photomicrograph showing features of HSV infection.
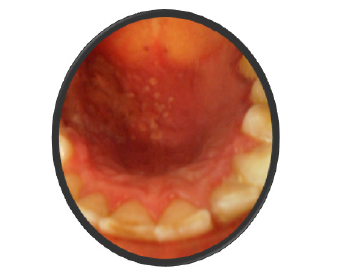
Figure 4:Follow up after 1 week.
The term ‘herpes’ is often used loosely to refer to infections with Herpes Simplex Virus(HSV), a ubiquitous virus which commonly produces lesions in mouth & oropharynx [1]. All herpes simplex viruses contain DNA nucleus which can remain latent in host neural cells, thereby evading host immune response. HHV-6 is a newly discovered virus and can infect T-4 cells and is a possible factor in HIV infection. Herpes Simplex Virus is the most common viral disease affecting men.
In children and adults who are immuno competent, primary herpetic infections may be annoying and uncomfortable, but they rarely cause significant morbidity or mortality. In individuals who are immuno suppressed, primary herpetic infections can be severe, and, occasionally, they can cause esophagitis, encephalitis, kerato conjunctivitis, and other diseases. The other forms of HHV can result in death. Herpes infections occasionally trigger erythema multiforme [2]. Primary clinical infection with HSV usually caused by HSV-1, seen mainly between ages of 2-4 years. It is increasingly seen in older patients. When seen in teenagers it is due to HSV-2 transmitted sexually & may mainly cause orophayngeal soreness [2].
Herpes Simplex Virus is contracted from infected saliva or other body fluids after an incubation period of approximately 4-7 days. Close contact with infected individuals, such as in play groups or sexually active persons predisposes to infection. HSV-1 can cause oral or orophayngeal infection usually via infection from saliva, and is most frequent & at a lower age in lower socioeconomic groups. HSV-2 can cause severe oropharyngeal infection usually via orogenital or oroanal sexual contact [3]. Herpes Simplex Virus anogenital infection is contracted from infected semen,saliva or other body fluids. HSV-1 genital infection is usually less common & less severe than HSV-2 infection. Patients with immune defects are liable to severe and/or protracted HSV infections [3].
Physical contact with an infected individual is the typical route of HSV inoculation for a seronegative individual who has not been previously exposed to the virus or possibly for someone with a low liter of protective antibody to HSV. The virus binds to the cell surface epithelium via heparan sulfate, followed by the sequential activation of specific genes during the lytic phase of infection. These genes include immediate early (IE) and early (E) genes coding for regulatory proteins and for DNA replication, and late (L) genes coding for structural proteins [4].
Documentation of the spread of infection through airborne droplets, contaminated water, or contact with inanimate objects is generally lacking. During the primary infection, only a small percentage of individuals show clinical signs and symptoms of infectious systemic disease, whereas a vast majority experience only subclinical disease. This latter group, now seropositive, can be identified through the laboratory detection of circulating antibodies to HSV [4]. The incubation period after exposure ranges from several days to 2 weeks. In overt primary disease a vesiculoulcerative eruption (primar gingivostomatitis) typically occurs in the oral and perioral tissues. The focus of eruption is expected at the original site of contact. After resolution of primary herpetic gingivostomatitis, the virus is believed to migrate, through some unknown mechanism, along the periaxon sheath of the trigeminal nerve to the trigeminal ganglion, where it is capable of remaining in a latent or sequestered state [5].
During latency no infectious virus is produced; there is expression of early, but not late, genes; and there is no free virus. No major histocompatibility (MHC) antigens are expressed, so there is no T-cell response during latency [5]. Some 50% of primary HSV infections are subclinical.
The main features of clinical primary disease are:
A. The mouth or oropharynx is sore
B. A single episode of oral vesicles which may be widespread, and break down to leave oral ulcers. These are initially pin point but fuse to produce irregular painful ulcers
C. Acute generalised marginal gingivitis
D. Cervical lymph nodes may be enlarged & tender.
Usually several nodes in anterio triangle of the neck – especially the jugulo digastric nodes – are enlarged often bilaterally. Posterior triangle & nodes elsewhere are not enlarged, unless there are systemic complications or lesions in other sites. There is no hepato splenomegaly unless there are systemic complications or lesions elsewhere. There is sometimes fever and /or malaise [6]. Diagnosis is largely clinical.
Lab investigations include-
A. Culture –takes days to give result.
B. Electron microscopy –is not always available.
C. Polymerase chain reaction detection of HSV-DNA-is sensitive & Rapid but expensive.
D. Immuno detection – conventional enzyme linked immuno sorbent assays (ELISA) for serum antibodies have poor sensitivity & specificity. While newer assays based on IgG1 HSV glycol proteins are comparable with western blot assays.
E. A rising titre of serum antibodies is confirmatory but only gives the diagnosis retrospectively.
F. Smears for viral damaged cells –routinely used [7].
Although patients eventually have spontaneous remission, treatment is indicated particularly to reduce fever & control pain. Adequate fluid intake is important, especially in children. Antipyretics/ analgesics such as paracetamol/ acetoaminophen to releive pain & fever. A soft bland diet as mouth can be very sore. Local antiseptics (0.2% aqueous chlorhexidine mouthwashes) may aid to resolve painful lesions. Acyclovir orally or parenterally is useful mainly in immuno compromised patients or in otherwise apparently healthy patient if seen early in the course of the disease. Anti virals do not reduce the frequency of subsequent reccurences.
Herpetic infections represent a reactivation of the herpes simplex virus, which is highly infectious to patients, their families, dentists and staff members. The diagnosis of these conditions usually is based on case-specific historical findings, the characteristic clinical appearance and the location of the lesions. Dentists often treat patients with a history of recurrent herpetic infections. Until the herpetic lesions are completely healed, the dental team should use management strategies to prevent spread of the virus, ensure adequate nutrition and maintain appropriate oral hygiene practices.


