Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sonia Nath1, Shaju Jacob Pulikkotil*2, Jayant Prakash3, Ajoy Kumar Shahi1 and Sultan Omer Sheriff2
Received: July 24, 2017; Published: August 16, 2017
Corresponding author: Shaju J Pulikkotil, International Medical University, School of Dentistry, Kuala Lumpur, Malaysia 57000
DOI: 10.26717/BJSTR.2017.01.000273
Adenomatoid odontogenic tumour (AOT) is a rare slow growing tumour, usually associated with an impacted tooth commonly situated in anterior maxillary region. A 14 year old young female complained of swelling on left side of her face which was increasing progressively in size. Aspiration revealed yellow coloured fluid and radiographically a unilocular radiolucent area was seen associated with an impacted canine. The lesion was suspected to be dentigerous cyst. Enucleation was performed and the excised tissue was sent for histopathological examination. Microscopic examination revealed AOT showing presence of spindle shaped cells and numerous cystic spaces surrounded by cuboidal or columnar cells. Few epithelial cells formed rosette like structure with eosinophillic coagulum in between.The features of both dentigerous cyst and AOT were overlapping in the lesion. Therefore proper clinical, radiographic and histopathological examination is critical for accurate diagnosis and treatment planning for lesions associated with impacted tooth.
Keywords: Adenoatoid odontogenic tumour; Dentigerous cyst; Impacted tooth; Odontogenic tumour; Unerupted tooth; Unilocular
The Adenomatoid odontogenic tumour is considered as a benign, nonneoplastic,non invasive, lesion with a slow but progressive growth [1]. Philipsen and Birn suggested the most widely accepted abbreviated terminology for Adenomatoid odontotgenic tumour, as AOT [2]. Various names have been used in the literature for AOT like adenoameloblastoma, ameloblastic adenomatoid tumour, adamantinoma, epithelioma adamantinoma, or teratomatous odontoma [3]. AOT is an uncommon tumour of odontogenic origin, accounting for 2.2-7.1 % of all odontogenic tumours [4]. The lesion was initially described by Steensland in 1905 and later further described by Philipsen and Reichart in 1907 as they described three clinical-topographic variants of AOT: follicular (71%), extrafollicular (23%) and peripheral (4%). The follicular and extra follicular occur in intrabony sites while peripheral variant occurs in the gingival issue of the tooth bearing area [4].
The lesion usually presents as an asymptomatic slow growing lesion which is often associated with an unerupted tooth [1,3]. The tumour may be partly cystic and in some cases the solid lesion may be present as masses in the wall of a large cyst. Few reports have suggested the epithelial lining of the odontogenic cyst may transform to an odontogenic tumor like AOT or ameloblastoma [5-8]. We present a case of follicular type of AOT in a 14 year old young girl in anterior maxillary region with clinical and histological presentation overlapping with dentigerous cyst.
A 13 year old female patient reported to the outpatient department of Dental Institute, Rajendra Institute of Medical Sciences, Ranchi on April, 2017. The patient complained of swelling on the left side of the face since 6 months which was increasing progressively causing disfigurement of left side of the face. The face was asymmetrical, due to diffuse solitary swelling of about 4 cm x 5 cm on the left maxillary region of face. On palpation the swelling was firm in consistency, non tender and fixed to the underlying bone and free from overlying skin (Figure 1). The intraoral examination showed mucosa of normal coral pink in colour, with diffuse swelling causing expansion of buccal cortical plate,measuring about 3 cm x 2 cm extending from left maxillary lateral incisor to second molar region mesio-distally and supero-inferiorly from free marginal gingiva to buccal vestibule causing its obliteration. The left permanent maxillary canine was missing with an over retained deciduous canine in its place. The left maxillary premolars and deciduous canine showed drifting with severe mobility.On intraoral palpation the swelling was diffuse, firm, and slightly tender with egg-shell crackling of buccal cortical bone.
Figure 1: Patient showing extraoral swelling on left side of face.

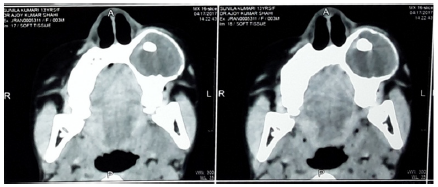
The medical and family history was not significant. There was no history of trauma, adverse habit, and was not under any medication. The patient tested negative for hepatitis B, C, and HIV. The blood examination revealed no abnormality. Aspiration revealed clear and straw coloured fluid. Orthopantomogram (OPG) and CT-scan of face was advised for the patient. Orthopantomogram showed well defined, unilocular corticated radiolucency associated with an impacted canine, extending from apical region of left maxillary lateral incisor to left maxillary first molar with the involvement of deciduous canine and premolars. The roots of deciduous canine and premolars were resorbed with distal displacement of both the premolars (Figure 2). CT-scan showed well defined unilocular radiolucent lesion with radio opaque border causing expansion of buccal cortical plate (Figure 3).
Figure 2:Orthopantomogram showing unilocular corticated radiolucency with an impacted canine.

Figure 3:CT scan showing unilocular radiolucency causing expansion of buccal bone.
According to clinical and radiological findings a provisional diagnosis of dentigerous cyst was considered. Differential diagnosis includes unicystic ameloblastoma, odontogenic keratocyst, calcifying odontogenic cyst, calcifying odontogenic tumour and AOT. Surgical enucleation of the lesion was planned under local anaesthesia. Infraorbital and middle and posterior superior alveolar nerve block and greater palatine nerve block were given. A mucoperiosteal flap was raised on buccal side with releasing incisions on both sides of the flap. The buccal cortical bone appeared to be thinned out completely with shells of bone in between. The thinned bone was removed to expose the cystic lesion. The whole encapsulated cyst with its lining was carefully separated from the mucoperiosteum and the lesion was enucleated along with the impacted canine.The cavity was thoroughly curetted, debrided and irrigated with saline and betadine. The over retained deciduous canine, and premolars were extracted and the wound was closed by primary intention with 3-0 black silk suture.
Figure 4:A) Gross specimen enclosing the crown of canine. B) Cut section of specimen showing cystic spaces in between solid masses.
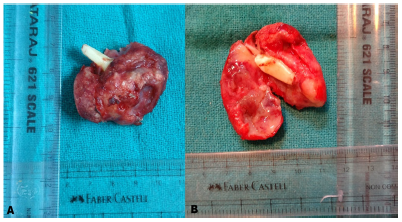
Figure 5:Photomicrograph showing numerous tubular or duct like cystic spaces surrounded by cuboidal or coulumnar cells.
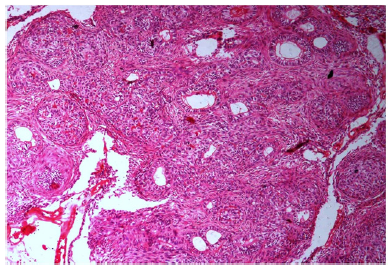
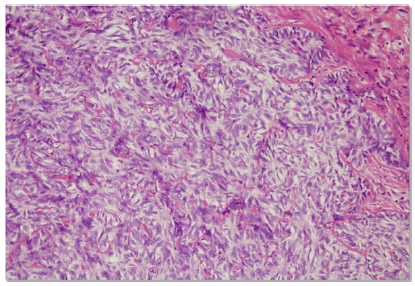
The excised specimen was reddish white in colour, size of about 4.5 x 4.0 x 3.0 cms, round in shape, having irregular and rough surface, firm in consistency, enclosing the crown of an impacted canine. The specimen was cut into half showing cystic spaces in between solid tissue (Figure 4). The histopathological examination revealed a well developed connective tissue capsule with solid masses and few large and small cystic spaces. Between the epithelial cells as well as in the centre of rosette-like structures showed presence of amorphous eosinophillic material.Numerous tubular or duct like spaces were present surrounded by cuboidal or columnar cells, the nuclei of which was polarized away from the central lumen (Figure 5). Magnification showed the presence of spindle shaped cells or polygonal cells forming sheets, strands and whorled masses in a scant connective tissue (Figure 6). These findings were suggestive of follicular type of AOT.
Figure 6:Photomicrograph showing spindle cells forming sheets, strands and whorled masses.
This report describes a case of slow growing lesion in young female which was misdiagnosed as dentigerous cyst based on clinical and radiographical features. The follicular type of AOT is often initially misdiagnosed as dentigerous cyst and final diagnosis was only confirmed after histopathological examination. Very few cases have been reported of AOT associated with dentigerous cyst [5-8]. This tumour can also be referred as 2/3rd tumour as 2/3rd of cases occurs in maxilla, 2/3rd in young females, 2/3rd are associated with unerupted teeth and 2/3rd are associated with impacted canine [9]. The tumour most commonly occurs in second or third decade. Similarly, our patient was a young 14 year old female, with the lesion situated in left maxilla which was associated with an impacted maxillary canine. Although AOT has been reported in other areas of the jaws such as in the maxillary sinus, posterior maxillary regions and in anterior mandibular region. This is possibly due to presence of dental laminar remnants which may likely represent the progenitor cells. The size of the lesion usually is 1-3 cm, but in our case the lesion was larger in size.
Three variants of AOT has been described by Philipsen and Richart; follicular, extrafoliicular and peripheral. The follicular variant is the most common variant having a central lesion associate with an impacted tooth [4]. Approximately 77% of the follicular variants are provisionally diagnosed as dentigerous cyst [5]. Similar to dentigerous cyst the lesion in our patient was clinically hard, painless, associated with an impacted canine and aspiration revealed straw coloured fluid. AOT is most commonly associated with impacted canine or anterior maxilla whereas dentigerous cyst occurs mostly with impacted mandibular third molar and maxillary canine. The pericoronal radiolucency in dentigerous cyst encloses the coronal part of the impacted tooth while AOT may enclose both coronal and radicular, and sometimes the entire tooth. AOT are usually seen in young teens with female predilection usually below 20 years, whereas a dentigerous cyst seen in second to the third decade of life with male predilection [10]. AOT is usually 1-3 cm rarely may enlarge up to 7 cm. A normal dental follicular space is approximately 3-4 mm and a follicular space of 5 mm or more is suspicious of a dentigerous cyst. Furthermore, AOT may displace adjacent teeth where as dentigerous cyst may not displace the adjacent teeth until attain a large size [11]. Our patient had clinical and radiological features of both the condition overlapping, with more inclination towards dentigerous cyst. After histopathological examination AOT was confirmed and it may be associated with dentigerous cyst.The tumour was partly cystic in between the solid lesion.
The pathogenesis of AOT is controversial. Some authors state the origin to be from odontogenic epithelium of a dentigerous cyst. Our case was cystic variety of AOT, as its growth was in the walls of the dentigerous cyst. Histopathology revealed numerous cystic spaces which were surrounded by cuboidal or columnar cells. In the literature very few cases of AOT arising from dentigerous cyst have been described [5-8]. Few authors reported a case of AOT being developed in the fibrous capsule of dentigerous cyst [5,12]. Garci Pola et al. [12] described the proliferation of an AOT in the epithelial border of dentigerous cyst. Therefore, dental laminar remanants could be the progenitor cells for this benign odontogenic tumour. According to envelopmental theory the lesion grows next to or into nearby dental follicle. According to literature, the cells of AOT usually differentiate toward an apparent ameloblastic phenotype but fail to achieve further functional maturation [4]. According to WHO “Histological Typing of Odontogenic Tumours”, AOT is defined as a tumour of the odontogenic epithelium with duct like structures and with varying degrees of inductive changes in the connective changes [13]. The latest WHO definition, states that an “AOT is composed of odontogenic epithelium in a variety of histoarchitectural patterns, embedded in a mature connective tissue stroma and characterized by slow but progressive growth [14].” There should a fourth variant of AOT, where both dentigerous cyst and AOT co exist together.
The lesion was large and extensive which involved the surrounding supporting bone of adjacent teeth leading to migration, drifting and mobility. Therefore if was planned to extract the involved teeth. The recurrence rate (0.2%) is very rare [7,8]. The lesion was well encapsulated enucleation with peripheral osteotomy provides success in treating the lesion. A diagnosis of AOT can only be confirmed by combined accurate clinical, radiographical and trans-surgical observation, biopsy specimen examination and histopathological evaluation. This approach will help determine the most effective treatment and prevent recurrences. There is a possibility of a fourth variant of AOT which is combination of dentigerous and AOT.


