Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Murat Karacan1, Feyza Karagoz Guzey1*, Ozgur Yusuf Aktas1, Azmi Tufan1, Abdurrahim Tas2, Burak Eren1,Ilker Gulec1 and Mehmet Sar3
Received: August 07, 2017; Published: August 17, 2017
Corresponding author: Feyza Karagoz Guzey, Health Sciences University, Bagcilar Training and Research Hospital, Neurosurgery Clinic, Istanbul 34093 Turkey
DOI: 10.26717/BJSTR.2017.01.000277
Medulloblastomas are usually in desmoplastic type in adults. This type of medulloblastoma is generally a well-circumscribed tumor. In this report we present an adult patient with desmoplastic medulloblastoma with atypical appearance on magnetic resonance imaging mimicking cerebellar infarction, infectious or demyelinating diseases. He was followed for atypical radiological imaging with misdiagnoses of those diseases. However, histological diagnosis was desmoplastic type medulloblastoma.
Keywords: Atypical Radiology; Brain Tumor; Desmoplastic medulloblastoma
Abbreviations: MB: Medullablastoma; MRI: Magnetic Resonance Imaging; MRS: Magnetic Resonance Spectroscopy; NAA: N Acetyl Aspartate
Medullablastoma(MB) that is the most frequently seen malignant brain tumor in childhood constitutes less than 1% of the brain tumors in adults [1], and nearly 50% of them was in desmoplastic type [2]. It has been reported that adult MB is also distinct from pediatric MB in genomic aberrations, histopathology, and prognostic outcomes [3-5]. Unlike childhood cases, adult MBs tend to be desmoplastic in histological type and to locate at cerebellar hemisphere rather than cerebellar vermis [2]. The adult desmoplastic tumors are usually well-circumscribed tumors and they can be easily dissected and resected. However, it has been reported that they may rarely be presented within atypicalinfiltrative appearance [6,7]. We reported an adult patient with an infiltrating diffuse desmoplastic MB affecting both cerebellar hemispheres and vermis.
A 34-year-old male patient was admitted with complaints of severe headache and ataxia for 3 months. His clinical history revealed that he had been followed by another center because of diffuse cerebellar lesion with pre-diagnoses of cerebellar infarction, infectious or demyelinating diseases. He had been hospitalized and external ventricular drainage had been applied for a few days, but a biopsy had not been performed. Then he had been discharged for outpatient follow-up. The patient was admitted to the emergency service of our hospital because his headache was extremely increased 1 month after he was discharged.
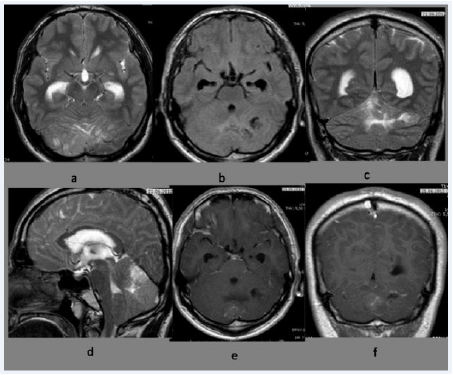
There was cerebellar ataxia in his physical examination. On magnetic resonance imaging (MRI), a diffuse lesion extending to the both cerebellar hemispheres and the vermis with mass effect and a moderate hydrocephalus were seen. The diffuse lesion had a small cystic part on the left cerebellar hemisphere. It had irregular hypointensity on T1-weighted sections and hyperintensity on T2- weighted sections. After intravenous contrast administration, a weak/insignificant heterogeneous staining was seen (Figure 1). Magnetic resonance spectroscopy (MRS) revealed increase in the choline peak and choline/creatinine ratio and extreme decrease in N acetyl aspartate (NAA) peak and NAA/ choline ratio led to diagnosis of malignancy.
Because of the severe continuing headache of the patient, an operation was planned. Infiltrating and diffuse lesion was partially removed and cerebellar tissue was decompressed. Headache completely diminished after operation and ventricle dilatation was decreased. The pathological investigation revealed a medulloblastoma in desmoplastic type with nodular appearance and without necrosis. Mitosis rate was high and Ki-67 score was 20-40%. The tumor cells were positive for neuron specific enolase, S-100, and synaptophisin, and it was negative for glial fibrillary acidic protein, desmin and pancytokeratin by immune histochemistry. The patient received radiotherapy after operation, and the tumor did not recur during 3 years follow-up.
Figure 1: Preoperative T2-weighted axial (a) T1-weighted axial (b) T2-weighted coronary (c) and T2-weighted sagittal (d) MRI sections revealed a heterogeneous diffuse lesion affecting both cerebellar hemispheres and vermis. In the T1-weighted axial (e) and coronary (f) sections after contrast administration, the lesion had minimal and heterogeneous staining.
Medulloblastoma is rarely seen in adulthood and in most cases it is in the desmoplastic type with well-circumscribed mass. However, there are a few case report of MB that has infiltrative character mimicking ischemia, infection or demyelinating diseases in literature such as in our case [6,7]. Savardekar et al [6] reported such 2 cases, and Tuzgen et al [7] another one case. In the cases by Savardekar et al [6], the lesions mimicked Lhermitte-Duclos disease with their tiger stripped pattern. In the case reported by Tuzgen et al [7], there were separate lesions in each cerebellar hemisphere.
In our case, the treatment was delayed because of misdiagnoses as ischemic, infectious or demyelinating diseases, and operation and histological diagnosis could be performed 3 months later. In such cases, MRS may be useful for differential diagnosis. A malignancy was thought by MRS study in our case and the cases reported by Savardekar et al [6].
In conclusion, medulloblastoma in adults may cause a typical appearances with diffuse infiltrating lesions on radiological investigations. In such situations, MRS may help to differential diagnosis. In the adult cases with infiltrative and/or multifocal cerebellar lesions causing mass effect, the histopathological diagnosis should be made without delay.


