Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
*Ludmil MARINOV MD
Received: August 17, 2017; Published: August 29, 2017
Corresponding author: Ludmil MARINOV MD, General Surgery Consultant, GHER, Reunion, France
DOI: 10.26717/BJSTR.2017.01.000308
After the introduction of laparoscopy as a method of choice for cholecystectomy, the amount of the biliary injury of the main bile duct has raised significantly. Primary cause for this is complicated cholecystitis with gallstone impacted in theHartmann’s pouch, also known as Mirizzi syndrome.
The chronic complications of symptomatic gallstone disease, or Mirizzi syndrome, are named after Dr.Pablo Luis Mirizzi [1], an Argentinean surgeon who first performed intra-operative cholangiography in 1931 to obtained visual impression of the bile duct tree, and who in late 1948 described chronic complications of gallstone cholecystitis. Till the end of the 80’s the laparotomy is the main method for treatment of gallbladder stone decease. The introduction of mini invasive methods makes laparoscopy the first choice. But in 1, 5% [2] of the cases, predominantly in Mirizzi syndrome, the laparoscopic operation became the main reason for the increase of iatrogenic irrevocable injury of the main bile ducts. This, on its own, requires laparotomy and performance of bilio-digestive anastomosis, which significantly compromises the laparoscopy.For this reason we need to perform preoperative imaging diagnosis and to precise the options to perform save laparoscopic Cholecystectomy in complicated cases.
Mirizzi syndrome is a chronic complication of impacted gallstone, usually more than 10m min diameter at Hartmann’s pouch of the gallbladder. This provokes obstruction of cystic duct followed by dilation of gallbladder, chronic inflammation of the wall and forming of intraluminal pressure with influence on the stone. Under this pressure the impacted stone presses the bladder’s tissues surface of contact and provokes anatomical inflammatory changes at triangle of Callot’s normal anatomy such as:
a. Shortening of distance between cystic duct and common hepatic duct and compressing of the impacted stone on the wall of CHD with stenosis and mechanical jaundice.
b. Dilation, shortening and disappearing of cystic duct, with protrusion of stone in the lumen of CBD
c. Forming of large fistula between gallbladder and CHD.
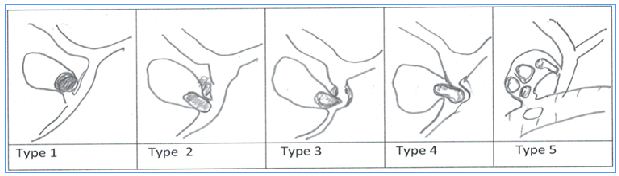
Figure 1: Variation of Mirizzi syndrome: Type 1- Biliary stone impacted in Hartmann’s pouch with compression on the CBD. Type 2- fistula between gallbladder and CBD, and stone obstructing third of the duct. Type 3- fistula between GB and CBD? With obstruction more than two third of CBD.Type 4- fistula between GB and CBD with total obstruction of CBD.Type 5- Fistula between GB and CBD, and second fistula between GB and D1. (GB –gallbladder; CBD- common bile duct; D1-first part of duodenum).
All of the cited before with formation of perihilar inflammatory plastron and abscess. All of those stages of Mirizzi syndrome may compromise the laparoscopic surgery (Figure 1).
According to SAGES, for safe cholecystectomy strategy every surgeon needs to use:
A. The Critical view of safety (CVS) [3].
B. Consider an Intra-operative Time out during laparoscopic cholecystectomy prior to clipping, cutting or transecting any ductal structure
C. Understanding the potential for aberrant and variant anatomy
D. Use of cholangiographyor to image the biliary tree intraoperatively before cutting [4],
E. Recognize when the dissection is approaching a zone of significant risk and halt the dissection. Finish the operation by a safe method other than cholecystectomy.
F. Get help from another surgeon, when the dissection or conditions are difficult.
Mirizzi syndrome in its variations poses the biggest questions now: is the criteria for safe laparoscopic cholecystectomy helpful and what else may be recommended?
For the last 2 years, we have performed in our clinic 176 laparoscopic cholecystectomies with 17 cases of Mirizzi syndrome, staged as: (Table 2).
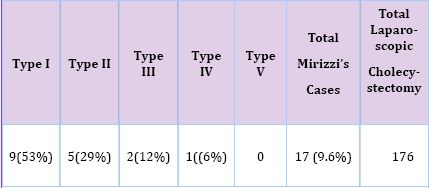
Table 1: Number of cases with Mirizzi syndrome.
In three cases, 2 of type II and 1of type III, the CBD was clipped and cut off. Biliary injury was noticed after switching to laparotomy in 2 patients, who obtained biliodigestive reconstruction with Roux-Y jejunal loop.In the third case it was found after 24 hours, postoperatively, after biliary IRM for mechanical jaundice.
In another 6 cases, after difficult dissectionwas performed the fallowing steps [5] to present real hilar anatomy:
a) Gallbladder aspiration
b) Antegrad gallbladder dissection just to Hartmann’s pouch
c) Opening of gallbladder and extraction of impacted stone
d) Intra-operative cholangiography
e) Mobilization of rest of gallbladder with presentation of cystic duct and clipping
f) Or maximal reducing of gallbladder in fundibulum and clipping
In 4 of patients with Mirizzi syndrome and formation of large sub-hepatic inflammatory plastron we converted to laparotomy.
Laparoscopic cholecystectomy appears to be the best approach for stone cholecystitis, but needs to be performed precisely for complicated cases such Mirizzi syndrome before clipping and cutting. Preoperative Biliary IRM is mandatory if suspicion for Mechanical obstruction. Using of different maneuvers to expose cystic duct- common hepatic junction is important.


