Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Abigail Mitchell1*, Kayla Limardi2 and Meredith Chamberland2
Received: January 12, 2018; Published: January 23, 2018
*Corresponding author: Abigail Mitchell, DHEd, MSN, RN, CNE, FHERDSA, Director of Grad Nursing, D’Youvill College, Buffalo, New York, USA
DOI: 10.26717/BJSTR.2018.02.000686
The prevalence of inpatient falls on medical/surgical floors is of great concern among many hospitals. Research has shown that up to 15% of hospitalized patients fall at least once during their hospital stay [1] identifying an immediate need for nursing intervention. The purpose of this quality improvement project was to create a new fall risk tool to specifically help nurses on medical/surgical floors assess their patients, identify each patients risk score per shift, and implement proper fall precautions based on the determined scores. Faye Glenn Abdellah’s theory served as the theoretical framework for this study.
The number of falls that occur during acute care in hospitalized settings is alarming. The predominance of inpatient falls on medical/ surgical floors negatively affects patient outcomes resulting in serious injury, prolonged debility, and increased length of stay in the hospital. “Falls are the most frequent cause of unintentional injuries in elderly people (aged > or = 65years), and are the leading cause of emergency admission loss of functional ability, independence, quality of life, and injury-related death”. Fall risk assessments and interventions to prevent falls needs to be a priority in nursing care. Several factors can influence a patient’s risk for falls such as decreased cognitive function, being introduced to an unfamiliar environment, medications, medical equipment, etc. In most cases, inpatient falls can be prevented and nurses need to be proactive in recognizing the risk factors and implementing appropriate fall precautions. Recognizing these risks specific to medical and surgical patients and developing a fall risk assessment tool for the nurses to use that include those risks may have a positive effect on the rate on inpatient falls on the identified units.
By comparing scores of the Morse Fall Risk tool and the newly designed fall risk tool of patients that fell on adult in-patient medical/surgical units, will the newly designed fall risk tool be more accurate at determining the risk?
This quality improvement program sought out to aid the medical/surgical unit nurse in using a newly designed fall risk assessment tool in addition to the Morse Fall Risk tool to determine the level of risk for each patient. Staff nurses on medical/ surgical units were educated on the use of the new fall risk assessment tool, and the reminder to still use the Morse Fall Risk tool the hospital is currently using. When patient falls occur, the two fall risk tool scores will be compared to determine the accuracy of the fall risk for each patient. There is a strong need to keep patients safe during their hospital stay to avoid further complications that can even result in an easily preventable death.
Faye Glenn Abdellah served as the theoretical framework for this study. The twenty-one nursing problems theory developed by her inter -relates the concepts of health, nursing problems, and problem solving. Problem solving is an activity that is essentially logical in nature. The framework focuses on nursing practice and individualizing patient care, which is essential when implementing fall risk interventions for acute care patients. Abdellah’s theory provides a basis for determining and organizing nursing care. Nurses must get to know their patients to determine if and how they are at risk of sustaining a fall. By sorting out relevant data and information the nurse can best determine the severity of the patients fall risk. Based on the nurses’ assessment and gathered relevant information the nurse can then develop a therapeutic plan for the patient. The nurses’ plan should also include the patient and the family to involve them in the care.
Findings from the literature review suggest a lack of knowledge and urgency exist on the nurse’s part on inpatient medical/surgical floors related to the severe impact falls have on patients. The overwhelming numbers of falls that take place during admissions for acute care yield a need for additional interventions to prevent patient harm and extensive nurse education. The developed fall risk tool was specific to patients admitted to medical and surgical floors. Limitations: The Project Authors recognized the following project limitations: small samples size, this QI was a pilot for the medical/ surgical floors only, and the lack of knowledge by the lead nurses.
There is much to be said about the complexities and multifactorial components of falls within an inpatient hospital setting. It is clear that falls are a significant problem in older adults, with more than 800,000 patients are admitted to the hospital following an injury related to a fall each year, according to the Center for Disease Control and Prevention [2]. The literature also provides and expands upon many factors that contribute to falls, such as, chronic illness, cognitive status, polypharmacy, or cluttered rooms. Both intrinsic and extrinsic components are to blame for increasing patients’ fall risks. Those patients who are at higher risk for falls, according to the literature, may include one with a history of past falls, Parkinson’s disease, history of alcoholism, COPD, vertigo, cancer, and some socio-demographic characteristics as well.
Further in the research, the literature review discusses the importance of patient and staff involvement in the active prevention of falls, and what the outcomes are when a fall is actually sustained in terms of hospital costs. The tool that was used for comparison is the Morse Fall Risk Assessment Tool. Developed in 1985, the Morse Scale has been the standard assessment tool in many inpatient settings, and the current protocol at the facility where the quality improvement project takes place. Based on a study by Borikova et al. [3], it was concluded that “Based on several validation studies, the Morse Fall Scale [MFS] is recommended for the identification of high fall risk patients. However, the predictive values of the MFS are not stable; they vary in different clinical conditions due to a number of factors”. It is imperative that the future of fall risk prevention is up-to-date and multifactorial.
The intended project setting was four inpatient Medical-surgical units in a small hospital in Western New York. The patient census on each unit is usually around 20 patients, with about 6 nurses per unit, per shift. The intended project population was adult (>/= 18 yrs. old) patients on medical-surgical units with a wide variety of surgeries, diseases, and co morbidities.
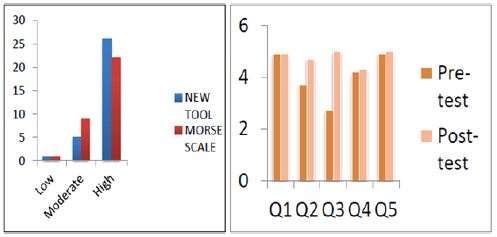
The quality improvement project was developed based on an extensive review of literature regarding inpatient falls, specifically on medical/surgical floors. Upon receipt of Full Approval from Hospital’s Institutional Review Board (IRB) and College’s IRB the research was able to commence. For each documented fall, the patients’ scores for both the Morse Fall Risk Scale and the New Fall Risk Tool were recorded. The scores for each tool were then compared to see what fall risk category (low, moderate, and high) applied to each patient. For each nurse that participated in using the new fall risk assessment tool, a pre- and post-test was completed. The questions included nurse’s opinions on fall prevention being a priority, usability of both Morse and the New fall risk tool, accuracy of both tools, responsibility relating to falls, and openness to new fall prevention tools. Each question was given a score of 1 (strongly disagree) to 5 (strongly agree), with a 5 showing a positive attitude on fall-related topics. The pre- and post- test scores were then compared to see how nurse’s attitudes have changed related to fall prevention on the unit since using the new fall risk tool.
The purpose of this project was to develop a new Fall Risk Assessment Tool that would hopefully be proven to be more accurate at determining falls for inpatients on medical/surgical units. The Fall Risk Tool consisted of risk criteria scoring based on findings obtained from the review of current evidence-based literature.
The participants in the study included RN’s that met the following criteria: Graduated from a registered nurse program, have one or more years of experience as a medical/surgical nurse, and used the newly designed fall risk tool after a patient fall. Recruitment of RNs that met the criteria started September 2017 and continued until the end of October 2017. Recruitments of RN’s into the study were provided with a brief description of the study and asked to participate. Implied consent was utilized. All RNs were provided a letter explaining the purpose of the study and requesting their participation. RNs that chose not to participate did not have to do so and returned the incomplete questionnaire to the investigators. The nurses who completed the survey were not compensated nor did they receive any benefits or gifts. All participation was voluntary.
There was no physical risk, psychological risk, economic risk, or legal risks. All participation was voluntary and there were no professional repercussions for not participating in this study. Participants were provided with a survey to be completed and returned to a designated secured area. Pre-survey data collection for the nurses also began September 2017 and continued until 25 nurses completed the survey. All responses were anonymous and no participant was harmed by participation in this study. Responses to the surveys were collected in a secure envelope by the researches and placed in a locked drawer at the researchers’ home to ensure anonymity. These surveys will be kept in this secure location for 3 years after the completion of the study and then destroyed.
For each documented fall, the patients’ scores for both the Morse Fall Risk Scale and the New Fall Risk Tool were recorded. Of a total of 32 falls, the newly designed fall risk tool was more accurate at determining who was at high risk, putting 26 of them into the high risk category, where Morse scale only put 22 of them into the high risk category (Figure 1). For each nurse that participated in using the new fall risk assessment tool, a pre- and post-test was completed. The questions included nurse’s opinions on fall prevention being a priority, usability of both Morse and the New fall risk tool, accuracy of both tools, responsibility relating to falls, and openness to new fall prevention tools. Each question was given a score of 1 (strongly disagree) to 5 (strongly agree), with a 5 showing a positive attitude on fall-related topics. After evaluating the newly designed fall risk tool, the nurses’ higher scores on the post-test reflect a greater understanding of fall prevention, safety awareness, and benefits of the new fall risk tool in comparison to Morse Scale.
Figure 1: Results for Morse Fall Risk Scale and the New Fall Risk Tool.
The project highlighted the need for a more current, accurate and multidisciplinary fall risk assessment tool to decrease falls on inpatient, medical-surgical units. The purpose and intention of this project was to address a current gap in nursing and health related knowledge regarding the educational needs of fall risk assessment. Future projects and research should focus on exploring and examining more patient-specific risk factors. Furthermore, future research and projects should focus on nursing staff’s input and attitude related to fall prevention and interventions. To further prove the accuracy and validity of the new fall risk assessment tool, a consideration for an additional study implementing the new fall risk tool to compare the prevalence of falls before and after the implementation.


