Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Suomao Yuan1, Bin Wei2, Yonghao Tian1, Jun Yan1, Wanlong Xu1 and Xinyu Liu1*
Received: January 19, 2018; Published: January 29, 2018
Corresponding author: Xinyu Liu, M.D., Orthopaedic department of Qilu Hospital of Shandong University, Jinan, PR China
DOI: 10.26717/BJSTR.2018.02.000699
Discal cysts are uncommon causes of low back pain and radiculopathy. Due to the diversity of discal cysts was reported by about 50 case reports; we do not yet have a detailed understanding of their natural history, etiology or pathogenesis. Here, we report two unique discal cysts to give a new insight to our understanding of the pathogenesis of discal cysts.
Keywords: Discal cyst; Pathogenesis
Abbreviations: EHL: Extensor Hallucis Longus; MR: Magnetic Resonance; Gd: Gadolinium; SNRB: Selective Nerve Root Block
Discal Cyst is relatively uncommon intraspinal space-occupying lesion. It is named by Chiba in 2001, and it was thought that the cyst communicated with corresponding intervertebral disc [1]. The clinical manifestation is the same as lumbar disc herniation, which can be manifested as low back pain and lower limb radiative pain [1]. Due to the low incidence of the disease, it is easy to be misdiagnosed by clinicians who are not aware of this disease. At present, a large series report was rare and most of them were presented in case reports. As of the end 2017, there are no more than 120 cases reported. At present, the natural history of lumbar intervertebral disc cyst is not clear, and its treatment is still controversial. The author reported two cases of lumbar discal cyst confirmed by surgery and postoperative pathology. The discal cysts were excised by microlaminotomy. The diagnosis, clinical manifestation and treatment of these two cases were reported as follows.
The first patient was a 30 years old man. He is a welder. The patient had low back pain for two years before his visit to our clinics. His pain aggravated after fatigue and received no special treatment. Five months ago, after a slight lumbar sprain, the pain of right buttock suddenly appeared and radiated down to the right lower limb. The symptoms aggravated after the activity and relieved after rest. The patients received multiple courses of massage, traction, nonsteroidal anti-inflammatory drugs, steroids, and physical therapy which failed to relieve his symptoms. The pain was significantly increased in the past 1 week and the activity was obviously restricted. Physical examination revealed a weakness in the extensor hallucis longus (EHL) muscle and a mild sensory disturbance at the L5 nerve dermatome. Straight leg raising test was positive at 30° on the right leg and negative on the left side. The knee jerk was weak on the right side and normal on the left side. The preoperative JOA score was 7 points.
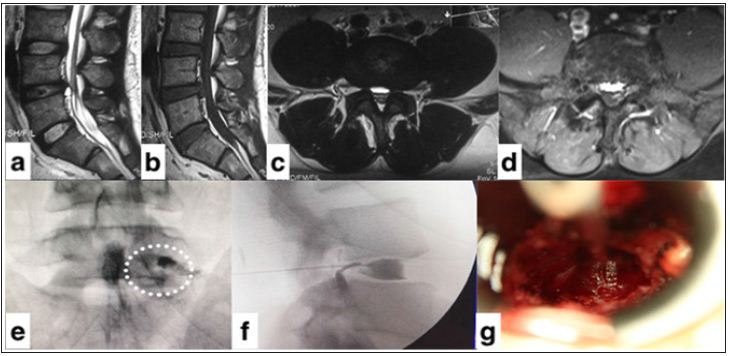
Magnetic resonance (MR) imaging in this patient demonstrated a 1.3cm cystic lesion immediately adjacent to the posterior right central L4-L5 intervertebral disk. MRI images reveals the cyst with low signal intensity on sagittal and axial T1-weighted images and high signal intensity on sagittal T2-weighted images (Figure 1a,1b,1c). This oval-shaped cyst showed a sub capsular fluid collection and the eriphery of the cyst wall was not enhanced with gadolinium (Gd) (Figure 1d). Before the surgery, the selective nerve root block (SNRB) was performed to clarify the responsible nerve root. Under radiographic guidance, a 22-gauge needle was punctured to the root of transverse process of L5 on the right side. 2 ml of mixture of 2% lidocaine and Iopromide was injected (Figure 1e) and infiltrated into spinal canal via intervertebral foramina of L5/S1 (Figure 1e).
The pain of lower extremity was completely relieved ten minutes after SNRB. The symptoms came back 2 hours later. Immediate before surgery, iodinated contrast material injected into the L4/5 intervertebral disc leaked into the cyst on the discogram (Figure 1f). A right partial laminectomy was performed at L4 and the lesion was excised. The dura and L5 nerve root were exposed after resection of the partial lamina of L4 and the ligamentum flavum. L5 nerve root was tense by exploration. A 1.5 ×1.5cm dark red cyst (Figure 1g) was seen underneath the right L5 nerve root after the nerve root and dural sac was retracted medially. L5 nerve root was compressed by the cyst obviously. There was no adhesion between the cyst and neural structures (Figure 1).
Figure 1: Sagittal T2-weighted (a), Tl-weighted (c) and axial T2-wighted (c) MRI showing a cystic mass below the L4/5 intervertebral disc. (d)The cyst wall was not enhanced with gadolinium (Gd). (e) The mixture of 2% lidocaine and Iopromide was injected and infiltrated into spinal canal via intervertebral foramina of L5/S1. (f) Iodinated contrast material injected into the L4/5 intervertebral disc leaked into the cyst on the discogram. (g) A 1.5 *1.5cm dark red cyst was seen underneath the right L5 nerve root after the nerve root.
The cyst wall was punctured using a scalpel. The outflow of serous bloody fluid was encountered, and the shrinkage of the cyst was obtained. The wall of the cyst was resected and sent for pathologic examination. The channel-like soft tissues adjoining the intervertebral disc were identified. Then, discectomy was performed at L4/5. Histologically, the cyst walls were constituted with dense fibrous connective tissues without cell linings and disc materials was found in it. The patient's radicular pain resolved immediately after surgery and only slight numbness overlying his left lateral leg was reported during the follow-up observation period of two years.
The second patient was a 27 years old man. He is a driver. The patient had low back pain after sudden lumbar sprain ten months ago. The sensory and motor function was normal at that time. The low back pain got a relief after taking Chinese medicine to improve the microcirculation. One month ago, the patient experienced the pain of right buttock radiating down to the left lower limb. The patient had severe pain (VAS, 9 point) in the lower limb and could not walk. The patient was treated with analgesic drugs without obvious effect. Physical examination revealed a mild sensory disturbance at the L5 nerve dermatome and normal motor function. Leg straight leg-raising test was positive at 50° on the left leg and negative on the right side. The knee jerk was normal and the ankle jerk was weak on both sides.
Magnetic resonance (MR) imaging in this patient demonstrated a 1.2-cm cystic lesion immediately adjacent to the posterior left central L4/5 intervertebral disk and central disc herniation of L4/5.MRI images reveal the cyst with low signal intensity on sagittal and axial T1-weighted images and high signal intensity on sagittal T2- weighted images. This oval-shaped cyst showed a sub capsular fluid collection and septum inside, and the periphery of the cyst wall was enhanced with gadolinium (Gd).
A light purple cyst was seen underneath the left L5 nerve root and was excised with the same technique as the first patients. The pathology showed the cyst walls were constituted with dense fibrous connective tissues without cell linings and disc materials was found in it. The symptoms were significantly improved and no symptoms recurrence was observed during the one year of follow- up.
The name of discal cyst is due to discographic (discogram) demonstration that the cyst is communicated with the corresponding intervertebral disc. However, they are not necessarily associated with extensive degenerative disease of the adjacent lumbar disc. There are some radiological characteristics, including ventral location, intimate or pedicled attachment to the annulus fibrosus, and absence of connection with a degenerative facet joint, helping distinguish discal cysts from other extradural cyst, such as ganglion cyst, synovial cyst, arachnoid cyst, ligamentum flavum cyst, etc. However, discal cysts demonstrate approximate epidemiological, clinical, radiological and pathological features to the other extradural cysts. Some authors suggested discography was not necessary for patients with radiographic evidence of disc- cyst communication [2].
Several hypotheses on mechanisms of pathogenesis have been proposed [1,3-6]. The bloody contents observed in almost 60% of reported cases as our two cases suggest that the cyst may be derived from epidural hematoma. The hematoma is assumed to result from hemorrhage of the epidural venous plexus caused by either disc herniation or an underlying disc injury by Chiba. The history of lumbar sprain in these cases was assumed to be the direct violence leading to blood vessel tears. However, that doesn't explain the origin of the cystic wall. The authors speculate that the hematoma comes from the rupture of blood vessels supplying the posterior annulus fibrosis, but not from the rupture of Batson's plexus. The existence of epidural membrane [7], which is a fibro vascular sheath lying external to the dura lining the vertebral canal and penetrated by Batson's plexus in many places, is a natural barrier to prevent more bleeding and is also the source of cystic capsule.
As for the color of the cystic content, it is more likely related to the time length of cyst formation, since the hemosiderin can be self-absorpted along the time. The associated disc herniation may explain why nucleus pulposus or cartilage was found in cyst contents in some patients like our two cases. Our last suggestion is that resection of the cyst and discectomy was sufficient to prevent recurrence. However, longer follow-up is needed to better evaluate this approach.


