Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yao Yongzhong*1,2, Shi Xianbiao1, Zhao Yixin2, You Xin2, Wang Jingmei3, Yu Huiping3 and Wang Shouju*4
Received: January 23, 2018; Published: February 02, 2018
Corresponding author: Wang Shouju, Department of Medical Imaging, Jinling Hospital, School of Medicine, Nanjing University, Nanjing, 210000, China
DOI: 10.26717/BJSTR.2018.02.000720
Invasive cystic hypersecretory hyperplasia (CHH) of the breast is very rare. The clinical manifestation of CHH iscystic masses, and it is not easy to determine its biological characteristics before an operation. A 54-year-old female patient was admitted with a cystic massin the left breastfor one week. After the operation, the pathology diagnosis was invasive CHC, and the postoperative period was uneventful.
Keywords: Invasive Cystic Hypersecretory Carcinoma (Chc); Breast Cancer; Breast-Conserving Surgery; Palpable Mass
Abbreviation: CHH: Cystic Hypersecretory Hyperplasia; CHC: Cystic Hypersecretory Carcinoma; TG: Thyro Globulin; TTF-1: Thyroid Transcription Factor-1; GATA3: GATA binding protein 3; ER: Estrogen Receptor; PR: Progesterone Receptor; HER-2: Human Epidermal growth factor Receptor-2
Cystic hypersecretory lesionsof the breast are uncommon. Theyhave a spectrum of morphological features ranging from cystic hypersecretory hyperplasia (CHH), CHH with atypia, cystic hypersecretory carcinoma (CHC) to invasive CHC. There have only been a few cases of invasive CHC reported in the literature. We are reporting an additional new case of a 54-year-old female who had a palpable mass in her left breast for one week. A local excision of the massand breast-conserving surgery with sentinel lymph node biopsy was performed successively and pathology diagnosis of invasive CHC was made. The postoperative period was uneventful.
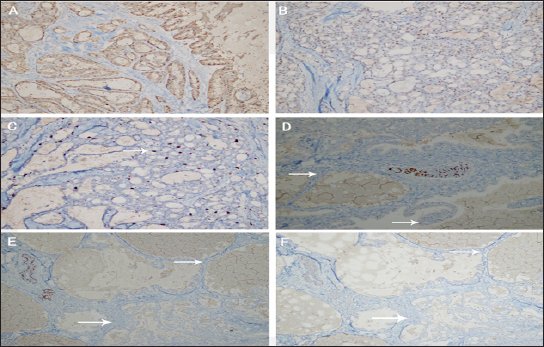
A 54-year-old postmenopausal woman presented with a cystic mass in the left breast for one week. Physical examination disclosed the breast lump was located in the lower outer quadrant, which was 5cmx 2cm, indolent, mobile, ill-defined, hard, with no nipple dischargeand retraction of nipples. Breast ultrasound showed a lobulated cystic-solid (mainly cystic) mass (Figure 1). Fine needle aspiration biopsy ofthe breast lump was done, and the smear showed a large number of tissue cells and a small amount of glandular epithelial cells with uniform size, which suggest consideration for cystic lesions. The patient and her family had no history of breast disease previously. Since the evidence from the fast pathological examination was not strong enough to diagnose this breast lump as malignant, the patient underwent local excision of the mass at first. Four days later, the result of the routine pathological examination was reported. Grossly, the cut surface revealed a 2.5cm x 2cm x 2cm tumor which showed multiple cystic as a honeycomb, and the cysts were filled withgelatinous secretions.Microscopically, the tumor showed a varied histological pattern with cysts, microcystic and solid structure, the tumor cells were in the same shape, the mitosis was rare, and eosinophilic secretions were found (Figure 2). Histo chemical staining showed the cystic contents were filled with PAS-positive dense eosinophilic material resembling thyroid colloid. However, the contents of the cyst were negative for thyroglobulin(TG) and thyroid transcription factor-1(TTF-1). The expression of S-100(Figure3A), GATA binding protein 3 (GATA3) and estrogen receptor(ER) was positive in tumor cells, while the expression of progesterone receptor(PR) and human epidermal growth factor receptor-2(HER-2) was negative (Figures 3B & 3C).The cells adjacent to tumor were negative in expression of P63 and calponin (Figures 3D-3F), which suggests myo epithelial deficiency that considered as invasive lesions. Taken together, the diagnosis is likely to be invasive CHC, thus breast-conserving surgery with sentinel lymph node biopsy was performed successively. The pathological examination post-surgery showed the sentinel lymph nodes were free of tumor metastasis. Then the patient underwent subsequent radiotherapy. The three-month follow-up of the postoperative period was uneventful.
Figure 1: Breast ultrasound showed a lobulated cystic-solid (mainly cystic) mass.
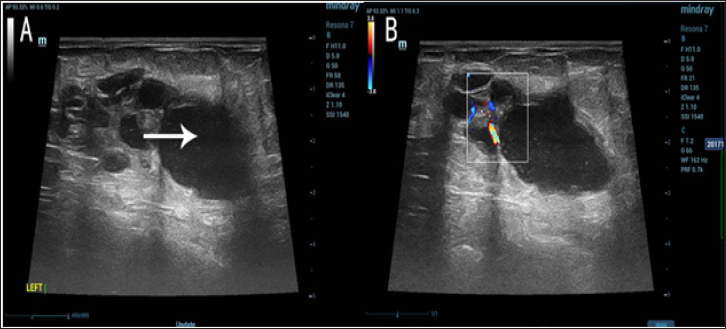
Figure 2: Microscopically, the tumor showed a varied histological pattern.
a. Cystic structure(white arrow),
b. Eosinophilic secretions(white arrow), Papillary structure(red arrow),
c. Microcystic structure(white arrow),
d. Microcystic structure and cystic structure(white arrow).
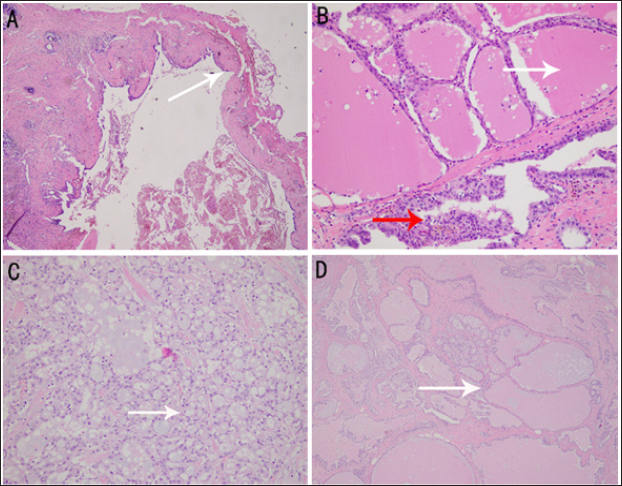
Figure 3:Immunohistochemistry of the tumor showed the invasive CHC characters.
a. Tumor cells positively expressedS100,
b. Tumor cells positively expressed ER,
c. Tumor cells positively expressed Ki67 (10%),
d. Normal breast tissue positively expressed P63, but the cells adjacent to tumor are negative(white arrows),
e. Normal breast tissue positively expressed P63, but the cells adjacent to tumor are negative(white arrows),
f. Normal breast tissue positively expressedcal ponin, but the cells adjacent to tumor are negative (white arrows).
Cystic hypersecretory lesions, which include CHC and CHH, were first described by Rosen PP and Scott M in 1984 [1]. The main difference between CHH and CHC is the biological characteristics of epithelial cells. The epithelial cells in cystic hypersecretory lesions may appear atypical and the structure change. When the epithelial cells are benign, the lesion is considered to be CHH; when the atypical character and structure change of epithelial cells reach the diagnostic standard of carcinoma in situ, the lesion is diagnosed as CHC.CHC is a rare subtype of intraductal carcinoma of the breast, which has the characteristicof polycystic structure of varying sizes containing gelatinous materialand dilated cystic duct containing eosinophilic secretions. However, the majority of cases reported in the literature are in situ cancers, CHC with obvious infiltration characteristics has been reported rarely [2-4]. Typically, the CHC presents as a palpable lump without pain or tenderness and rarely manifests nipple discharge [5].
This patient presented with a palpable lump in the left breast without nipple discharge and pain. Fine needle aspiration biopsy and fast pathological examination showed there was no significant evidence of malignant, so the patient underwent local excision first. When the fine needle aspirate only sampled the secretion in cyst with no epithelial components of hetero morphic type, it is easy to misdiagnose the cyst as benign lesion [6]. Therefore, it is necessary to arouse the vigilance of the doctors. In our experience, if the cells around the tumor were negative in the expression of P63 and calponin (both are markers of myoepithelial deficiency), the diagnose of invasive CHC could be safely excluded. Until now there is still no standard regime of chemotherapy for this particular type of breast cancer, but in general, it should be treated in accordance with other common duct cancer. Meanwhile, there are different opinions about the prognosis of CHC. D'Alfonso TM [7] consider that CHC has an inert biological character. But once became invasive, the infiltrating component of CHC tends to transform into high-grade cancer. In this patient,thetumor was ER (+), PR (-),HER-2(-) and Ki67(10%+), and there was no in situ carcinoma, thus the degree of malignancy is not very high, it was very uncommon performance of invasive CHC. Therefore, the patient was uneventful in the three- month follow-upafter breast-conserving surgery and adjuvant radiotherapy.
This work was supported by the grant from the Nature Science Foundation of China (NSFC 81372294 and 81501588).


