Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Amro S El sayed and Ahmed Ibrahim Zayda*
Received: February 23, 2018; Published: March 06, 2018;
*Corresponding author: Ahmed Ibrahim Zayda, Orthopedic Surgery Department, Faculty of Medicine-Menofia University, Shebin Al-Kom, Menofia, Egypt
DOI: 10.26717/BJSTR.2018.02.000823
Objective: To assess the effectiveness of repair of chronic ruptured Achilles tendon by V-Y Plasty and plantaris tendon augmentation.
Background: Treatment of chronic Achilles tendon rupture is still a challenge for most orthopedic surgeons. It is different from the acute Achilles tendon rupture as there are large gaps that will be bridged by scar tissue and muscle becomes infiltrated with fat, so ankle will be weak affecting the gait. Several techniques for reconstruction of Achilles tendon have been described, including tendon graft, turndown flap, and flexor hallucis longus augmentation and augmentation with synthetic materials. The superiority of one technique over another has not been demonstrated.
Patient and Method: This retrospective study included nine patients with chronic Achilles tendon rupture who underwent surgery in our institution, between February 2013 and April 2016. The study group consisted of 7 male and 2 female, ranging in age from 28 to 52 years old with mean age of 40 years. 6 cases were right side and 3 were left. All patients were diagnosed by clinical examination, sonographic examination and MRI. Treatment was by doing V-Y plasty of tendo-Achilles to cross large gaps with augmentation of repair by plantaris tendon in all cases.
Results: At the end of follow-up (range, 7-12 months), no major complications related to surgery occurred. No patient had re-rupture at any follow-up. All patients returned to their previous occupation. The Postoperative range of ankle movement equaled to that of the opposite side in 8 patients, but in one patient the ankle dorsi-flexion was 10° less than the contralateral side. All patients were able to stand on tip toes for 30 seconds at last follow up.
Conclusion: Several surgical treatment options were described for reconstruction of a neglected Achilles tendon rupture but without definite data that support one technique over another. Whatever the technique, the final goal of surgical treatment is to restore the length tension relationship to provide sufficient plantar flexion power. Treatment with V-Y plasty of tendo-Achilles to cross large gaps with augmentation of repair by plantaris tendon provides adequate surgical option with no major complications and no re-ruptures avoiding complications of tendon transfer.
Keywords: Chronic; Ruptured; Achilles Tendon; V-Y Plasty; Plantaris Tendon; Repair
Ruptures of the Achilles tendon cause marked impairment of the function of foot and ankle. The management of acute ruptures is debated whether operative or conservative [1,2], with a higher rerupture rate with conservative treatment than with operative [3,4]. The true frequency of acute Achilles tendon rupture is unknown but historically it was regarded as a rare injury comprising less than 0.2% of the general population [5]. However the incidence of Achilles tendon rupture increased markedly over the past decades, Nowadays it is the most common tendon to be ruptured in the lower extremity accounting for 40% of the operated tendon. The increased incidence of Achilles rupture may be attributed to increased interest with recreation sports in young adults as well as elderly and to better reporting [6-8]. The area proximal to insertion of tendoachilles on the calcaneal tuberosity is a vascular watershed area predisposed to degeneration and tears. This area was found to be about 2-6 cm proximal to the insertion. Repetitive micro-tears which exceed the body's regenerative capacity results into a trivial trauma causing complete tendoachilis rupture [9].
Acute rupture of the Achilles tendon can be easily diagnosed clinically by a physical examination, but incorrect early diagnosis can occur in 10% to 25% of acute rupture patients [10]. If 6 weeks elapses between trauma and time of diagnosis, it is classified as chronic tear [11]. Symptoms as swelling and pain may be masked in some patients with tendon rupture thus delaying diagnosis [11]. Chronic ruptures are normally managed operatively unless there are contraindications to surgery [12,13]. The chronicity of the lesion with great degeneration of neglected Achilles tendon rupture results in large gaps which make direct repair more difficult or even impossible; therefore, reconstructive surgery of the Achilles tendon is more desirable [14]. While several techniques for Achilles tendon reconstruction have been described, the superiority of one technique over another has not been demonstrated and optimal surgical management of Achilles tendon rupture remains controversial.
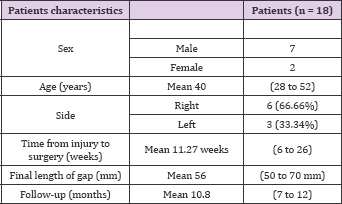
This retrospective study included 9 patients with chronic Achilles tendon rupture who underwent surgery in our institution, between February 2013 and April 2016. All patients, any age with neglected ruptured Achilles tendon more than 6 weeks were included in the study. We excluded all cases with infection at or nearby the Achilles tendon, cases with uncontrolled diabetes, malignant diseases as well as those with associated vascular or nerve injury and those with absent plantaris muscle. The study group consisted of 7 male and two female patients, ranging in age from 28 to 52 years old with mean age of 40 years. All cases had unilateral injury, 6 cases were right side and 3 were left (Table 1). The time lapse before definite treatment ranged from 6 to 26 weeks with mean 12.27 weeks. The etiology for chronic Achilles tendon injury was neglection in all patients.
All patients were diagnosed by clinical examination for a palpable gap or a change in the contour of the posterior aspect of the ankle, +ve Thompson test, is decreased planter-flexion power compared with the other healthy side, inability to perform a single limb heel rise and delayed heel-off and a shortened stride.
X ray was used for evaluation of the presence of avulsion fracture of the calcaneus, ultrasonography (US) to differentiate partial thickness tears or tendinosis from full-thickness tears [15], Magnetic resonance imaging (MRI) for assessing the amount of functional defect within the Achilles tendon for preoperative planning. The site of the rupture was 4-6 cm from the tendon insertion in os calcis measured in MR (Figure 1) The size of the gap was between 3-6 cm preoperative (mean 4.5 cm).
Figure 1: MR of ruptured Achilles tendon.
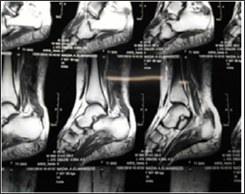
Figure 2: The planned incision of one case.

Figure 3: The gap of ruptured tendon after debridement.

Figure 4: Inverted V shaped incision of the tendinous portion of the proximal stump.
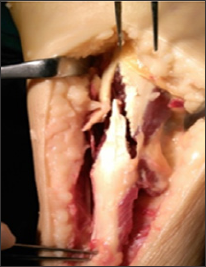
All cases were operated under spinal anesthesia, tourniquet was applied to the affected limb, postero-medial approach was used and centered over the site of the rupture (Figure 2). All scar tissues were debrided, keeping surrounding tissues and approaching healthy margins of the Achilles tendon, and exploration of plantaris tendon is performed. The gap between both ends was measured with the ankle at 30 degrees planter flexion after debridement and excision of scar tissues were 5-7 cm (mean 5.6 cm) (Figure 3). An inverted V shape incision was done in the proximal tendinous portion of the proximal stump; the length of the limb is 1.5 times the length of the gap (Table 1) (Figure 4). The proximal stump is pulled down, with the ankle in 30 degrees planter flexion and repaired to the distal stump with Krackow method using non-absorbable sutures (Demo-bond no 5). Then the plantaris was harvested using tendon stripper and used to augment the repair (Figures 5 & 6) Closure of the wound and above knee cast in 20 degrees planter flexion was applied.
Figure 5: The proximal and distal ends are repaired by Krackow method and plantaris tendon was harvested.

Figure 6: The proximal stumps are repaired to each other with Krackow method and plantaris used to augment the repair.

Table 1: Patients characteristics.
Post operative injection antibiotic for 5 days (Third generation cephalosporins 1 gm/twice daily). Patients were kept in planter flexion of the ankle up to 20 degrees in above-knee cast for 4 weeks. Oral anticoagulant till they returned back to their daily activities. After 4 weeks stitches were removed and cast was changed with below knee cast for 2 weeks with reduction of the planter flexion. Patients were allowed to start weight bearing with crutches after 6 weeks. Patients were followed regularly at monthly interval for the first 3 months and then every two months till the end of follow up. Follow up were for the wound condition and then for assessment of range of motion, walking strength and for development of complications. Seven patients were followed for 12 months whereas two were followed for 7 months, the mean follow up period was (10.8 months).
Physiotherapy was started at 6 weeks postoperative after cast removal to increase range of ankle movement and prevent reflex sympathetic dystrophy, the duration of physiotherapy ranged from 4 to 7 weeks with mean 5.5 weeks. The pre- and postoperative American Orthopedic Foot and Ankle Society (AOFAS) ankle- hind foot scores were used in patient evaluation with Clinical evaluations included assessment the ankle ROM and surgery- related complications. Comparisons between the preoperative and postoperative AOFAS score was performed with use of paired- sample t-tests significance level was set as P value < 0.05
In all patients the gaps were closed with adequate repair and the mean follow-up period was 10.8 months (range, 7-12 months), and no major complications related to surgery occurred. No patient had re-rupture at last follow-up. All patients returned to their previous occupation. Three patients had superficial wound infection that was treated successfully with dressing and antibiotic; only one case needed surgical debridement of the wound and finally healed with no major complications. The Postoperative range of ankle movement equaled to that of the opposite side in 8 patients, but in one patient the ankle dorsi-flexion was 10° less than the contralateral side. All patients were able to stand on tip toes for 30 seconds at last follow up. Mean AOFAS improved from 65° (range, 50°-80°) preoperatively to 91.5° (range, 88°-95°) at last follow-up. This difference was statistically significant (p value < .05).
Treatment of chronic Achilles tendon rupture is still a challenge for most orthopedic surgeons. It is different from the acute Achilles tendon rupture as there are large gaps that will be bridged by scar tissue and muscle becomes infiltrated with fat, so ankle will be weak affecting the gait. Several techniques for chronic Achilles tendon reconstruction have been described, including turndown flap, tendon transfer, tendon graft, and augmentation with synthetic materials [16]. In cases of neglected chronic tendo-Achilles ruptures, augmented tendo-Achilles repair provides stronger reconstruction and provides more biomechanical stability to the repair. Central gastro-soleus aponeurosis flap repair is superior to standard Kessler repair by virtue of its strength. Augmentation to the repair site allows earlier mobility, weight-bearing and a more aggressive rehabilitation program with reduction in the incidence of re-rupture for both acute and neglected Achilles tendon rerupture. Lo et al. [17] reviewed the literature on the treatment of Achilles tendon rupture and identified 742operative cases and 248 cases managed conservatively. The overall rate of re-rupture was 3% for those managed operatively and 12% for those managed non-operatively.
While the rate of re-rupture in the operative group was lower, the rate of minor and moderate complications associated with operative treatment was up to twenty times greater in some reports [18]. In our series we had no cases of re-rupture till now. Serder et al. [19] did a case report study with encouraging results regarding the repair of an Achilles tendon rupture using the partial Lindholm technique augmented by the plantaris tendon and thought that they need long-term studies of their technique using a higher number of patients should be performed to compare the stability, range of motion, wound healing, and time required to return back to sport activities [19]. Yangjing et al. [20] did a retrospective study in chronic Achilles tendon rupture but with augmentation with flexor haullcis longus tendon in 3 cases and had similar good results with low complications rate [20]. The main criticism of the V-Y plasty was alteration of the muscle to tendon ratio [18]. However in this study this technique enables us to overcome a large aseptic defect of chronic AT rupture as long as 7 cm with good functional outcome and low complication rate.
The small number of cases of the study and the relatively short follow up period are main limitation of this study also the wide spectrum of exclusion of patients with infection at or nearby the Achilles tendon, cases with uncontrolled diabetes, malignant diseases as well as those with associated vascular or nerve injury and those with absent plantaris muscle is a true limitation of this study.
Several surgical treatment options were described for reconstruction of a neglected Achilles tendon rupture but without definite data that support one technique over another. Whatever the technique, the final goal of surgical treatment is to restore the length tension relationship to provide sufficient plantar flexion power. Treatment with V-Y plasty of tendo-Achilles to cross large gaps with augmentation of repair by plantaris tendon provides adequate surgical option with no major complications and no reruptures avoiding complications of tendon transfer.


