Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sham Kishor Kanneppady*1, Sowmya Sham Kanneppady2, Anusha Rangare Lakshman3, Shishir Ram Shetty4 and Prasanna Kumar Rao5
Received: March 21, 2018; Published: April 06, 2018
*Corresponding author: Sham Kishor Kanneppady, Senior Lecturer, Division of Oral Diagnostics and Surgical Sciences, School of Dentistry, International Medical University, Kuala Lumpur, Malaysia
DOI: 10.26717/BJSTR.2018.03.000924
Abbreviations: OSF: Oral Submucous Fibrosis; CTGF: Connective Tissue Growth Factor; ROS: Reactive Oxygen Species
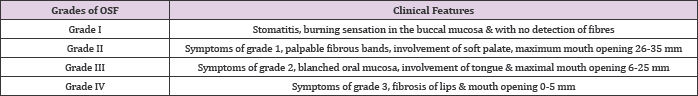
Oral submucous fibrosis (OSF) is a chronic, progressive, scarring, precancerous condition which is characterized by mucosal rigidity. It clinically appears as blanching of oral mucosa, which is usually associated with burning sensation. On palpation of the affected mucosa, clinician may elicit fibrotic bands. The other clinical signs and symptoms of OSF are vesicles, ulcerations, petechiae, melanoses, xerostomia and limitation in jaw movement [1,2]. It has been associated with long-lasting dipping of betel nut or paan in the mouth. Oral submucous fibrosis predominantly occurs in Indians and Southeast Asians. This condition is more common in young adults, aged 20-40. The most frequently affected sites in the oral cavity are buccal mucosa, retromolar area, tongue and soft palate. Mehrotra highlighted clinical grading of the disease as follows [3] (Table 1).
Table 1: Clinical grading of OSF.
The areca nut alkaloid arecoline is now identified as the principal causative factor for OSF. Effects of arecoline in the pathogenesis of OSF include fibroblastic proliferation and increased collagen formation. Many studies had been performed so far in order to find out the exact mechanism of arecoline in collagen metabolism. Connective Tissue Growth Factor (CTGF) is associated with the onset and progression of fibrosis in many human tissues. In an attempt to analyze the expression of CTGF in OSF, it was found that CTGF was present in fibroblasts and endothelial cells in all the OSF cases included in the study. It was further shown that arecoline stimulated CTGF synthesis in a dose- and time-dependent manner in buccal mucosal fibroblasts through reactive oxygen species (ROS), NF-kappa B, JNK and p38 MAPK pathway. In the meantime, many studies have shown that NF-kappa B, JNK and p38 are strongly activated by ROS and thereby it is suggested that ROS elicited by arecoline may play important roles in NF-kappa B, JNK, P38 activations and subsequent CTGF expression. It was hypothesized that Overexpression of CTGF may enhance the fibrotic activity in OSF and thereby play a role in the pathogenesis of OSF. Unlike TGF P, CTGF is only produced by hepatic stellate and kidney mesangial cells in adults under normal conditions, therefore it may be used as a novel target for developing anti-fibrotic therapy in treating OSF. Inhibition of CTGF will block the profibrotic effects of TGF-β, without affecting its anti-proliferative and immunosuppressive effects [4].
The malignant potential of OSF was first described in 1956 by Paymaster and the rate of which has been estimated to be 7-13% only recently. Many follow up studies had been conducted so far in order to identify the important aspects in malignant transformation of OSF [5]. Recently it has been proposed that oral cancers arising in OSF constitute a clinico-pathologically distinct disease, the differences of which believed to arise from differential mechanisms of areca nut carcinogenesis. One study recognized that most of these patients are younger males with better prognostic factors such as better grade of tumour differentiation, lesser incidence of nodal metastases, and extra capsular spread [6]. It was proposed that clinical presentation and behaviour have a wide spectrum. Minority of cases during the process of transformation show large Exophytic lesions which are clinically typical OSCC without showing any histological evidence of invasion [7].
Primordial Prevention: Educating the masses that the consumption of tobacco, areca nut and its related products is a key factor in the development of OSF.
Primary Prevention:
a) Restriction of the habit: Patients should be counselled about the disease, its complications and the need of abstinence from chewing areca nut and tobacco. Elimination or even reduction of the habit of tobacco and areca nut chewing is an important preventive measure.
b) Minimizing consumption of spicy foods and maintaining proper oral hygiene.
c) Supplementing the diet with foods rich in iron, vitamins A, B complex, and C.
Secondary Prevention: Early diagnosis can be made by self-assessment of one's own oral cavity in mirror and reporting immediately to the nearest medical or dental practitioner if any abnormality is detected. The doctor will diagnose the patient clinically with above mentioned criteria.
Medical Treatment: There is a dizzying array of reported medical interventions to improve current treatment regimens for OSF. The patients should be given nutritional support in the form of dietary supplements rich in protein, calories, vitamins and minerals. These are commonly employed in combination with other more specific therapeutic agents like immunomodulatory drugs. Local and systemic application of glucocorticoids, placental extract and hyaluronidase are commonly used. They act by inhibiting the action of sensitized lymphocytes following activation by specific antigens and by preventing or suppressing inflammatory reactions. The effects of steroids and hyaluronidase are thought to be responsible for the satisfactory results obtained in OSF patients who have severe limitation in mouth opening. Placental extracts (aqueous solution of human placenta) in the form of local injections as well as in parenteral form have been tried with varied results.
They can be separated into four different fractions: aqueous extract, lipoid extract, immune gamma globulins, and tissue coagulants. Only the aqueous extract of placenta acts as a biogenous stimulator-by accelerating cellular metabolism (through the pituitary-adrenal cortical axis), assisting in the absorption of exudates, stimulating the regenerative process, and increasing the physiological actions of organs. The other actions of placental extract are an anti-inflammatory and significant analgesic effect, increase in blood circulation and tissue vascularity and arrest of tissue growth stagnation. Placental extract has been found to contain between 50 and 100 KA units of alkaline-phosphatase and it has been used as a local nutrient. Combination therapy has shown better therapeutic efficacy for medical management of OSF. Local injections of chymotrypsin, hyaluronidase and dexamethasone together yielded significantly better results than with one drug alone or a combination of dexamethasone with either chymotrypsin or hyaluronidase. Combined therapy with nylidrin hydrochloride (a peripheral vasodilator), vitamins D, E and B complex, iodine, placental extract, local and systemic corticosteroids, and physiotherapy claims a success rate of 62% in OSF.
Surgical Management: Surgery remains a therapeutic option in advanced cases of OSF which are refractory to conventional conservative therapies. Historically attempts to excise the fibrotic bands has resulted in progressively more scarring in follow-up periods resulting in worse quality of life for the patients. In recent years attempts have been made to replace the defects created by excision by split thickness skin grafting, bilateral nasolabial flaps, palatal island flaps, tongue flaps, buccal fat pad graft and temporalis muscle flap graft. A new treatment regimen composed of surgical excision of the fibrotic bands with submucosal placement of fresh human placental grafts, followed by local injections of dexamethasone was recommended recently for advanced cases. The rationale for using placental grafts in OSF is that they have both a hormonal and a mechanical effect; the biogenic stimulant effect is because the placenta is a homograft that is immunologically competent and rich in steroids, proteins, chorionic gonadotrophins, estrogens and progesterone. The grafts are easily moldable and undergo total absorption only after prolonged periods, thus mechanically preventing fibrosis.
Physiotherapy and Rehabilitation: Physiotherapy exercises remain undoubtedly the basic, most commonly performed and the modality with longest therapeutic effect on relieving the trismus. This has been used in combination with other medical therapies and surgical procedures.
A thorough knowledge on various oral precancerous diseases will help clinician to make appropriate diagnosis and plan the treatment. Oral submucous fibrosis is mainly associated with areca- nut chewing. Thus, health education counselling the individual and behavioural therapies especially the younger generation is most successful approaches of prevention at a primary level.


