Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Anita Syla Lokaj* and Blerta Rama
Received: March 25, 2018; Published: April 11, 2018
*Corresponding author: Anita Syla Lokaj, Department of Ophthalmology, University Center Clinic of Kosova, Prishtina, Kosova
DOI: 10.26717/BJSTR.2018.03.000952
Back ground: Lacrimal gland Adenocarcinoma is very rare tumors and highly aggressive.
Methods: A 86-year-old woman presented with a 5-month history of a painless mass in the right upper outer eyelid. The clinical presentation, workup, surgical approach, and pathological findings were reviewed.
Results: Excision biopsy was performed to confirm diagnosis. Exoneration was undergone and follows up further to oncology department.
Conclusion: Tumors of Lacrimal gland are highly aggressive tumor but fortunately these kinds of tumors are very rare. In some invasive cases complete excision including exoneration with adjuvant radiotherapy and chemotherapy is highly recommended.
Keywords: Lachrymal gland; Adenocarcinoma NOS; Neoplasia; Exoneration
Lacrimal gland tumors with epithelial origin are very rare tumors and accounts about less than 5% of all biopsied orbital lesions [1]. The lacrimal gland is considered in some ways to be a type of minor salivary gland that shares histological features with the major salivary glands. But the many study shows that, lacrimal gland tumors and major salivary gland tumors are similar[2].Until recently, primary Adenocarcinoma of the lacrimal gland were not further sub classified, but they can now be divided into low-grade and high-grade malignancies. The most tumors of lacrimal gland are in epithelial origin, constituting approximately 50-60% of all benign tumors and 40-50% of all malignant tumors [3]. Approximately of 20 % of all lacrimal gland benign tumors it is appropriate by pleomorphic adenoma. Malignant tumors of lacrimal gland are very rare, but very aggressive and the most common form is adenoid cystic carcinoma. In the group of malignant tumors there is also inserted an unspecified group that numbers about 5 to 10 percent of very rare malignant tumors called Adenocarcinoma not otherwise specified (NOS)[3].In the absence of definitively of special morphologic features, histopathological and imunohistochemica fenotipisation as in our paper not otherwise specified Adenocarcinoma was made. In this case report we present an update on these different tumor types with regard to their clinical presentation, histolopathology findings, imunohistochemica results and the best state treatment strategies for this rare tumor and more heterogeneous group of diseases [4].
Figure 1a: Stage when patient come in clinic.

An 86-year-old woman was referred to our clinic with a history of progressive, painless swelling over the right upper eyelid, for the past 5 months (Figure 1). In this region of masses was present an ulcerated swelling (Figures 1 & 3). Initially the tumor was too small but it was rises very rapidly (Figure 2). There were no systemic symptoms including loss of appetite, loss of weight, fever or a headache. No significant medical, surgical or family history could be elicited (Figures 2 & 3). An MRI of ocular area revealed a 45x40x35 mm solid mass in the upper eyelid with infiltration of rectus muscle but there was no extraconal, intraconal, intraocular, intracranial or paranasal sinus involvement. No bony erosions were noted (Figure 4) MRI.
Figure 1b: Proifle view of tumor.

Figure 2: Inicial stage before 6-month.

Figure 3: Ulcerated mass.

In the appearance of the tumors we increase the suspicion about Merkel cell carcinoma so we decided to do incision biopsy throw upper eyelid to confirm diagnosis (Figure 5). Biopsy from the eyelid revealed a poorly differentiated carcinoma of epithelial origin with infiltrative neoplastic islands of epithelial malignant cell. The neoplastic cells were large polygonal cell with vesicular nuclei, prominent nucleoli and amphophylic cytoplasm. But to make tumor phenol typing it was necessary to do immuno histo chemistry examinations. On immuno histo chemistry examination, cyto keratin 7 was positive, whereas cyto keratin 20 turned out to be negative. Based on histological analysis and immuno histo chemical results we can concluded in poorly differentiated Adenocarcinoma of lacrimal gland (grade 3).T Merkel cell carcinoma is excluded because of the phenotype CK20, CD56, Chromogranin A. She underwent an orbital exoneration under general anesthesia without any complications and instructed to oncology department for further treatment with radiotherapy and chemotherapy.
Figure 4: An MRI scan of the ocular space revealed a 45*40*35 mm, malignant tumor on the right upper eye lid and lacrimal gland.
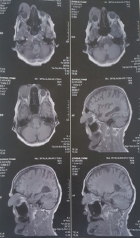
Figure 5: During operating day.

Lacrimal gland fossil lesions may be divided into four categories: Inflammatory, lymph proliferative, epithelial lesions and metastatic tumors [5]. Out of epithelial lesions 55% are benign and 45% are malignant [6]. It is known that approximately 50% of lacrimal gland lesions are originated from epithelial elements and 50% are of none epithelial origin [5]. Epithelial tumors of the lacrimal gland are divided into low-grade and high-grade malignancies [7]. Among the malignancies, most frequently present is adenoid cystic carcinoma (66%), followed by a carcinoma-ex- pleomorphic adenoma (18%), primary Adenocarcinoma (9%), and at least mucoepidermoid carcinoma (3%) [6]. Patient with glandular lacrimal is Adenocarcinoma are associated with upper eyelid mass production which might be accompanied by symptoms such as exophthalmoses, pseudoptosis, dystopia, and in advanced disease or reduced visual acuity [8]. However, the duration of the symptoms before first ophthalmic examination can vary; where for patients with pleomorphic adenoma is approximately 2 years, slow-growing tumors can persist up to 20 years, adenoid cystic carcinoma is approximately 6 and months and other malignant tumor can persist is typically less than a year [9]. Painless or late clinical featured pain in the upper eyelid appears commonly for the Adenocarcinoma patients comparing to the other malignant subtypes [10], explaining neglected approach of the patient toward this disease and delayed decision for ophthalmology consultation like our patient case.
This clinical features and patients history can lead into wide range of differential diagnosis of lacrimal gland lesions and also eyelid malignant tumors. Therefore our initial approach was suspicion of the Merkel cell carcinoma basing on the eyelid mass protrusion. Meanwhile we followed other suspicions of the lacrimal gland lesions knowing other lacrimal glandular epithelial tumors, lymphoid tumors, inflammatory diseases and miscellaneous diseseses involving the lacrimal gland like trachoma, granulocytic sarcoma, neuro fibroma [11]. To make the final diagnosis incision biopsy was made; where immuno histo chemical results revealed Lacrimal gland Adenocarcinoma non otherwise specified (NOS). Adenocarcinoma NOS is used to distinguish non specific carcinomas, because of the undistinguished histo morphological features characterize for the other, previously mentioned, more specific carcinoma [9]. According to recent data Adenocarcinoma NOS of lacrimal gland is very rare; therefore we have limited clinical trials, treatments, follow ups and prognosis [12]. Only few cases with this diagnosis are represented; one with abduction deficit symptoms [12] and other with left lower eyelid accessory lacrimal gland [4]. According which this diagnosis questioned the accessory lacrimal gland neoplasm classification [4]. Our patient underwent orbital exenterating under general anesthetize and was sent to oncology department for further treatment with radiotherapy and chemotherapy.
It is known that the lacrimal glands can develop aggressive tumors like adenoid cystic carcinoma, carcinoma-ex-pleomorphic adenoma, mucoepidermoid carcinoma, primary Adenocarcinoma or non otherwise specified. Although the clinical behavior, prognosis, and treatment of these tumors are still poorly defined, the glandular lacrimal is Adenocarcinoma NOS is extremely rare. The diagnosis of the Adenocarcinoma none otherwise specified NOS is made because of the absence of unifying morphologic, immuno phenotypic, and molecular genetics findings. In one side because the absence of the clinical case and prognosis data we assume that early recognition of this highly aggressive tumor may help to delineate its better management and good prognostic outcome. On the other side this case represents the importance progression of the advanced immuno histo chemical or others methods diagnostic approaches towards this group of disease. Finally, this case also illustrates lacrimal gland tumor classification challenges.


