Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rabii Laababsi*, Mohamed Amine Allouane, Anass Bouzbouz, Sami Rouadi, Reda Abada, Mohamed Roubal and Mohamed Mahtar
Received: June 18, 2018; Published: July 03, 2018
*Corresponding author: Rabii Laababsi, Department of ENT, 20 Août hospital, Ibn Rochd University Hospital, Casablanca, Morocco
DOI: 10.26717/BJSTR.2018.06.001324
Non-Hodgkin’s lymphoma with orbital location is a relatively rare tumor with a difficult diagnosis. We report the case of a 54-year-old patient with bilateral exophthalmos. Orbital biopsy allowed the diagnosis of diffuse type B lymphoma. The diagnosis is pathological and immunohistochemical. The treatment consisted of a poly-chemotherapy with a multidisciplinary management.
Keywords: Lymphoma; Non-Hodgkin; Orbit; Exophthalmos; Chemotherapy
Non-Hodgkin’s lymphoma with orbital location is a relatively rare tumor and difficult diagnosis, orbital location accounts for 5 to 10% of orbital expansive processes [1] .The confirmation of the diagnosis is made by histology and immun histochemistry, the treatment consists of poly chemotherapy with multidisciplinary care.
It is a 54-year-old patient, with no particular pathological history, who presented a left exophthalmia and then progressive right in six months, with preservation of the general condition. The clinical examination found a visual acuity at 7/10 on the right and 5/10 on the left, a photo-motor reflex preserved. The biological assessment showed a blood count, normal renal, hepatic functions and negative HIV serology.
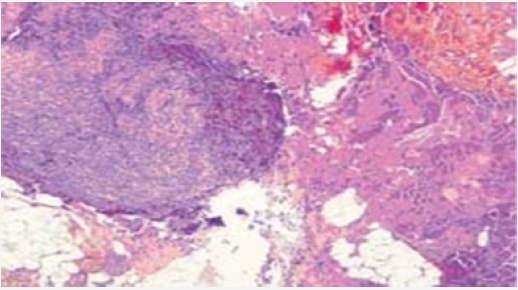
Magnetic resonance imaging (MRI) revealed the presence of intra-orbital processes, retro septal intra and extra-conical, responsible for an exophthalmitis grade 1 right and grade 2 left (Figure 1). A biopsy was made at the block, under general anesthesia and endoscopically, the histopathological examination of the biopsy showed a diffuse proliferation of lymphomatosis cells of medium size, presenting a mature chromatin nucleus and cleaved contour. Immunohistochemistry confirmed the diagnosis of diffuse B-cell lymphoma with negativity of ck and chromogranin and CD3 and CD20 (Figure 2). To date, the patient has received three courses of a polychemotherapy type rituximab-CHOP (ciclophosphamideadriablastinevincristine- prednisolone). The follow-up is only five months but the evolution has been towards a stabilization of the attack.
Figure 2: Infiltration of the orbital muscle and adipose tissue by lymphomatous tumor proliferation.
Non-Hodgkin’s lymphoma with orbital location accounts for 5 to 10% of orbital expansive processes [1-3]. According to Ducrey [4], they constitute 4% of non-traumatic orbital conditions. The orbital localization is rare, objectified at 2% of all Lymphomas [5]. T-cell and B-cell lymphomas are the most frequent at the orbital level. The incidence of ocular lymphoma in ocular appendages in the United States is estimated at about 43,000 new cases per year, with a higher incidence in white populations than in black populations [6- 7]. The increase in HIV cases alone does not explain the increase in the incidence of non-Hodgkin’s lymphoma. Multiple environmental factors appear to be incriminated and are under study.
Patients’ blood spots were collected with a standard procedure: first a peripheral venous blood sample was taken, and then a drop of blood was collected falling on dedicated area of filter paper. To obtain dried blood spots, papers were kept first at ambient temperature for 24 hours. Samples were stored double-bagged with desiccant at-20 °C and analyzed within 1 week of storage. LAL-A on DBS was determined by using 4-methylumbelliferyl palmitate as substrate [7]. As other lipases may interfere with LAL-A measurement, a specific LAL inhibitor known as Lalistat 2 was used. Total lipase activity was determined in absence and then in presence of the inhibitor: the difference between these results corresponds with LAL-A. The range of LAL-A was considered normal between 0, 73 and 3, 03 nmol/spot/h [7,8]. According to Hamilton findings, LAL activity in homozygotes patients with LAL-deficiency was <0.03 nmol/spot/h and in heterozygotes in the range 0.15– 0.40 nmol/spot/h. 7 In cases of LAL-A less than the lower limit of normal of 0.73 nomol/spot/h, a second confirmation was obtained before proceeding to genetic analysis. DBS tests were performed in Bambino Gesù Hospital in Rome. Physicians analyzing LAL activity were unaware of clinical and biochemical characteristics of any enrolled patient.
The average age of onset is 65.8 with a female predominance. The disease is progressive and indolent with an average duration of the symptomatology depending on the site and tumor volume. The most common clinical sign is a periocular mass that can lead to exophthalmia or diplopia. The imaging highlights two evocative aspects, a well-defined mass with fuzzy contours that can mold on the eyeball, optic nerve or bone wall, or an infiltrating form extending into the eyelid, the subcutaneous planes or intra and extra-conical adipose tissue and more or less including muscle and optic nerve [2].
CT shows a density close to that of muscles with moderate enhancement after contrast injection.
The MRI shows:
i. T1 sequence: signal close to that of the muscles.
ii. T2 sequence: moderately hypo or hyper intense, the enhancement is net after injection of PDC.
Bone damage is rare, the extension assessment must be complete and carried out in a specialized department. It conditions the care that must be Multidisciplinary. The diagnostic examination of certainty remains the biopsy, it allows an anatomo pathological examination more or less accompanied by an immunohistochemical study, even genetic. In isolated low-grade lymphomas, the appropriate course of action is clinical and paraclinical surveillance; for symptomatic or high-grade forms, chemotherapy combined with localized radiotherapy will be the gold standard first-line treatment. New therapeutics appear to be effective in lower grade lymphomas to note the anti CD20 antibody. The prognosis depends mainly on the histological form, disease-free survival rates and overall survival at 5 years are 64% and 79% for low-grade lymphoma and 43% and 50% for high-grade lymphomas. .
Orbital lymphoma is a rare disorder, often of indolent evolution the diagnosis can only be asserted by the pathological +/- immunohistochemical study. The MRI and if not the orbital CT allow to give a precise assessment of extension which conditions the management, the main differential diagnosis is the pseudoinflammatory tumor.


