Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Enver Mirza*1, Feyza Calis Karanfil2 and Gunsu Deniz Mirza3
Received: October 22, 2018; Published: November 02, 2018
*Corresponding author: Enver Mirza, Department of Ophthalmology, Turkey
DOI: 10.26717/BJSTR.2018.10.001995
Pseudoxanthoma elasticum (PXE) is a rare, multisystemic, genetic disorder and it is characterized by mineralization and fragmentation of elastic fibers. PXE is associated with many complications in various organs especially the skin, eyes, and vascular system. Angioid streaks (AS) are the frequent ocular findings in PXE. AS with PXE is also known as Gronblad-Strandberg syndrome. In fact, the most important complication of PXE in ophthalmology is the development of choroidal neovascularization. CNV is the main reason for visual impairment. In this case report, it was aimed to share the ocular manifestations in a patient with PXE.
Abbreviations: PXE: Pseudoxanthoma Elasticum; AS: Angioid Streaks; CNV: Choroidal Neovascularization; OCT: Optical Coherence Tomography
Pseudoxanthoma elasticum (PXE) is a rare genetic, multisystemic disease which affects primarily the skin, the eyes, and the vascular system. The prevalence of PXE is approximately 1:50000-200000 [1]. PXE is characterized by progressive calcification and degeneration in elastic fibrils [2]. It is known that the cause of PXE is associated with the mutation in the gene encoding the ABCC6 (MRP6) transmembrane transport protein [3]. Ocular abnormalities or complications which are angioid streaks (AS), peau d'orange appearance, comet lesions, and choroidal neovascularization (CNV) develop in vast majority of patients with PXE [4]. In PXE, the earliest fundus finding is peau d'orange appearance and the most common ocular manifestation is as [5]. CNV occur less than AS but CNV may lead to serious visual impairment [6]. In this paper, we report the case of a 45-year- old PXE patient whose visual acuity was decreased due to CNV secondary to AS.
Figure 1: Fundus photography of the patient revealed peau d’orange appearance and peripapillary angioid streaks in both eyes.
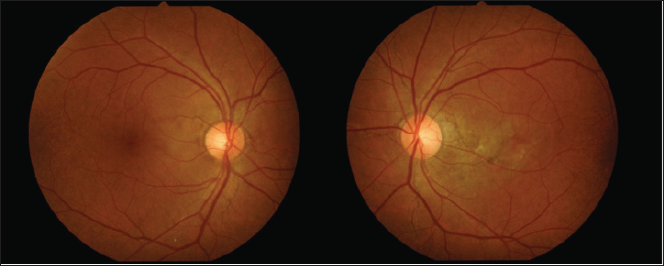
A 45-year-old man with no history of any systemic diseases presented to our clinic complaining of visual impairment in his left eye for approximately a year. He had previously applied to some other clinics but could not be diagnosed correctly. Best corrected visual acuity was 20/20 OD and 16/20 OS. The anterior segment of both eyes showed no abnormalities and intraocular pressure was 16 mmHg in both eyes. Dilated funduscopic examination revealed peau d'orange appearance in the temporal parts of the retina and AS extending radially from the optic disc in both eyes (Figure 1). AS were more distinct in the left eye and extended to near the fovea. Optical coherence tomography (OCT) revealed CNV and intraretinal fluid in the left eye (Figure 2). Asymptomatic, cutaneous signs such as small (1-5 millimeters), yellowish or skin-colored papules were also observed in his back of the neck (Figure 3). When his medical history questioned again it was learned that he had gastrointestinal bleeding before. Therefore, the patient was consulted with the department of dermatology, internal medicine and cardiology. Indeed, biopsy of skin lesions confirmed PXE and intravitreal anti- VEGF injections were performed to the patient s left eye for the CNV secondary to AS.
Figure 2: Choroidal neovascularization and intraretinal fluid observed in the left eye of the patient by optical coherence tomography.

Figure 3: Cutaneous manifestations of PXE. Small yellowish papules coalescing into larger plaques in the back of the patient's neck.

Generally, the first signs of PXE are the asymptomatic cutaneous features and AS are the most frequent ocular findings of PXE [3]. AS are gray-white lines with rupture of the thickened elastic fibers of Bruch's membrane extending radially from the optic disc [1]. AS occur in 80% of patients with PXE [7]. However, AS are not the pathognomonic sign of PXE and may occur due to Paget's disease, Marfan syndrome, Ehler-Danlos syndrom, sickle-cell anemia, and beta thalassemia [8-10]. AS most often present in both eyes and do not exist at birth. They usually develop at third or fourth decades of life. AS mostly do not threat visual acuity if they are not extending to the fovea. The development of CNV near to fovea is the major cause of visual impairment. CNV occurs in approximately 42-84% of patients with PXE [6]. The knowledge of pathogenesis and the nature of this complication remains limited but probably, CNV may occur due to fibrovascular scar after subretinal hemorrhages [11,12]. Besides ocular complications, some serious and life- threatening complications associated with PXE has been reported previously [4]. These are heart failure, sudden cardiac death, gastrointestinal and intracerebral hemorrhages [1].
Indeed, our patient had gastrointestinal bleeding previously but no serious problems were reported. To date, there is no effective treatment for PXE or specific therapies for the systemic complications of this disease. Nevertheless, intravitreal anti-VEGF injections have been performed to increase visual acuity in PXE complicated with CNV [12]. In conclusion, PXE is a multisystemic disorder and eye is one of the affected organs. CNV is the most serious complication which may reduce visual acuity but it should be kept in mind that other systemic complications may be fatal.


