Abstract
Introduction: Mid Urine Iodine Concentration (MUIC) is one of the biomarkers that are typically used to measure the concentration of iodide found in plasma thyroxin in human being and used to predict the risk of Iodine nutrient deficiency at population level. This study aimed to assess MUIC and associated factors among children age 6 to 59 months in the Central highland area of Ethiopia after an over a decade of intervention of with iodized salt by Ethiopian Government.
Methods: Community-based cross-sectional study was applied with multistage sampling method to select individual household (HH) and correspondent mothers/ caregivers with their pair children age 6 to 59 months according to the proportion of population found in each Keble (small administrative unit). Collected samples of mid urine specimens taken from selected children were transferred to and stored in laboratory with great percussion. MUIC were analyzed with ammonium persulfate methods in Ethiopian Public Health Institute laboratory. Data were entered into EpiData3.0 and transferred to SPSS for window as version 21 for cleaning and analyses, t multivariable logistic regressions model was fitted to isolate independent proctitis of inadequate MUIC.
Results: The median MUIC was 107+ 5 μg/L and mean iodide found in mid urine was 108 + 9 μg/L (n = 812). The status of adequate iodine nutrient (MUIC >100) among children was 88.2 % (n=716) and those 11.8 % (n=96) of children who had MUIC 50 to 99 μg/L were mild deficient in iodine nutrition. Being female (adjusted odds ratio [AOR] = 8.3, 95% CI95%CI:4.44, 15.43) and stunted growth (AOR=2.35, 95%CI:1.44,3.84) were considered as independent predictors the likelihood of for insufficient iodine nutrient among children of female and stunted group compared to male children and children who had normal growth. However, early initiation of complementary food (AOR=0.18, 95%CIL0.05, 0.65) and conclusive communication on iodized salt intake (AOR=0.64, 95%CI: 0.39, 1.11) had positive effect on adequacy of iodine nutrient among children. In linear logistic regression analysis, being increasing height (B coefficient [B] = 0.43, CI=0.04, 0.92) and early time to incite complementary food (B=0.13, CI=0.19, 0.27) were potentially increase adequacy of iodine nutrient in children by 0.43 μg and 0.04 μg respectively.
Conclusion: A high proportion (88.2%) of children had adequate iodine nutrient showing that the intervention program has an effect in improving iodine status of children. This finding should be substantiated by future studies that measure more sensitive biomarkers such as T3 and T4.
Abbreviations: MUIC: Mid Urine Iodine Concentration; HH: Household; AOR: Adjusted Odds Ratio; WHO: World Health organization; UI: Urinary Iodine; IDD: Iodine Deficiency Disorders; WHZ: Weight for Height Z score; HAZ: Height for Age Z Score; Hb: Hemoglobin; CDHS: Cambodian Demographic Health Survey
Introduction
Iodine is a crucial nutrient during the fetal time and childhood, especially during the first five years. as these a group is more vulnerable group to inadequate iodine intake [1]. Globally, Iodine deficiency affects 1.8 billion with brain damage in newborns, reduced mental capacity, and goiter and in Africa alone; 260 million populations are under insufficient of iodine intake [2]. Iodine deficiencies potentially cause mental impairment and physical damage on children [3]. Iodine deficiency occurs in preschool children when iodine intake falls below the recommended levels /90μg [4]. Improving progress towards the sustainable elimination of IDD in Latin America and the Caribbean, East Asia and the Pacific regions showed that greater of 80% of the households have been consuming adequately iodized salt since 1990 [1]. World Health organization (WHO) recommended that the deficiency of iodine corrected by increasing iodine intake through fortified table salt that required four major components of implementing the strategies. Among these strategies are correction of iodine deficiency, surveillance including monitoring and evaluation, educate the public and inter-sectorial collaboration and advocacy and communication to mobilize public health authorities are frontline for the Control of IDD through the world [5].
According to WHO recommendation, urinary iodine (UI) as potential indicator with high acceptance for the assessment and monitoring for subclinical iodine deficiency [6]. However, median urinary iodine concentrations of 100-199 mg/l in samples from schoolchildren or adults indicate adequate iodine intake and optimal iodine nutrition [7]. Urinary iodine excretion reflects the average daily iodine requirement intake and is an important index for determining the concentration of iodide found in plasma thyroxin [6]. In Ethiopia, insufficient iodine intake remained pervasively high until 2011 when the country was recognized as the top burden of iodine-deficient in the world [1]. Ethiopia had developed strategies are currently insufficient to monitor and evaluate the national programs related to measuring progress towards the goal of eliminating iodine deficiency [3]. In the Ethiopia monitoring and evaluation of iodine deficiency is not done regularly. But a single finding showed that 99.17% of households (HHs) had met their requirement of iodine per person per day in central highland region in Ethiopia [8]. Concerning to knowledge and attitude of the HHs toward prevention of IDD and HH iodised salt utilization is required necessary to educate the public. Following the current report, this study intended to measure MUIC to determine the effect of iodised salt intervention since over a decade. The study intended to assess iodine status of children as a marker for the impact of intervention with iodized in eliminating IDD salt [8].
Methods and Materials
Study Design and Area
Community based cross sectional study was used to determine iodine deficiency using MUIC through ammonium persulfate analysis methods following evolution iodised salt intervention in Central highland region of Ethiopia in October to December 2018. The study area included Arsi and Bale provinces (Munesa, Asella, Limuna Bilalo, Digeluna Tijo, Honkolo Wabe) mountains areas and has an altitude of above 2400 meters and had history of annual mean rainfall of 2200 mm to 2350mm [9]. All children aged 6-59 months with their mothers from households registered were selected using systematic sampling to participate in the past survey of Knowledge and Attitude about Prevention of Iodine Deficiency Disorders (IDD) among Women in the study area in June 2018. Children aged 6-59 months from those women who were registered and participated in the previously survey of January to June 2018 were included in study.
Sample Size Estimation
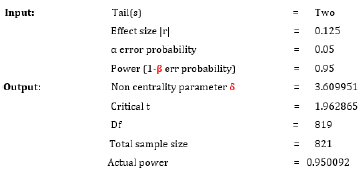
Sample size was determined using G power computer software version 3.0 with the following assumptions:
Analysis: t tests - Correlation: Point bi-serial model
Sampling Procedure
Multistage sampling method was used to select study subjects. Clustered sampling method was applied in the first stage to select eight distracts administration at the side of to Arsi Bale plateau and the neighboring of Chilalo Mountain; subsequently 12 kebeles (small administrative units) and towns (3 rural and Asella) were randomly selected from districts. Finally, systematic sampling method was used to select the individual household and correspondent mothers/caregivers with their pair children age 6 to 59 months according to the proportion of population found in each Keble. Mothers/ caregivers were oriented about the need of requisition urine specimen collection from their children before distributing specimen collection clean cups. To keep the need mid urine specimen, procedural demonstration was shown for mothers/ caregivers as to collect the specimen. It was possible to collect mid urine specimen from 800 children and each specimen was transferred to ladled clean tubes. These samples were transported with cold-boxes to Ethiopian Public Health Institute and put into refrigerators. Following these, adequate information was given for laboratory professionals to prevent contamination and keeping the specimen tubes as tightened closed to protect evaporation in laboratory. Other important cares were taken for specimen during transfer and storage in laboratory.
Laboratory Procedure for iodine determination from mid urine
a. In first, for each specimen mixing urine procedure was made to suspend sediment.
b. 250μl Pipetted from each urine sample into a 13 x 100 mm test tube. Pipette was used for each iodine standard into a test tube, and then H2O was added as needed to make a final volume of 250μl. Duplicate iodine standards and a set of internal urine standards were included in each assay.
c. One ml 1.0 M ammonium persulfate was Added to each test tube.
d. All test tubes were heated for 60 minutes at 100oC.
e. Each test tube was cooled to room temperature.
f. Afterwards 2.5 ml arsenious acid solution was added and mixed by inversion or vortex and then the test tube was allowed to stand for 15 minutes.
g. Subsequently, 300μl of ceric ammonium sulfate solution was added to each tube (quickly mixed) at 15-30 second intervals between successive tubes. A stopwatch was used for this practice at 15 seconds interval.
h. Each test tube contained treated specimen was allowed to sit at room temperature. 9. Exactly after 30 minutes, ceric ammonium sulfate was added to the first tube and its absorbance was read at 420 nm.
i. Successive tubes were read at the same interval of adding the ceric ammonium sulfate.
Based on WHO references, the cut-off value for iodine deficiency was signified as MUIC lower than100 μg/L and severity was classified as lesser than 50 μg/L stated as iodine nutrition was insufficient. MUIC level was 50 to 99 μg/L was classified as insufficient and termed as mild iodine deficiency, and level of MUIC within the range of 100 to 199 μg/L traced as adequate iodine nutrition [7]. Child feeding and dietary sources: Individual mother or caregiver was interviewed using structured administered questionnaire to assess her child’s dietary sources, time for introduction of complementary food and the usual option of food types during infantile and childhood period, about her knowledge and attitude relating to HH iodised salt utilization.
Blood test for hemoglobin: Each child’s mother or guardian was informed about need of blood samples. Consequently, each child’s right-hand finger was warmed and relaxed before precise finger prick. Mothers or guardians were asked to comfortably immobilize the finger to be punctured. Blood sample taken from children were determined using Hemocoel Hb 301® and categorized into no Anaemia (hemoglobin [Hb]) >11g/dl)/ normal, anaemic [Hb < 11g/dl] [10]. Anthropometric measurements: weight and height measurements were done according to standards procedures and weight for height Z score (WHZ) and height for age Z score (HAZ) generated using WHO anthrax software [11].
Abbreviations and Symbols
ml: mil-litter;
μl: micro litter;
nm: Nano-meter;
oC: degree Celsius
Data Analyses
Data on MUIC laboratory results and other variables were entered into EpiData3.0 software and transferred to SPSS for windows version 21 for cleaning and analyses. Descriptive statistical methods were used for presenting median urinary iodine excretion with 25th, 75th percentile mean among different variables. Demographic variables and nutritional status of children described and analysed using logistic regression models. AOR with 95% CI were computed to assess the presence and degree of association with the outcome variables. P-value less than 0.05 was used to declare a statistically significant association. Linear regression model was used to assess predictors for positive/ negative or no effect on children’s MUIC and correlation was declared at beta coefficient (B) and 95% CI. All assumptions of linear regression analysis were considered as sign of model fitness.
Results
A total of 812 children participated in the study with a response rate of 98.9 % and 48.8% of study subjects were young children age < 24 months. More than 716 (88.2 %) of the respondents had adequate iodine nutrient (MUIC >100) which was very exciting for organizations and people working for the success of iodised salt intervention. Children who had MUIC 50 to 99 μg/L were 11.8 % (n=96). The mean iodine concentration found in mid urine was 108 + 9 μg/L (n = 812) with the maximum and minimum values of 178 μg/L and 52 μg/L. respectively.
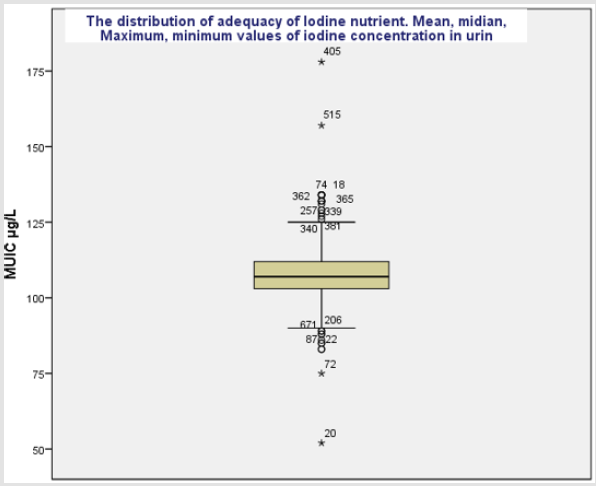
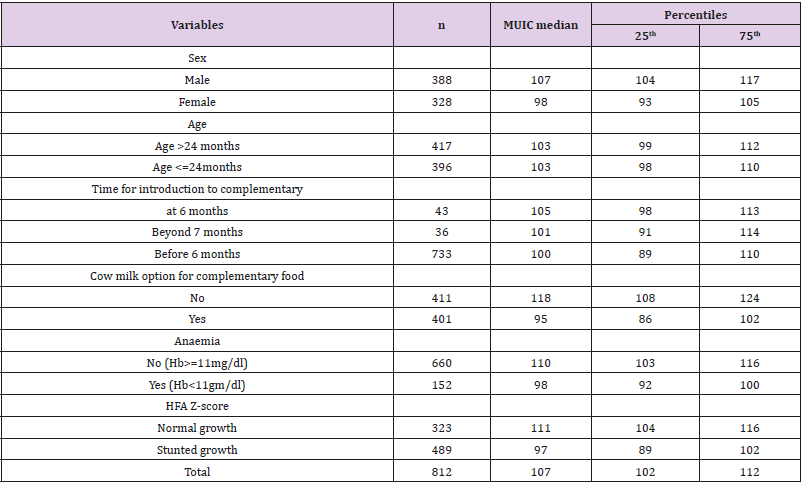
The median MUIC was 107+ 5 μg/L which is found between 100-199 μg/L indicative for the adequate iodine nutrient in study population and majority of the study subjects had urine iodine concentration above 75th percentile (Figure 1). Median UIC among male group was higher (107μg/L) than female (98 μg/L) and anaemic children had lesser UIC median (98μg/L) than children group with non anaemic (110 μg/L), but there was no difference in median UIC among children age group >24 months and <=24months (Table 1). In bivariate logistic regression analysis, sex, age, starting time for complementary food, attitude HH to use adequate iodized salt, practicing of adding iodized salt in HH food cooking and Anaemia were strongly associated with insufficiency of iodine nutrient among study subjects.
Figure 1: Median, 25th, 75th and mean iodine concentration distribution in mid urine among children 6 to 59 months in Central Highland of Ethiopia.
Table 1: Demographic and nutritional variables adjusted for MUIC weights and presented as median with 25th, 75th percentile.
dl, decilitre; Hb, haemoglobin; HFA, Height relevant to age, MUIC, mid urine iodine concentration; mg, milligram; n, total samples; Z score, standard diversion from distribution of HFA or WFH.
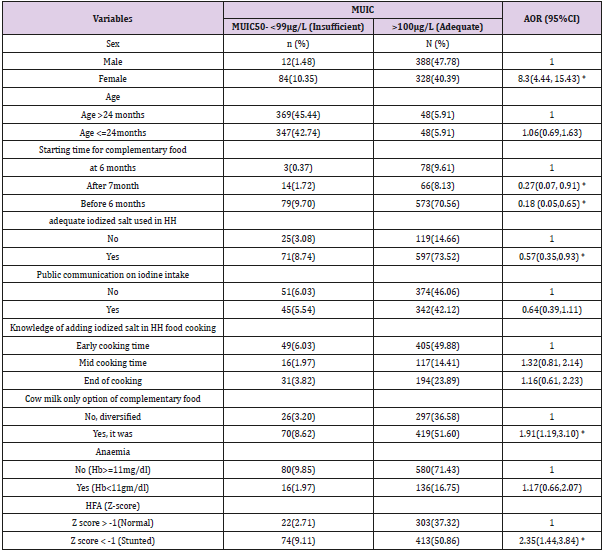
In multivariable logistic regression analysis, being female had more than 8 times likely to exposed for insufficiency iodine nutrient than those who were males (AOR = 8.3, 95%, 95%CI: 4.44, 15.43). Regarding complementary food of children, using cow milk as the only option had 1.9-time risk of iodine deficiency compared to children who used diversified foods (AOR= 1.91, 95%CI:1.19, 3.10). Stunted growth (HFA Z score < -1) in children also had more than 2 times the risk of inadequacy of iodine nutrient compared to those children who had normal growth (AOR=2.35, 95%CI:1.44, 3.84). Being female, stunted growth and using cow milk as the only option for complementary food were statistically significant predictors of risk for insufficient iodine nutrient among children.
The introduction of complementary food for children at early age of 6 months had only 0.18 the risk of developing insufficiency of iodine nutrient compared with nonusers (AOR=0.18, 95%CI: 0.05, 0.65). Adequate iodized salt used in HH was preventing the risk of insufficiency iodine nutrient by 0. 57 compared to those HH who did not use (AOR=0.57, 95%CI:0.35, 0.93) and these variables were had positive effect on adequacy of iodine nutrient among children (Table 2).
Table 2: Multivariable logistic regression models predicting the likelihood of insufficiency of iodine among children age 6 to 59 months in Central highland of Ethiopia, 2018.
MUIC, AOR, CI dl, decilitre; Hb, haemoglobin; HFA, Height relevant to age, MUIC, mid urine iodine concentration; mg, milligram; n, total samples; Z score, standard diversion.
Discussion
This study showed that the proportion of children that had adequate iodine nutrient was higher (88.2 %) than finding in the 2014 Cambodian Demographic Health Survey (CDHS) which was 36.3% [12]. Likewise, in the current finding the prevalence of mild (50 to 99 iodine nutrient insufficiency accounted to 11.8 % which was very lower compared to CDHS reported that 63.7% of children had UIC below 100 μg [12]. This difference could be from the time of 2014 and 2018 for MUIC reassessment. The achievements on the success of iodised salt intervention increasing from time to time even in the feature the current finding can be changed. This finding indicated that median UIC among children age 6 to 59 months was 107 μg/L (102, 1012 μg/L0) consistent with the study conducted among Norwegian children age 18 months reported in 2018, where UIC median was 129 μg/L (81–190 μg/L). But, the proportion of children that had UIC below100 μg/L was higher (34%) compared to the current finding was 11.8% [13]. On the other prediction of adequacy of iodine nutrient, of this study finding higher proportion children (88.2%) found with UIC between 100 and 200 μg/L compared with Norwegian children was 59% [13].
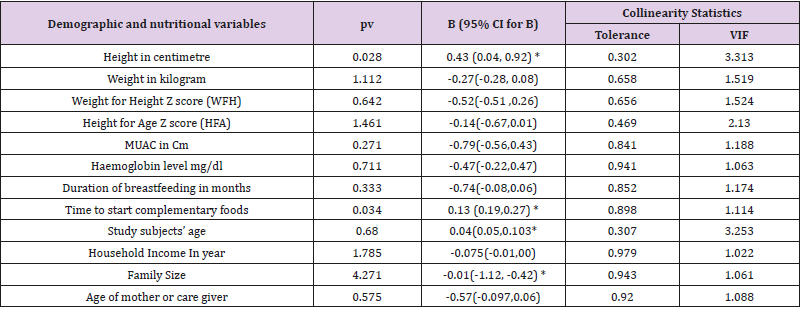
Therefore, estimating the success of long era iodised salt intervention in the population with holding adequate data through wide study area in diversified community and using applicable feasible-preferable method (A ammonium persulfate) in MUIC analysis were validated for accuracy of these findings [7]. In monitoring iodine status, median urinary iodine among young children remains the key defining indicator [14]. However, very few studies were conducted among young children age 6 to 59 months that are potentially risk group for iodine deficiency and indicator for the evaluation of the success for iodine intervention. For instance, monitoring and evaluation has improved over the last decade, but many countries have still not implemented national monitoring systems and lack of literatures may be relay to the cost of MUIC analysis which rise a challenge for researchers working in developing countries. We thought that this finding will have a primary contribution of information on the MUIC among children age 6 to 59 months in Ethiopia which can be used for evaluating the effect of iodized salt intervention in this age group in Ethiopia (Table 3).
Table 3: Linear logistic regression model predicting nutritional and demographic with MUIC in μg/L among children in Central Highland of Ethiopia.
Cm, centimetre, MUAC, Mid upper Arm circumference; Z score, standard division from the normal distribution HFA or WFH; pv, p-value; B, Beta –Coefficients, CI, Confidence Interval; VIF, Variable inflation factor.
Conclusion
This study showed that the iodine status among children age 6 to 59 months was at good status. But few proportions of children had insufficient iodine status. Being female and stunted (short stature) were the major independent variables that predicted iodine insufficiency among these children. Future research should use for sensitive biomarkers including T3 and T$ to substantiate this finding.
Acknowledgement
We would like to express their gratitude to Jimma University for financial support and ethical approval. We extend our special gratitude to Central highland provinces (Arsi and Bale), Munesa, Asella, Limuna Bilalo, Digeluna Tijo, Honkolo Wabe Health Offices for their administrative, technical and material support. Finally, we thank the study participants and health extension workers for their involvement in the study. Finally, I like to thank Ethiopian PHI Nutrition laboratory workers for their patience and carful MUIC analysis.
Ethical approval
This research was approved by Ethical Review Committee of Jimma University. Letter of permission was obtained from Arsi Zone administrative and health department offices. At the end, we obtained permission from 8 district administrative offices 16 Kebeles (Smallest Administrative Units) which were site for data collection administrations offices. In addition, all of the study participants (children’s mothers/ caregivers) were informed about the purpose of the study.
References
- (2014) Iodine Nutrition in Africa. The International Council for Control of Iodine Deficiency Disorders. SIGHT AND LIFE 27(3).
- (2008) World Health Organization, UNICEF, ICCIDD Assessment of Iodine deficiency disorders and monitoring their elimination.
- Zimmermann MB (2012) The effects of iodine deficiency in pregnancy and infancy. Paediatric and Perinatal Epidemiology 26(Suppl 1): 108- 117.
- (2004) World Health Organization. Iodine status worldwide WHO Global Database on Iodine Defiiency, Department of Nutrition for Health and Development World Health Organization, Geneva, USA.
- (2001) Human Vitamin and Mineral Requirements. Food and Agriculture Organization of the United Nations. World Health Organization: Food and Nutrition Division FAO, Rome.
- (2001) World Health Organization, WHO, UNICEF, ICCIDD Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 2nd edition, Geneva, USA.
- Frrerde A, Abera M, Belachew T (2018) knowledge and attitude about prevention of iodine deficiency disorders (IDD) among women and quantification of iodide found in table talt in Central Highland of Ethiopia. Biomedical Journal of Scientific & Technical Research 12(2).
- Mekasha A, Nigatu L, Tesfaye K, Alan J Duncanc (2013) Modeling the response of tropical highland herbaceous grassland species to climate change: The case of the Arsi Mountains of Ethiopia. Biological Conservation 168: 169-175.
- (2011) World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System, Geneva, USA.
- (1995) World Health Organization Expert Committee on Physical Status. Physical status: the use and interpretation of anthropometry: report of a WHO Expert Committee, Geneva, USA.
- Arnaud Laillou, Prak Sophonneary, Khov Kuong Low, Hong R, Un S, et al. (2016) Urinary Iodine Concentration among Mothers and Children in Cambodia, PMC Journal of Nutrients 8(4): 172.
- Aakre I, Markhus MW, Kjellevold M, Moe V, Smith L, et al. (2018) Sufficient iodine status among Norwegian toddlers 18 months in Norway. Journal of Food & Nutrition Research 62: 1443.
- Maria Andersson, Bahi Takkouche, Ines Egli, Bruno de Benoist (2003) The WHO Global Database on iodine deficiency disorders: the importance of monitoring iodine nutrition. Scandinavian Journal of Nutrition 47(4): 162-166.
- Delange F, Fisher DA, Glinoer D (1989) Iodine nutrition and congenital hypothyroidism. Research in congenital hypothyroidism 161: 173-185.

 Research Article
Research Article