Abstract
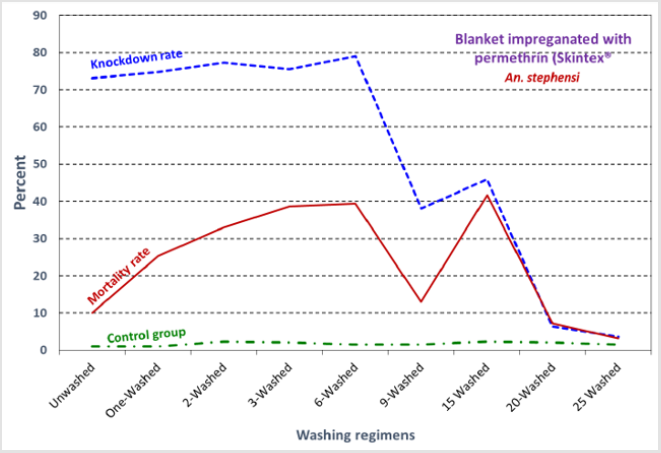
Objective of this study was to evaluate the bioefficacy of Skintex® MR III blanket against main malaria vector, Anopheles stephensi. The effectiveness of blanket was evaluated using conical according to the WHO methods. Washing procedure was followed by WHO method. Results indicated that in Skintex® MR III blanket mortality around 40% in 6 washes and no mortality in control group. After 25 washes the efficacy is reducing. This blanket has more repellency and knockdown effect against malaria vectors. Findings of this study provide guideline for malaria vector control authorities and people using pyrethroid-impregnated blanket especially in the complex emergency conditions.
Keywords: Malaria; Blanket; Skintex; Permethrin; Residue
Introduction
Malaria and other mosquito-borne disease are the major problems worldwide. Currently there are proven and effective tools to fight against malaria including vector control measures [1]. As these tools are scaled up, malaria endemic countries need to continually update the skills and competence of the health workers engaged in malaria control and elimination. Malaria is one of the important infectious diseases in Iran with an average of about 15000 annual cases in the last decade. More than 80% of malaria cases in Iran are reported from three provinces of Sistan and Baluchistan, Hormozgan, and Kerman in southern and southeastern areas of the country. The most routes of malaria cases are immigration from Afghanistan and Pakistan to southern and southeastern areas of the country (Ministry of Health, annual reports). Locally transmitted cases are now concentrated in the south-eastern part of the country, which are affected by extensive population movement across the border with Pakistan, where malaria control faces serious difficulties. In 2009, I.R. Iran set timebound elimination objectives for its malaria program.
There has been excellent progress since, but the continued risk of importation of malaria cases from Pakistan poses a huge challenge, politically, socially, operationally and technically, to malaria elimination in Iran. The situation in the next decade will be absolute elimination or one where a few small shortlived foci emerge from time to time as a result of importation. The latest number of autochthonous cases in the whole country is 42 including 23 local malaria patients, 7 relapsed cases, 12 imported from the other districts by end of July 2016. There are several works on different aspects of malaria including insecticide resistance monitoring [2-12], sibling species, molecular study, new record [13-20], novel methods for vector control [21-26], faunestic study [27,28], use of plants for larval control [29-41] using bednets and long lasting impregnated nets [42-48]morphological studies [49-51], malaria epidemiology [52-55], ecology of malaria vectors [56-64], biodiversity [65,66], community participation [45,54], vector control [67], repellent evaluation [68], anthropophilic index of malaria vectors [65,69], training [70] is designated as malaria training center by WHO. There are several reports on different aspects of malaria vectors recently [71-96]. Insecticide-treated bedding materials such as impregnated blanket with pyrethroids could protect the people against vectors of diseases such as malaria in the complex emergency situation which and are more likely to sleep in exposed situations.
Skintex MR III Blanket
Every yard of our Skintex MR III blankets contains millions of permethrin filled microcapsules that protect against mosquitoes, ticks, ants, flies, chiggers and midges. The proprietary micro encapsulation process creates a slow release effect for the active ingredient, Permethrin, and doesn’t leave any greasy residue or smell associated with some insecticides. The blanket is lightweight and breathable, packs up small, and can be used in many different applications. Many users of the blanket find that it is comfortable to wear even in the humid conditions which attract mosquitos. When you add in the other various pests and insects that experience the knockdead/knockdown effect of Skintex MR III, the blanket quickly becomes an appealing accessory for hikers, campers, cycle tourists, and any family who spends time outdoors.
Materials and Methods:
Mosquitoes
The Beech strain of An. stephensi which is susceptible to insecticides is used. The breeding was carried out at 29±1 ºC and 60±10% relative humidity at 16:8 h light-dark photoperiod. The larvae were fed with enriched wheat germ and the adults received a 10% sucrose solution. Guinea pigs were used for blood-feeding of female mosquitoes. At each replicate of the biological efficacy of the nets, a total of 100 sugar-fed of 5–8 days females were used. The sucrose solution was picked up from the cage, 12 hours before starting the experiments.
Washing Procedure
Samples (25×25 cm) were individually introduced into one-liter beakers containing 0.5-liter deionized water, with 2 g/L soap savon de Marseille “Le Chat®”. The soap was added and fully dissolved just before introduction of net samples. Beakers were immediately placed into a water bath at 30 ºC and were shacked for 10 min at 155 rounds per min. The machine is the same as recommend by WHO. The samples were then removed and rinsed twice for 10 minutes in clean, deionized water in the same shaking conditions. Nets were dried at room temperature and stored at 30 ºC in the dark. A piece of 25×25cm was used for tunnel test prior and after every washing. This is following of WHO standard washing procedure. The net was washed and dried once a week. The netting sample had nine holes with 1 cm diameter and the nets were fixed on a cardboard frame. The nets were replicated as appropriate number.
Conical Bioassay
The samples were subjected to standard WHO bioassays. Mosquitoes were exposed to netting samples for 3 minutes after which they were held for 24 h with access to 10% sugar solution. Four cones gently fitted on the net. A net flap was made inside the cone to reduce the chance of mosquitoes resting on the cone instead of on the treated net. Five female mosquitoes introduced at a time in each cone with appropriate replicates per net sample. In cone bioassays, five mosquitoes were introduced into a cone at a time. 20 other batches of each mosquito were exposed to netting from untreated nets as control. Time interval between each set of a 4 cone was as brief as possible. At least 100 mosquitoes were tested on a netting sample (25×25 cm). Conical tests were carried out according to the WHO method.
Results and Discussion
Figure 1: Trend of knockdown and mortality rates of An. stephensi exposed to blankets impregnated with permethrin (Skintex®) using cone tests.
The present study determined the efficacy of Skintext using cone bioassay. The results are presented in (Figure 1). In the conical test, mortality rate in the control was zero and in the treatment was high indicating efficacy of blanket. Many fields research exhibited that if pyrethroid impregnated bed nets was not exposed to washing, the residual effect of insecticide will be remained up to 6 to 12 months. There are several reports on the efficacy of nets [97-108]. This residual effect depends on type and quantities of insecticide used as well as type and characteristics of net. In practice, washing methods, type of detergents, the numbers and method of washing, are not as the same as in different parts of the world. It is determined that remaining soap on nets will demolish the molecular structure of pyrethroids. Results of this study are useful for decision making for malaria and other vector control. According to the producer, the SkintexTM MR III blanket is a lightweight, durable synthetic blanket treated with microencapsulated permethrin. The blanket is intended to provide personal protection from mosquito bites and malaria infection in situations where use of an insecticide-treated net or indoor residual spraying is not feasible.
Blanket use disrupts permethrin microcapsules, releasing the insecticide, which repels and kills mosquitoes landing on the blanket. The blanket provides a physical barrier against mosquito bites. Permethrin in the blanket deters mosquito landing and probing, and kills mosquitoes following exposure (100% knockdown, 100% mortality). The encapsulation of the permethrin provides extended persistence of the permethrin as the capsules are gradually opened by movement and friction during blanket use. By reducing mosquito bites, the prototype provides personal infection in situations where use of insecticide treated nets or indoor residual spraying are not feasible. Preliminary results on entomological efficacy, including knockdown and mortality testing, and limited repellency testing WHO tube assays showed 100% knockdown in one hour and 100% mortality of Ae. aegypti after 5 minutes exposure to washed samples (up to 25 washes) [109,110]. Repellency testing indicated a reduction in bites from Ae. aegypti, but did not demonstrate repellency due to the absence of a control and sufficient replication. After 25 washes the concentration of permethrin was 64% of the original concentration (1.4 g/m2). This concentration provided 100% knockdown at 60 min post-exposure and 100% mortality at 24 hrs. Studies by Graham et al. [110] supporting acceptability of pyrethroid-treated sheets and clothing to users and protection from bites. Previous published studies from Afghanistan and Kenya show the proof of principle of treated topsheets or blankets [111,112].
Acknowledgment
This project is financially supported by the Ministry of Health and Medical Education of Iran as NINAD code number: 943646.
References
- (2015) World Health Organization World Malaria Report: 2012. Geneva: WHO 2012. Fecha de consulta 23: 247.
- Vatandoost H, Shahi H, Abai MR, Hanafi Bojd AA, Oshaghi MA, et al. (2004) Larval habitats of main malaria vectors in Hormozgan province and their susceptibility to different larvicides. The Southeast Asian journal of tropical medicine and public health 35(2): 22-25.
- Vatandoost H, Mashayekhi M, Abaie MR, Aflatoonian MR, Hanafi Bojd AA, et al. (2005) Monitoring of insecticides resistance in main malaria vectors in a malarious area of Kahnooj district, Kerman province, southeastern Iran. J Vector Borne Dis 42(3): 100-108.
- Davari B, Vatandoost H, Ladonni H, Shaeghi M, Oshaghi M, et al. (2006) Comparative Efficacy of Different Imagicides Against Different Strains of Anopheles stephensi in the Malarious Areas of Iran, 2004-2005. Pakistan Journal of Biological Sciences 9(5): 885-892.
- Hanafi Bojd AA, Vatandoost H, Jafari R (2006) Susceptibility status of Anopheles dthali and An. fluviatilis to commonly used larvicides in an endemic focus of malaria, southern Iran. J Vector Borne Dis 43(1): 34-38.
- Davari B, Vatandoost H, Oshaghi M, Ladonni H, Enayati A, et al. (2007) Selection of Anopheles stephensi with DDT and dieldrin and cross-resistance spectrum to pyrethroids and fipronil. Pesticide biochemistry and physiology 89(2): 97-103.
- Abai MR, Mehravaran A, Vatandoost H, Oshaghi MA, Javadian E, et al. (2008) Comparative performance of imagicides on Anopheles stephensi, main malaria vector in a malarious area, southern Iran. J Vector Borne Dis 45(4): 307-312.
- Hasasan V, Hossein ZA (2010) Responsiveness of Anopheles maculipennis to different imagicides during resurgent malaria. Asian Pacific journal of tropical medicine 3(5): 360-363.
- Vatandoost H, Hanafi Bojd AA (2012) Indication of pyrethroid resistance in the main malaria vector, Anopheles stephensi from Iran. Asian Pacific journal of tropical medicine 5(9): 722-726.
- Soltani A, Vatandoost H, Oshaghi MA, Enayati AA, Raeisi A, et al. (2013) Baseline Susceptibility of Different Geographical Strains of Anopheles stephensi (Diptera: Culicidae) to Temephos in Malarious Areas of Irana. Journal of arthropod-borne diseases 7(1): 56-65.
- Lak SS, Vatandoost H, Entezarmahdi M, Ashraf H, Abai M, et al. (2002) Monitoring of insecticide resistance in Anopheles sacharovi (Favre, 1903) in borderline of Iran, Armenia, Naxcivan and Turkey, 2001. Iranian Journal of Public Health 31(3-4): 96-99.
- Enayati AA, Vatandoost H, Ladonni H, Townson H, Hemingway J, et al. (2003) Molecular evidence for a kdr-like pyrethroid resistance mechanism in the malaria vector mosquito Anopheles stephensi. Medical and veterinary entomology 17(2): 138-144.
- Naddaf SR, Oshaghi MA, Vatandoost H, Assmar M (2003) Molecular characterization of Anopheles fluviatilis species complex in the Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 9(3): 257-265.
- Oshaghi MA, Sedaghat MM, Vatandoost H (2003) Molecular characterization of the Anopheles maculipennis complex in the Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 9(4): 659-666.
- Sedaghat MM, Linton YM, Oshaghi MA, Vatandoost H, Harbach RE, et al. (2003) The Anopheles maculipennis complex (Diptera: Culicidae) in Iran: molecular characterization and recognition of a new species. Bulletin of entomological research 93(6): 527-535.
- Azari Hamidian S, Abai MR, Ladonni H, Vatandoost H, Akbarzadeh K, et al. (2006) Anopheles peditaeniatus (Leicester) new to the Iranian mosquito fauna with notes on Anopheles hyrcanus group in Iran. J Am Mosq Control Assoc 22(1): 144-146.
- Oshaghi MA, Shemshad K, Yaghobi Ershadi MR, Pedram M, Vatandoost H, et al. (2007) Genetic structure of the malaria vector Anopheles superpictus in Iran using mitochondrial cytochrome oxidase (COI and COII) and morphologic markers: a new species complex? Acta tropica 101(3): 241-248.
- Mehravaran A, Oshaghi MA, Vatandoost H, Abai MR, Ebrahimzadeh A, et al. (2011) First report on Anopheles fluviatilis U in southeastern Iran. Acta tropica 117(2): 76-81.
- Naddaf SR, Oshaghi MA, Vatandoost H (2012) Confirmation of Two Sibling Species among Anopheles fluviatilis Mosquitoes in South and Southeastern Iran by Analysis of Cytochrome Oxidase I Gene. Journal of arthropod-borne diseases 6(2): 144-150.
- Dezfouli SR, Oshaghi MA, Vatandoost H, Assmar M (2003) rDNA-ITS2 based species-diagnostic polymerase chain reaction assay for identification of sibling species of Anopheles fluviatilis in Iran. The Southeast Asian journal of tropical medicine and public health 34(2): 56-60.
- Soltani A, Vatandoost H, Jabbari H, Mesdaghinia A, Mahvi A, et al. (2008) Use of expanded polystyrene (EPS) and shredded waste polystyrene (SWAP) beads for control of mosquitoes. Journal of arthropod-borne diseases 2(2): 12-20.
- Omrani SM, Vatandoost H, Oshaghi MA, Shokri F, Guerin PM, et al. (2010) Fabrication of an olfactometer for mosquito behavioural studies. J Vector Borne Dis 47(1): 17-25.
- Omrani SM, Vatandoost H, Oshaghi M, Shokri F, Yaghoobi Ershadi M, et al. (2010) Differential Responses of Anopheles stephensi (Diptera: Culicidae) to Skin Emanations of a Man, a Cow, and a Guinea Pig in the Olfactometer. Iranian journal of arthropod-borne diseases 4(1): 1-16.
- Omrani SM, Vatandoost H, Oshaghi MA, Rahimi A (2012) Upwind responses of Anopheles stephensi to carbon dioxide and L-lactic acid: an olfactometer study. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 18(11): 1134-1142.
- Chavshin AR, Oshaghi MA, Vatandoost H, Pourmand MR, Raeisi A, et al. (2012) Identification of bacterial microflora in the midgut of the larvae and adult of wild caught Anopheles stephensi: a step toward finding suitable paratransgenesis candidates. Acta tropica 121(2): 129-134.
- Soltani A, Vatandoost H, Jabbari H, Mesdaghinia AR, Mahvi AH, et al. (2012) Field efficacy of expanded polystyrene and shredded waste polystyrene beads for mosquito control in artificial pools and field trials, Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 18(10): 1042-1048.
- Moosa Kazemi S, Vatandoost H, Nikookar H, Fathian M (2009) Culicinae (Diptera: culicidae) mosquitoes in chabahar county, sistan and baluchistan province, southeastern iran. Iranian journal of arthropod-borne diseases 3(1): 29-35.
- Oshaghi MA, Vatandoost H, Gorouhi A, Abai MR, Madjidpour A, et al. (2011) Anopheline species composition in borderline of Iran-Azerbaijan. Acta tropica 119(1): 44-49.
- Hadjiakhoondi A, Aghel N, Zamanizadeh Nadgar N, Vatandoost H (2000) Chemical and biological study of mentha spicatal essential oil from Iran. DARU Journal of Pharmaceutical Sciences 8(1-2): 19-21.
- Hadjiakhoondi A, Vatandoost H, Jamshidi A, Amiri EB (2003) Chemical Constituents of Efficacy of Cymbopogon Olivieri (Boiss) Bar Essential Oil Against Malaria Vector, Anopheles Stepensi. DARU Journal of Pharmaceutical Sciences 11(3): 125-128.
- Oshaghi M, Ghalandari R, Vatandoost H, Shayeghi M, Kamali Nejad M, et al. (2003) Repellent effect of extracts and essential oils of Citrus limon (Rutaceae) and Melissa officinalis (Labiatae) against main malaria vector, Anopheles stephensi (Diptera: Culicidae). Iranian Journal of Public Health 32(4): 47-52.
- Vatandoost H, Vaziri VM (2004) Larvicidal activity of a neem tree extract (Neemarin) against mosquito larvae in the Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 10(4-5): 573-581.
- Hadjiakhoondi A, Vatandoost H, Khanavi M, Abaee MR, Karami M, et al. (2005) Biochemical investigation of different extracts and larvicidal activity of Tagetes minuta L. on Anopheles stephensi larvae. Iranian Journal of Pharmaceutical Sciences 1(2): 81-84.
- Hadjiakhoondi A, Vatandoost H, Khanavi M, Sadeghipour Roodsari HR, Vosoughi M, et al. (2006) Fatty acid composition and toxicity of Melia azedarach L. fruits against malaria vector Anopheles stephensi. Iranian Journal of Pharmaceutical Sciences 2(2): 97-102.
- Sadat Ebrahimi S, Hadjiakhoondi A, Rezazadeh S, Fereidunian N, Vatandoost H, et al. (2005) The components of Tagetes minuta L. and its biological activities against malaria vector, Anopheles stephensi in Iran. Journal of Medicinal Plants 4(16): 43-47.
- Shahi M, Hanafi Bojd AA, Iranshahi M, Vatandoost H, Hanafi Bojd MY, et al. (2010) Larvicidal efficacy of latex and extract of Calotropis procera (Gentianales: Asclepiadaceae) against Culex quinquefasciatus and Anopheles stephensi (Diptera: Culicidae). J Vector Borne Dis 47(3): 185-188.
- Khanavi M, Toulabi PB, Abai MR, Sadati N, Hadjiakhoondi F, et al. (2011) Larvicidal activity of marine algae, Sargassum swartzii and Chondria dasyphylla, against malaria vector Anopheles stephensi. J Vector Borne Dis 48(4): 241-244.
- Sedaghat M, Dehkordi AS, Abai M, Khanavi M, Mohtarami F, et al. (2011) Larvicidal Activity of Essential Oils of Apiaceae Plants against Malaria Vector, Anopheles stephensi. Iranian journal of arthropod-borne diseases 5(2): 51-59.
- Sedaghat MM, Dehkordi AS, Khanavi M, Abai MR, Mohtarami F, et al. (2011) Chemical composition and larvicidal activity of essential oil of Cupressus arizonica E.L. Greene against malaria vector Anopheles stephensi Liston (Diptera: Culicidae). Pharmacognosy research 3(2): 135-139.
- Khanavi M, Vatandoost H, Khosravi Dehaghi N, Sanei Dehkordi A, Sedaghat MM, et al. (2013) Larvicidal activities of some Iranian native plants against the main malaria vector, Anopheles stephensi. Acta medica Iranica 51(3): 141-147.
- Vatandoost H, Sanei Dehkordi A, Sadeghi SM, Davari B, Karimian F, et al. (2012) Identification of chemical constituents and larvicidal activity of Kelussia odoratissima Mozaffarian essential oil against two mosquito vectors Anopheles stephensi and Culex pipiens (Diptera: Culicidae). Experimental parasitology 132(4): 470-474.
- Vatandoost H, Dehakia M, Djavadia E, Abai MR, Duchson S, et al. (2006) Comparative study on the efficacy of lambdacyhalothrin and bifenthrin on torn nets against the malaria vector, Anopheles stephensi as assessed by tunnel test method. J Vector Borne Dis 43(3): 133-135.
- Moosa Kazemi S, Vatandoost H, Raeisi A, Akbarzadeh K (2007) Deltamethrin impregnated bed nets in a malaria control program in Chabahar, Southeast Baluchistan, IR Iran. Journal of arthropod-borne diseases 1(1): 43-51.
- Rafinejad J, Vatandoost H, Nikpoor F, Abai MR, Shaeghi M, et al. (2008) Effect of washing on the bioefficacy of insecticide-treated nets (ITNs) and long-lasting insecticidal nets (LLINs) against main malaria vector Anopheles stephensi by three bioassay methods. J Vector Borne Dis 45(2): 143-150.
- Soleimani Ahmadi M, Vatandoost H, Shaeghi M, Raeisi A, Abedi F, et al. (2012) Effects of educational intervention on long-lasting insecticidal nets use in a malarious area, southeast Iran. Acta medica Iranica 50(4): 279-287.
- Soleimani Ahmadi M, Vatandoost H, Shaeghi M, Raeisi A, Abedi F, et al. (2012) Field evaluation of permethrin long-lasting insecticide treated nets (Olyset((R))) for malaria control in an endemic area, southeast of Iran. Acta tropica 123(3): 146-153.
- Vatandoost H, Mamivandpoor H, Abai MR, Shayeghi M, Rafi F, et al. (2013) Wash Resistance and Bioefficacy of Alpha-cypermethrin Long Lasting Impregnated Nets (LLIN-Interceptor((R))) against Anopheles stephensi using Tunnel Test. Journal of arthropod-borne diseases 7(1): 31-45.
- Vatandoost H, Ramin E, Rassi Y, Abai M (2009) Stability and Wash Resistance of Local Made Mosquito Bednets and Detergents Treated with Pyrethroids against Susceptible Strain of Malaria Vector Anopheles stephensi. Iranian journal of arthropod-borne diseases 3(1): 19-28.
- Emami SN, Vatandoost H, Oshaghi MA, Mohtarami F, Javadian E, et al. (2007) Morphological method for sexing anopheline larvae. J Vector Borne Dis 44(4): 245-249.
- Doosti S, Azari Hamidian S, Vatoost H, Hosseini MOM (2006) Taxonomic differentiation of Anopheles sacharovi and An. maculipennis sl (Diptera: Culicidae) larvae by seta 2 (antepalmate hair). Acta medica Iranica 44(1): 21-27.
- Doosti S, Vatandoost H, Oshaghi M, Hosseini M, Sedaghat M, et al. (2007) Applying morphometric variation of seta 2 (Antepalmate Hair) among the larvae of the members of the Maculipennis Subgroup (Diptera: Culicidae) in Iran. Journal of arthropod-borne diseases 1(1): 28-37.
- Vatandoost H, Ashraf H, Lak SH, Mahdi RE, Abai MR, et al. (2003) Factors involved in the re-emergence of malaria in borderline of Iran, Armenia, Azerbaijan and Turkey. The Southeast Asian journal of tropical medicine and public health 34(2): 6-14.
- Hanafi Bojd A, Vatandoost H, Philip E, Stepanova E, Abdi A, et al. (2010) Malaria situation analysis and stratification in bandar abbas county, southern iran, 2004-2008. Iranian journal of arthropod-borne diseases 4(1): 31-41.
- Hanafi Bojd AA, Vatandoost H, Oshaghi MA, Eshraghian MR, Haghdoost AA, et al. (2011) Knowledge, attitudes and practices regarding malaria control in an endemic area of southern Iran. The Southeast Asian journal of tropical medicine and public health 42(3): 491-501.
- Hemami MR, Sari AA, Raeisi A, Vatandoost H, Majdzadeh R, et al. (2013) Malaria elimination in iran, importance and challenges. International journal of preventive medicine 4(1): 88-94.
- Vatandoost H, Oshaghi MA, Abaie MR, Shahi M, Yaaghoobi F, et al. (2002) Bionomics of Anopheles stephensi Liston in the malarious area of Hormozgan province, southern Iran Acta tropica 97(2): 196-203.
- Vatandoost H, Shahi M, Hanafi Bojd A, Abai M, Oshaghi M, et al. (2007) Ecology of Anopheles dthali Patton in Bandar abbas district, Hormozgan province, southern Iran. Journal of arthropod-borne diseases 1(1): 21-27.
- Hanafi Bojd AA, Azari Hamidian S, Vatandoost H, Charrahy Z (2011) Spatio-temporal distribution of malaria vectors (Diptera: Culicidae) across different climatic zones of Iran. Asian Pacific journal of tropical medicine 4(6): 498-504.
- Hanafi Bojd AA, Vatandoost H, Oshaghi MA, Charrahy Z, Haghdoost AA, et al. (2012) Larval habitats and biodiversity of anopheline mosquitoes (Diptera: Culicidae) in a malarious area of southern Iran. J Vector Borne Dis 49(2): 91-100.
- Hanafi Bojd AA, Vatandoost H, Oshaghi MA, Haghdoost AA, Shahi M, et al. (2012) Entomological and epidemiological attributes for malaria transmission and implementation of vector control in southern Iran. Acta tropica 121(2): 85-92.
- Mehravaran A, Vatandoost H, Oshaghi MA, Abai MR, Edalat H, et al. (2012) Ecology of Anopheles stephensi in a malarious area, southeast of Iran. Acta medica Iranica 50(1): 61-65.
- Soleimani Ahmadi M, Vatandoost H, Hanafi Bojd AA, Zare M, Safari R, et al. (2013) Environmental characteristics of anopheline mosquito larval habitats in a malaria endemic area in Iran. Asian Pacific journal of tropical medicine 6(7): 510-515.
- Soleimani Ahmadi M, Vatandoost H, Shaeghi M, Raeisi A, Abedi F, et al. (2012) Vector ecology and susceptibility in a malaria-endemic focus in southern Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 18(10): 1034-1041.
- Vatandoost H, Emami SN, Oshaghi MA, Abai MR, Raeisi A, et al. (2011) Ecology of malaria vector Anopheles culicifacies in a malarious area of Sistan va Baluchestan province, south-east Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 17(5): 439-445.
- Oshaghi MA, Chavshin AR, Vatandoost H, Yaaghoobi F, Mohtarami F, et al. (2006) Effects of post-ingestion and physical conditions on PCR amplification of host blood meal DNA in mosquitoes. Experimental parasitology 112(4): 232-236.
- Nikookar S, Moosa Kazemi S, Oshaghi M, Yaghoobi Ershadi M, Vatandoost H, et al. (2010) Species composition and diversity of mosquitoes in neka county, mazandaran province, northern iran. Iranian journal of arthropod-borne diseases 4(2): 26-34.
- Vatandoost H, Abai MR, Abbasi M, Shaeghi M, Abtahi M, et al. (2009) Designing of a laboratory model for evaluation of the residual effects of deltamethrin (K-othrine WP 5%) on different surfaces against malaria vector, Anopheles stephensi (diptera: culicidae). J Vector Borne Dis 46(4): 261-267.
- Vatandoost H, Hanafi Bojd AA (2008) Laboratory evaluation of 3 repellents against Anopheles stephensi in the Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 14(2): 260-267.
- Oshaghi MA, Chavshin AR, Vatandoost H (2006) Analysis of mosquito bloodmeals using RFLP markers. Experimental parasitology 114(4): 259-264.
- Vatandoost H, Mesdaghinia AR, Zamani G, Madjdzadeh R, Holakouie K, et al. (2004) Development of the Regional Malaria Training Centre in Bandar-e Abbas, Islamic Republic of Iran. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 10(1-2): 215-224.
- Khoshdel Nezamiha F, Vatandoost H, Azari Hamidian S, Bavani MM, Dabiri F, et al. (2014) Fauna and Larval Habitats of Mosquitoes (Diptera: Culicidae) of West Azerbaijan Province, Northwestern Iran. Journal of arthropod-borne diseases 8(2): 163-173.
- Chavshin AR, Oshaghi MA, Vatandoost H, Hanafi Bojd AA, Raeisi A, et al. (2014) Molecular characterization, biological forms and sporozoite rate of Anopheles stephensi in southern Iran. Asian Pacific journal of tropical biomedicine 4(1): 47-51.
- Chavshin AR, Oshaghi MA, Vatandoost H, Pourmand MR, Raeisi A, et al. (2014) Isolation and identification of culturable bacteria from wild Anopheles culicifacies, a first step in a paratransgenesis approach. Parasites & vectors 7: 419.
- Karimian F, Oshaghi MA, Sedaghat MM, Waterhouse RM, Vatandoost H, et al. (2014) Phylogenetic analysis of the oriental-Palearctic-Afrotropical members of Anopheles (Culicidae: Diptera) based on nuclear rDNA and mitochondrial DNA characteristics. Japanese journal of infectious diseases 67(5):361-367.
- Chavshin AR, Oshaghi MA, Vatandoost H, Yakhchali B, Zarenejad F, et al. (2015) Malpighian tubules are important determinants of Pseudomonas transstadial transmission and longtime persistence in Anopheles stephensi. Parasites & vectors 8:36.
- Khoshdel Nezamiha F, Vatandoost H, Oshaghi MA, Azari Hamidian S, Mianroodi RA, et al. (2016) Molecular Characterization of Mosquitoes (Diptera: Culicidae) in Northwestern Iran by Using rDNA-ITS2. Japanese journal of infectious diseases 69(4): 319-322.
- Shayeghi M, Vatandoost H, Gorouhi A, Sanei Dehkordi AR, Salim Abadi Y, et al. (2014) Biodiversity of aquatic insects of Zayandeh Roud River and its branches, Isfahan Province, Iran. Journal of arthropod-borne diseases 8(2):197.
- Gezelbash Z, Vatandoost H, Abai MR, Raeisi A, Rassi Y, et al. (2014) Laboratory and field evaluation of two formulations of Bacillus thuringiensis M-H-14 against mosquito larvae in the Islamic Republic of Iran, 2012. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit 20(4): 229-235.
- Anjomruz M, Oshaghi MA, Pourfatollah AA, Sedaghat MM, Raeisi A, et al. (2014) Preferential feeding success of laboratory reared Anopheles stephensi mosquitoes according to ABO blood group status. Acta tropica 140: 118-123.
- Anjomruz M, Oshaghi MA, Sedaghat MM, Pourfatollah AA, Raeisi A, et al. (2014) ABO blood groups of residents and the ABO host choice of malaria vectors in southern Iran. Experimental parasitology 136: 63-67.
- Soleimani Ahmadi M, Vatandoost H, Zare M (2014) Characterization of larval habitats for anopheline mosquitoes in a malarious area under elimination program in the southeast of Iran. Asian Pacific journal of tropical biomedicine 4(1): 73-80.
- Soleimani Ahmadi M, Vatandoost H, Zare M, Alizadeh A, Salehi M, et al. (2014) Community knowledge and practices regarding malaria and long-lasting insecticidal nets during malaria elimination programme in an endemic area in Iran. Malaria journal 13: 511.
- Soleimani Ahmadi M, Vatandoost H, Zare M, Turki H, Alizadeh A, et al. (2015) Topographical distribution of anopheline mosquitoes in an area under elimination programme in the south of Iran. Malaria journal 14: 262.
- Soleimani Ahmadi M, Vatandoost H, Zare M, Turki H, Alizadeh A, et al. (2015) Topographical distribution of anopheline mosquitoes in an area under elimination programme in the south of Iran. Malaria journal 14(1): 262.
- Ataie A, Moosa Kazemi SH, Vatandoost H, Yaghoobi Ershadi MR, Bakhshi H, et al. (2015) Assessing the Susceptibility Status of Mosquitoes (Diptera: Culicidae) in a Dirofilariasis Focus, Northwestern Iran. Journal of arthropod-borne diseases 9(1): 7-21.
- Fathian M, Vatandoost H, Moosa Kazemi SH, Raeisi A, Yaghoobi Ershadi MR, et al. (2015) Susceptibility of Culicidae Mosquitoes to Some Insecticides Recommended by WHO in a Malaria Endemic Area of Southeastern Iran. Journal of arthropod-borne diseases 9(1): 22-34.
- Soltani A, Vatandoost H, Oshaghi MA, Ravasan NM, Enayati AA, et al. (2015) Resistance Mechanisms of Anopheles stephensi (Diptera: Culicidae) to Temephos. Journal of arthropod-borne diseases 9(1): 71-83.
- Golfakhrabadi F, Khanavi M, Ostad SN, Saeidnia S, Vatandoost H, et al. (2015) Biological Activities and Composition of Ferulago carduchorum Essential Oil. Journal of arthropod-borne diseases 9(1): 104-115.
- Nikookar SH, Moosa Kazemi SH, Oshaghi MA, Vatandoost H, Yaghoobi Ershadi MR, et al. (2015) Biodiversity of culicid mosquitoes in rural Neka township of Mazandaran province, northern Iran. J Vector Borne Dis 52(1): 63-72.
- Nikookar SH, Moosa Kazemi SH, Yaghoobi Ershadi MR, Vatandoost H, Oshaghi MA, et al. (2015) Fauna and Larval Habitat Characteristics of Mosquitoes in Neka County, Northern Iran. Journal of arthropod-borne diseases 9(2): 253-266.
- Chavshin AR, Dabiri F, Vatandoost H, Bavani MM (2015) Susceptibility of Anopheles maculipennis to different classes of insecticides in West Azarbaijan Province, Northwestern Iran. Asian Pacific journal of tropical biomedicine 5(5): 403-406.
- Shayeghi M, Nejati J, Shirani Bidabadi L, Koosha M, Badakhshan M, et al. (2015) Assessing the Fauna of Aquatic Insects for Possible Use for Malaria Vector Control in Large River, Central Iran. Acta medica Iranica 53(9): 523-532.
- Pirmohammadi M, Shayeghi M, Vatandoost H, Abaei MR, Mohammadi A, et al. (2016) Chemical Composition and Repellent Activity of Achillea vermiculata and Satureja hortensis against Anopheles stephensi. Journal of arthropod-borne diseases 10(2): 201-210.
- Gorouhi MA, Vatandoost H, Oshaghi MA, Raeisi A, Enayati AA, Mirhendi H, et al. (2015) Current susceptibility status of Anopheles stephensi (Diptera: Culicidae) to different imagicides in a malarious area, southeastern Iran. Journal of arthropod-borne diseases.
- Abai MR, Hanafi Bojd AA, Vatandoost H (2015) Laboratory Evaluation of Temephos against Anopheles stephensi and Culex pipiens Larvae in Iran. Journal of arthropod-borne diseases 10(4): 510-518.
- Sanei Dehkordi A, Vatandoost H, Abaei MR, Davari B, Sedaghat MM, et al. (2016) Chemical Composition and Larvicidal Activity of Bunium persicum Essential Oil Against Two Important Mosquitoes Vectors. Journal of Essential Oil-Bearing Plants 19(2): 349-357.
- Hougard JM, Duehon S, Darrirt F, Zaim M, Rogier C, et al. (2003) Comprative performances, under laboratory condition, of seven pyrethroid insecticides used for impregnation of mosquito nets. Bulletin of Word Health Organization 81: 324-323.
- Bhatt RM,Yadav RS, Adak T, Babu CJ (2005) Persistence and washresistance of insecticidal efficacy of nettings treated with deltamethrin tablet formulation (K-O TAB) against malaria vectors. J Am Mosq Control Assoc 21(1): 54-58.
- Bonnet J, Duchon S, Corbel V (2005) WHOPES phase I study of LLINS from BASF. Unpublished report to the WHO Pesticide Evaluation Scheme (WHOPES).
- Dehaki M, Javadian E, Vatandoost H, Abai MR (2008) Comparison the effect of Bed Nets Saturated with Lambdacyhalothrin Insecticide, Bifenthrin and DEET on Blood-Feeding Anopheles stephensi (Diptera: Culicidae). The Vector of Malaria 15(72): 13-20.
- Duchon S, Bonnet J, Corbel V (2005) Wash resistance and efficacy of long-lasting insecticide nets from BASF against susceptible mosquitoes of Anopheles gambiae. Unpublished report to the WHO Pesticide Evaluation Scheme (WHOPES).
- Elissa N, Curtis CF (1995) Evaluation of different formulations of Deltamethrin in comparison with Permethrin for impregnation of netting. Pesticide Science 44: 363367.
- Gonzalez JO, Kroeger AI, Pabon E (2002) Wash resistance of insecticide treated materials. Transactions of the Royal Society of Tropical Medicine and Hygienic 96(4): 370-375.
- Hougard JM, Duehon S, Darrirt F, Zaim M, Rogier C, et al. (2003) Comparative performances, under laboratory conditions, of seven pyrethroid insecticides used for impregnation of mosquito nets. Bull World Health, Organization 81: 324-333
- Malima RC, Magesa SM, Tungu PK, Mwingira V, Magogo SF, et al. (2008) An experimental hut evaluation of Olyset® nets against anopheline mosquitoes after seven years use in Tanzanian villages. licensee BioMed Central Ltd 38.
- Sharma SK, Upadhyay AK, Haque MA, Padhan K, Tyagi PK, et al. (2006) Wash resistance and bioefficacy of Olyset net--a long-lasting insecticide-treated mosquito net against malaria vectors and non-target household pests. J Med Entomol 43(5): 884-888.
- Vythilingam I, Zainal AR, Hamidah T (1999) Laboratory evaluation of lambdacyhalothrin a microencapsulated formulation on mosquito nets for control of vector mosquito. Southeast Asian J Trop Med Public Health 30(1): 177-183.
- WHO (1997) Guidelines on the use of insecticide-treated mosquito nets for the prevention and control of malaria in Africa? CTD/MAL/AFRO/97.4, Geneva.
- (2014) Pulcra Chemicals LLC. Skintex MR III blanket. [Unpublished dossier report to the WHO Vector Control Advisory Group (VCAG)].
- Graham K, Mohammad N, Rehman H, Farhan M, Kamal M, et al. (2002) Comparison of three pyrethroid treatments of top sheets for malaria control in emergencies: entomological and user acceptance studies in an Afghan refugee camp in Pakistan. Med Vet Entomol 16(2): 199-206.
- Rowland M (1999) Permethrin-treated chaddars and top-sheets: appropriate technology for protection against malaria in Afghanistan and other complex emergencies. Trans R Soc Trop Med Hyg 93: 465-472.
- Macintyre K, Sosler S, Letipila F, Lochigan M, Hassig S, et al. (2003) A new tool for malaria prevention? Results of a trial of permethrin-impregnated bedsheets (shukas) in an area of unstable transmission. Int J Epidemiol 32: 157-160.

 Review Article
Review Article