Abstract
Introduction: This review discuss about how to avoid perioperative pressure ulcers. Surgical patients have a high risk of pressure ulcer development in preoperative and postoperative stages. Here we will share about the management and some preventive measures to avoid pressure sores in perioperative patients.
Method: Pubmed, Ovoid, Ebase, google academic, Electronic databases including: Cochrane Library, MEDLINE, Scopus, CINAHL, SID, Iran Doc, ProQuest.
Discussion: There are so many studies conducted till now about the management of pressure ulcer in perioperative patients. Multy layer dressing, using alternative pressure mattress and vesico-elastic polymer pad (gel pad) on the operating table during surgery, patients’ and caregivers’ education on nutrition and skin care, frequent repositioning, and the use of positioning wedges are clinically demonstrated benefits for preventing pressure ulcers or accelerating the healing of pressure ulcers.
Conclusion: Conscientious effort is needed to prevent the development of hospitalacquired pressure ulcers (HAPU) through the early identification of risk and early implementation of preventive measure. Here we will compare all the available methods that prevent perioperative pressure ulcers.
Keywords: PU-Pressure Ulcers; HAPUHospital- Acquired Pressure Ulcers; Spinal Cord Injured -SCI; HDF-High-Density Foam Pads; VP-Viscoelastic Polymer; PCAPatient Controlled Anesthesia; MDRPUMedical Device Related Pressure Ulcer
Introduction
Pressure ulcers (PU) occur mainly in bedridden patients and are difficult to manage and treat once they develop. Patients who are unable to change their position because of spinal cord injury, cerebrovascular accident or general weakness are at a high risk of developing PU. These patients are typically elderly, have a long hospital stay and often have multiple comorbidities. The perioperative period is the time period of a patient’s surgical procedure. It commonly includes ward admission, anesthesia, surgery, and recovery. Perioperative may refer to the three phases of surgery: preoperative, perioperative, and postoperative, though it is a term most often used for the first and third of these only - a term which is often specifically utilized to imply ‘around’ the time of the surgery. Pressure ulcers can induce serious problems during patient care processes. A pressure ulcer is an area of localized damage to the skin and underlying tissue caused by pressure, shear, friction, and/or a combination of these. Recent studies have suggested that the overall incidence of pressure ulcers in the hospital range from 1%-11%, whereas the range varies between 4.7% and 66% among surgical patients. Different kinds of prevalent pressure ulcers have been reported in different countries, ranging from 10.1%-23.1%.
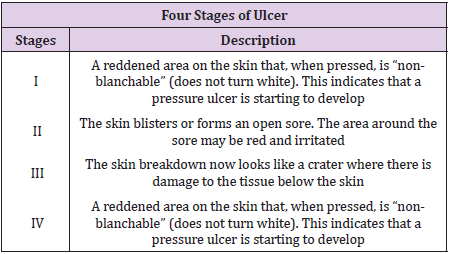
This indicates that surgical patients are usually at a high risk of developing pressure ulcers. The incidence of pressure ulcer leads to greater misuse of nursing resources and high medical costs. Pressure ulcers are not only adverse events in a hospital stay, that have to be treated and justified, but represent also a quantifiable risk in terms of morbidity and mortality. Adjusted for hospital, diagnosis related group (DRG), sex, race and age group, a case-control study revealed 3.98 extra days in hospitals and 7.23% attributable mortality, if a pressure ulcer occurs (Zhan & Miller 2003). From 1990-2001, pressure ulcer was mentioned as one cause among others for 3.79 deaths per 100,000 population in the USA (Redelings et al. 2005) as against the single underlying cause in 18.7%. The authors identified a high concurrence with sepsis (39.7% of all deaths with indication of a pressure ulcer). The risk factors associated with pressure ulcers amount to more than 100 and include medical diagnoses, patients’ demographic characteristics, anthropometrics, physiological status, nutritional status, and hospital environment, among others. The occurrence of pressure sores is a main obstacle to the long term rehabilitation of spinal-cord injured patient [1-3] (Table 1).
To achieve the best functional result with the most efficient use of resources, a comprehensive treatment plan is needed, that include preoperative workup, physical therapy, nutritional considerations, wound care, treatment of spasticity and reflex spasm, pre and postoperative bowel management, pulmonary consideration, anesthetic consideration, antimicrobial regimen. Surgical patients are prone to developing HAPU. In the United States, patients with HAPU had a longer length of stay, higher total hospitalization costs, and greater odds of readmissions compared with patients with no HAPU. Preventing HAPU involves accurate and ongoing risk assessments so that preventive measures can be implemented as early as possible and carried out throughout the period of immobility. The prevalence of HAPU among surgical patients is about 8.5% or higher depending on the type and the duration of the surgery. Patients with proximal femur fractures or patients after major lower limb amputation, the incidence of pressure ulcers was high (10.4% and 8.8%, respectively). Patients undergoing bowel surgery and peripheral vascular reconstructions are also prone to developing pressure ulcers. Several plausible mechanisms might be accounting for increasing risk of infections in relation to prior pressure sore exposures [4-6]. To start with, pressure sores were perceived to induce impairment of skin protection function by destroying integrity of erythematous skin and prompting reproduction and growth of pathogenic bacteria.
Pressure ulcers might introduce possible resources and entrances of pathogens to human body, which was possible to result in local infections in human body. Secondly, chronic pressure ulcers were supposed to persist chronic inflammation, which might lead to stimulation of cytokines and inflammation factors. An expansive literature suggest that long-term and excessive consumption of cytokines and inflammation factors might be accounting for immune suppression, and in turns led to a weaken ability to prevent invasions and attacks of pathogens. Thirdly, immobilization, as a primary risk factor for the occurrence and development of pressure sores, was considered to be associated with pneumonia. Immobilization might have destructive effects on removing function of bronchial secretions, which was conductive to reproduction of pathogen and help to result in pneumonia. Studies demonstrates an increased risk of several specific infections (surgical incision infection, pneumonia, urinary tract infection) within 14-day after spinal cord operation in patient with pressure sores preoperatively. Among the four stages of pressure ulcer, stage IV has the highest risk of postoperative infections. Intensive care units (ICUs) have the highest PU incidence rates in health care settings, which have been reported as high as 50% .The high rates in the ICUs can be attributed to the high acuity of patients, the nature of their critical illness and the highly invasive nature of the interventions and therapies that critically ill patients receive. Identifying patients at risk for PU development is essential for the effective implementation of PU prevention programs and usage of resources [7-10].
Method
Cochrane Library, MEDLINE/ PubMed, Scopus, CINAHL were used. The search was limited to the English language. In a final search, the reference lists of the included articles were also handsearched to identify further relevant articles.
Eligibility Criteria
Studies met the inclusion criteria if they assessed the effects of preventive measures on surgical patient. If the full text of an article could not be obtained, we included its abstract only when it had sufficient data.
Study Selection
Two independent reviewers screened and selected articles based on the title, subsequently on abstract and finally on full text. Disagreements were resolved via discussion with a third reviewer.
Data Extraction
The following information was extracted from the studies that met the eligibility criteria:
a. first the author’s name and year of publication;
b. participant characteristics (country of origin, sample size and mean age);
c. study characteristics (methods of participant allocation, allocation concealment, blinding, drop-out rates and reasons for drop-outs);
d. nature of aromatherapy intervention (type, dose, duration, route of administration for experimental and control interventions);
e. outcomes (instrument used to assess anxiety and outcome data).
Quality Assessment
The risk of bias of the included studies was assessed independently by two reviewers using the Cochrane Collaboration’s ‘Risk of bias’ tool. The criteria consisted of selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), and reporting bias (selective outcome reporting). Each item was classified as ‘low risk of bias’, ‘high risk of bias’, or ‘unclear risk of bias’. Disagreements were resolved by discussion between two reviewers.
Description
Pressure ulcer development was strongly correlated with indication for admission. In specific patient categories, such as patients with proximal femur fractures or patients after major lower limb amputation, the incidence of pressure ulcers was high (10.4% and 8.8%, respectively). Patients undergoing bowel surgery and peripheral vascular reconstructions are also prone to developing pressure ulcers [11-15].
Preoperative Work-Up
Patient Candidacy: Prior to becoming a candidate for reconstructive surgery, the patient must be prepared physically and mentally endure 6-10 weeks of hospitalization. Patient exhibits selfmotivation since a successful result is obtainable only with patient cooperation. The team approach for spinal cord injured patient. The physical medicine and rehabilitation physician is the primary care doctor for the spinal cord injured patient and intimately involved with perioperative care. Before a procedure the patient must be in optimum physical health, be free of spasms and contractures, be in adequate nutritional status, be able to tolerate the prone position (if needed) and have adequate pulmonary function.
Physical Therapy for SCI Patients: The role of physical therapist have great importance in the care of SCI patient, that prevent contractures. The exercise and proper positioning in bed combat the deforming forces caused by paralysis and spasticity. Custome cut out cushions are useful in proper positioning. The occupational therapy department aids our patient with positioning which causing iatrogenic skin problems. A pressure pad evaluation aids the selection of a cushion with the best pressure distribution properties for the patient with a tendency towards decubitus ulcers.
Preoperative Positioning: Surgical candidates must tolerate prone position for a minimum of 4 weeks postoperatively and must exhibit operatively the ability to maintain the position adequately. Position individualized according to the location of pressure sores. Prone position is mostly applied since the pressure ulcer seen in ischial, sacral, and trochanteric area mainly. The prone position is assumed for 4 week postoperatively with side-side movement and range of motion beginning 6-7 week post operatively.
Nutritional Consideration: Before surgery nutritional status must have priority. The serum albumin level should be greater than 35g/100ml, the lymphocytic count should be greater than 220g%. Delayed cutaneous hypersensitivity is also indicator of decreased visceral protein. Inability to respond to placement of purified protein derivative, mumps, or candida antigens correlate and with higher rates of sepsis and high mortality rates in acute surgical patient.
Wound Care
Preoperative Wound Care: The care of the open ulcer consists of debridement of obviously devitalized tissue. Debridement is done surgically just to the point of bleeding with additional debridement accomplished by frequent dressing changes using mesh gauze sponges/kerlix to debride the wound, decrease the bacterial count. The use of povidone - iodine offer no therapeutic benefit over the use of saline in wound treatment.
Roengenograms: Chest and pelvic roentgenograms are routinely done preoperatively. If there is a large wound with a tracking sinus, a simple sinogram is performed using radio opaque dye injected through a foley catheter to evaluate the extent of the ulcer and help in the preoperatively planning for reconstruction.
Treatment of Spasticity and Reflex Spasms: Excessive reflex activity below the level of the upper motor neuron lesion often exists after a spinal cord injury. The obliteration of supraspinal inhibitory pathways is the reason postulated for this phenomenon. In the immediate postoperative period the spasms can cause bleeding and hematoma that may result in flap necrosis.
Medical Treatment: The drug of choice at the institute for rehabilitation and research is baclofen, which is believed to act centrally and poly synaptically within the spinal cord and brain stem. This begun at a dosage of 5-10mg 4 times a day, not to exceed 100mg daily. Side effects are minimal in patient with SCI, however with a dosage greater than described memory lose and confusion may occur. Diazepam may be used alone or with baclofen. It acts centrally within the brain stem and cerebral cortex to affect spasticity with initial dosage 5mg a day until a total use of 40mg a day is reached. Dantrolene can also be used for the treatment of spasms, it acts on excitation-contraction coupling mechanism of muscle fiber itself. It has a bed effect on liver so that serum glutamic pyruvic transaminase must be monitored monthly. Initial dosage is 25mg twice a day, increased to 25mg 4 times a day then by 25mg increment every third to fifth day to a maximum 200mg daily.
Surgical Management of Spasms
Nerve Blocks: Usefulness of peripheral nerve block is primarily confined to patients who have incomplete lesions and who are not candidates for subarachnoid blocks, since we want to preserve as much sensation and useful motor functions initial attempt with lidocaine, have to repeat as needed.
Epidural Stimulator: Most useful in patients with incomplete lesions but costly.
Subarachnoid Blocks (Phenol Rhizotomy): Useful for patients with complete lesions. Specific for lower extremities and don not affect the trunk and upper extremities.
Urological Management
Initially indwelling catheter is utilized following by intermittent catheterization with or without a condom catheter. Patients who are not voiding or who have high residuals are given methenamine as well as ammonium chloride (1 mg of each every 6 hrs).
Proper Diet and Bowel Management: We have found that even the most complex pressure sores can be successfully managed without a diverting colostomy.The preoperative regimen begun 3 days prior to surgery with a clear liquid diet. The bowel is cleansed with enemas and mild laxatives.
Postoperative Diet and Bowel Management: The clear liquid diet is continued for 5 days postoperatively.1 tab (2.5mg) twice a day is given for 5 days to constipate patient. If contamination does occur the area is thoroughly cleansed and dried immediately. The patient resume their prior bowel program on the 6th day postoperatively.
Antimicrobial Regime for the Decubitus Ulcer: Clinical and experimental studies indicate that anti-microbial agents prevent infection when effective concentrations are prevent infection when effective concentration are present in tissues during or shortly after the surgical procedure. Maximum bacterial shedding occurs during this time. A single parenteral dose of antimicrobial agent is given just prior to surgery, providing adequate tissue levels throughout the procedure. Antibiotics are selected on the basis of preoperative cultures and sometimes modified when the result of intraoperative cultures are known. The duration of administration of antimicrobial agents is individualized, based on the extent inflammation, suppuration, sinus tracts, and bone involvement.
Septic Patient with Decubitus Ulcer: The sin qua none of the treatment of sepsis associated with decubitus ulcer is surgical debridement. The antibiotic regimen is also need for aerobic and anaerobic bacteria.
Pulmonary Consideration: Vital capacity is measured preoperatively in the prone and supine position. After the patient position is changed, he or she is observed for clinical signs of respiratory embarrassment, Arterial blood gas may be obtained 20 minutes after the patient’s position changed.
Sitting Regimen: A pressure pad evaluation must be performed postoperatively to determine new sitting surface requirement. Sitting is begun in the sixth or seventh postoperative week, beginning with 30 minutes of sitting twice during the first day. Lanolin massage of surgical site keeps the area soft and moist. However, pressure ulcer rates can only be used as an indicator of quality of care if certain crucial aspects of data collection and interpretation are taken into account. The VP pad is better than the HDF pad in relieving pressure. However, the measured average pressures for both types of pads were all higher than the threshold value of the capillary closing pressure (32mmHg; Schultz, 2005). Neither of them could reduce the pressure below the capillary closing pressure, which may have contributed to the occurrence of pressure ulcers in both groups. Both the average and peak pressures, measured after applying the VP pads, were significantly lower compared to measurements of the HDF pad; however, there was no significant difference between the two types of pad regarding the prevention of pressure ulcers.
Obese individuals had significantly lower values of surface pressure and shear force than slender individuals at the coccygeal bone site. At the sacral bone site and the thigh site, the values of surface pressure in the obese group were significantly higher than those of the slender group. The reason why obese subjects had higher values was not obvious, but the magnitude of pressure at the sites was low, and so the effect of bony prominences would not be apparent by weight distribution in the obese types. In clinical practice, subjects should be positioned at the bending conformity point or shifted 10cm from that point toward the head of the bed whenever bed operations are performed in order to avoid generating harmful shear forces and surface pressures. There are multiple possible reasons behind the correlation between PCA use and increased pressure ulcer incidence. Frist, the use of a PCA pump can relieve the sense of pain, a decreased sensation and blocked motor nerve owing to a PCA pump might accelerate the development of pressure ulcers. Meanwhile movement actually can be considered self protection for bedridden patients, however PCA can reduce the patient’s sense of pain so that they will reduce their movement, which can reduce the patient’s ability to self protect. Similarly the use of PCA may make patients over emphasize the disease severity so that they may fear moving.
Second because a PCA pump can relieve painful sensations, patients may be less willing to move in order to stay comfortable. Third in order to avoid the events of catheter prolapse and compression, postoperative patients are fearful of moving. Bed- or wheelchair-bound patients tend to suffer from multiple pressure sores and often undergo several operations over the years for reconstruction of the tissue’s integrity. This makes every pressure sore recurrence over previously reconstructed and therefore scarred tissue more complex to treat. Fillet flaps from nonfunctioning body parts not only impose little or no donorsite morbidity but can also prolong pressure sore recurrence by offering robust tissue for padding. In paraplegic patients with massive or bilateral pressure sores, where all other reconstructive measures have been exhausted, fillet flaps offer a last resort option for pressure sore management.
Conclusion
Conscientious effort is needed to prevent the development of HAPU through the early identification of risk and early implementation of preventive measure. So in my opinion when we compare all the points in discussion most applied and applicable method to achieve the best functional result with the most efficient use of resources, a comprehensive treatment plan is needed, that include preoperative workup, physical therapy, nutritional considerations, wound care, treatment of spasticity and reflex spasm, pre and postoperative bowel management, pulmonary consideration, anesthetic consideration, antimicrobial regimen. The majority of MDRPUs were related to poor positioning or fixation of respiratory equipment. Occurrence of these ulcers could be prevented with implementation of preventive strategies such as regular assessment of the area underneath and around medical devices and regular repositioning or securement of devices (45). Using protective dressings to secure and stabilize devices also could reduce the risk for MDRPU development.
References
- Fazila Aloweni, Shin Yuh Ang, Stephanie Fook Chong, Nurliyana Agus, Patricia Yong, et al. (2019) A prediction tool for hospital-acquired pressure ulcers among surgical patients: Surgical pressure ulcer risk score. Int Wound J 16(1): 164-175.
- Lardenoye JW, Thiéfaine JA Breslau PJ (2009) Assessment of Incidence, Cause and Consequences of Pressure Ulcers to Evaluate Quality of Provided Care. Dermatol Surg 35(11): 1797-1803.
- FWA Van Asbeck, MWM Post (2015) Bedside prediction of the progress of pressure ulcer healing in patients with spinal cord injury using the ‘Decu-stick’. Spinal Cord 53(7): 539-543.
- Chao Ton Su , Pa Chun Wang, Yan Cheng Chen, Li Fei Chen (2012) Data Mining Techniques for Assisting the Diagnosis of Pressure Ulcer Development in Surgical Patients. J Med Syst 36(4): 2387-2399.
- Yang Y, Sun L, Liu N, Hou X, Wang H, et al. (2015) Effects of Noninvasive Positive-Pressure Ventilation with Different Interfaces in Patients with Hypoxemia after Surgery for Stanford Type A Aortic Dissection. Med Sci Monit 21: 2294-2304.
- Wu T, Wang ST, Lin PC, Liu CL, Chao YF (2011) Effects of Using a High-Density Foam Pad Versus a Viscoelastic Polymer Pad on the Incidence of Pressure Ulcer Development During Spinal Surgery. Biol Res Nurs 13(4): 419-424.
- Lei luo Yang, Wu xun Peng, Chun qing Wang, Qing Li (2018) Elevated Risk of Infections after Spinal Cord Surgery in Relation to Preoperative Pressure Ulcers: a Follow-up Study. Sci Rep 8(1): 14027.
- Hyun Ho Han, Jun Gul Ko, Jong Won Rhie (2017) Factors for postoperative complications following pressure ulcer operation: stepwise multiple logistic regression analysis. Int Wound J14(6): 1036-1040.
- Stausberg J, Nils Lehmann, Knut Kroger, Irene Maier, Helmut Schneider, et al. (2010) Increasing pressure ulcer rates and changes in delivery of care: a retrospective analysis at a University Clinic. J Clin Nurs 19(11-12): 1504-1509.
- Mimura M, Ohura T, Takahashi M, Kajiwara R, Ohura N (2009) Mechanism leading to the development of pressure ulcers based on shear force and pressures during a bed operation: Influence of body types, body positions, and knee positions. Wound Repair Regen 17(6): 789-796.
- Van Leen M, Halfens R, Schols J (2018) Preventive Effect of a Microclimate-Regulating System on Pressure Ulcer Development: A Prospective, Randomized Controlled Trial in Dutch Nursing Homes. Adv Skin Wound Care 31(1): 1-5.
- Nahla Tayyib, Fiona Coyer, Peter Lewis (2016) Saudi Arabian adult intensive care unit pressure ulcer incidence and risk factors: a prospective cohort study. Int Wound J 13(5): 912-919.
- Daniel H Fulkerson, Shobhan Vachhrajani, Alison Brayton, Abhaya V Kulkarni, Andrew Jea (2010) The Perception of Complications in Pediatric Spine Surgery: A Comparative Survey of Surgeons, Caregivers and Patients. Pediatr Neurosurg 46(3): 213-220.
- Ling Gao, Lina Yang, Xiaoqin Li, Jin Chen, Juan Du, et al. (2018) The use of a logistic regression model to develop a risk assessment of intraoperatively acquired pressure ulcer. J Clin Nurs 27(15-16): 2984-2992.
- Iakovos Georgiou, Philipp Kruppa, Mojtaba Ghods (2019) Use of a Total Leg Fillet Flap to Cover Multiple Pelvic Pressure Ulcers. Plast Reconstr Surg Glob Open 7(1): e2084.

 Review Article
Review Article