Abstract
Internal rotation gait (IRG) is a common problem in children with cerebral palsy and increased femoral anteversion (FAV) is assumed to be a main cause. Therefore, femoral derotation osteotomy (FDO) is the current standard to restore regular angles (foot in direction to gait). The purpose of this study was to investigate if there is a correlation between FAV and IRG during stance phase. Clinical, radiological and 3D-gait analysis of 37 patients (24 boys, 13 girls, mean age 14.1 ± 3.2 years) showed no correlation between hip internal rotation (HIR) and real femoral anteversion (rFAV) during gait in cerebral palsy (CP). We consider other factors like indirect effects resulting from spastic equinus and/or dynamic factors of muscles to be considered as cause of hip internal rotation gait. Furthermore, it is shown that measured FAV in clinical examination (cFAV) did not correlate with the radiologically measured rFAV by standardized anteroposterior pelvic radiographs and the Dunn projection.
Abbreviations: cER: Maximal Hip External Rotation, cFAV: Clinical Femoral Anteversion; cIR: Maximal Hip Internal Rotation, cMV: Middle Value of Hip Internal Rotation, CP: Cerebral Palsy; cTT: External Tibial Torsion; EMG: Electromyography; FAV: Femoral Anteversion; FDO: Femoral Derotation Osteotomy FP: Foot Progression; FR: Foot Rotation; FDO: Femoral Derotation Osteotomy; GDI: Gait Deviation Index; GGI: Gillette Gait Index; GMFCS: Gross Motor Function Classification System; GPS: Gait Profile Score; HIR: Hip Internal Rotation; IRG: Internal Rotation Gait; MAP: Movement Analysis profile; rFAV: Real Femoral Anteversion; RoM: Range of Motion
Keywords: Cerebral Palsy; Femoral Anteversion; Internal Hip Rotation Gait; Femoral Derotation Osteotomy; 3D Gait Analysis
Introduction
Internal rotation gait (IRG) is a common problem in children with cerebral palsy (CP). A frequency up to 64 % has been reported [1]. It is a common doctrine that increased femoral anteversion (FAV) is one of the most important factors [2] causing IRG. Other common factors thought to contribute are compensatory mechanisms for decreased abduction moment arm, increased muscle tone of hamstrings and/or adductors [3,4], increased muscle tone of the anterior glutei [5], increased internal rotation moment arms because of hip flexion deformity and maybe other factors as equinus of the foot [6]. But the underlying biomechanics and causes of IRG are not clearly identified. Therefore, it is not surprising that the various treatment options such as addressing soft tissue procedures and bony interventions reflect these ideas.
The femoral derotation osteotomy (FDO), proximal or distal, is the current standard treatment for IRG with the aim to correct the increased FAV. Pirpiris et al. reported excellent correction of rotation of the hip and foot progression angles in children with spactic diplegia comparing FDO at both levels, proximally or distally [7]. Besides the fact, that several outcome study reports are controversial (a recurrence rate of IRG up to 33% after FDO [8], or even higher with recurrence rate of 40% [9]) FDO is still the standard procedure for correction. Schwartz et al. reported that limbs with anteversion and significant internal hip rotation during gait benefit from an FDO, but limbs with excessive FAV and only mild internal hip rotation are at risk of developing an excessive external foot progression angle [10]. The aim of this study was to investigate if there is a correlation between FAV and IRG for the stance phase during gait in patients with CP.
Materials and Methods
Medical records and gait laboratory data were reviewed retrospectively. All children with CP who were scheduled for multilevel orthopedic surgery between February 2008 and April 2011 were included in this study. All participants had a preoperative 3D gait analysis (3-DGA) including a thorough clinical examination, a radiological assessment with standardized anteroposterior pelvic radiographs and Dunn projections. 33 patients met the inclusion criteria as well as 4 patients with other similar neurological syndromes (due to chromosomal abnormalities), resulting in 37 participants with 74 femurs. 18 patients with CP had spastic diplegia and 15 suffered from quadriplegia. The Gross Motor Function Classification System (GMFCS) level of the participants was I for 6, II for 19 and III for 12 patients. There were 24 boys and 13 girls with a mean age of 14.1 ± 3.2 years (range: 7-22 y). Clinical femoral anteversion (cFAV), clinical external tibial torsion (cTT), maximal hip internal (cIR) and external rotation (cER) in extension were measured clinically. The real femoral anteversion (rFAV) angle was calculated from the standardized anteroposterior pelvic radiograph and the Dunn projection. Foot progression (FP), foot rotation (FR), and hip internal rotation (HIR) angles were determined by 3-DGA (only from the stance phase).
All patients had a 3-DGA performed by a physiotherapist and a human movement scientist both experienced in gait analysis. The clinical assessment included the examination of the passive range of motion (RoM), spasticity according to the modified Ashworth/ Bohannon scale [11] (scale: 0 - 4), and the manual muscle strength test [12,13] (scale: 0 - 5) of the ankle dorsi- and plantarflexors. The preoperatively instrumented gait analysis included kinematics, kinetics, and dynamic surface electromyography (EMG), using a motion capture system (6 camera VICON 460 system, Oxford Metrics Ltd., UK), 2 force plates (Kistler Instrumente AG, Winterthur, Switzerland) and an 8-channel surface EMG system (Neurodata GmbH, Vienna, Austria). The patients walked barefoot at their selfselected speed. The Helen Hayes Marker set [12] was used and at least 6 trials were recorded. Anthropometric data were recorded for appropriate scaling. Surface EMG was recorded simultaneously. Bipolar Ag/AgCl surface electrode pairs (electrode diameter 10 mm and an inter-electrode spacing 22 mm) were placed bilaterally over the medial gastrocnemius, tibialis anterior, rectus femoris, and semitendinosus muscles. For electrode placement, the SENIAM recommendations for surface EMG were followed [14].
The ground electrode was placed over the tibial tuberosity. The EMG signals were band-pass filtered (10-700 Hz) and collected at a sampling rate of 2500 Hz. All data were expressed as a percentage of gait cycle using the Polygon software (Oxford Metrics Ltd., UK). From the 3D gait data temporalspatial parameters (cadence, stride length, and walking speed), the Gillette Gait Index (GGI), the Gait Deviation Index (GDI), the Movement Analysis profile (MAP) and the Gait Profile Score (GPS) were calculated for all patients pre- and postoperatively for group I and II separately [15-17]. For statistical analysis first a Shapiro-Wilk normality test was performed to verify that the data met the assumptions of a parametric test. The Pearson and Spearman rho correlation coefficient was calculated to analyze the correlations between normally and not-normally distributed data, respectively. The level of significance for all tests was set at p ≤ 0.05.
Results
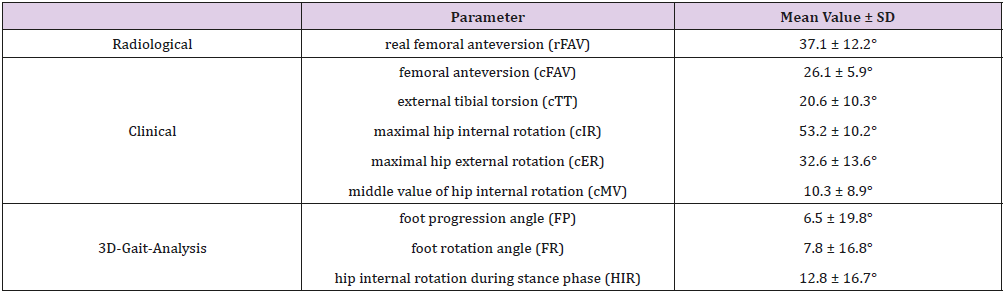
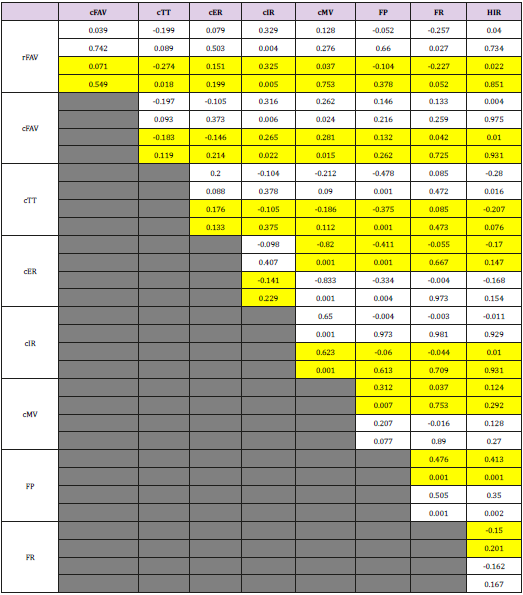
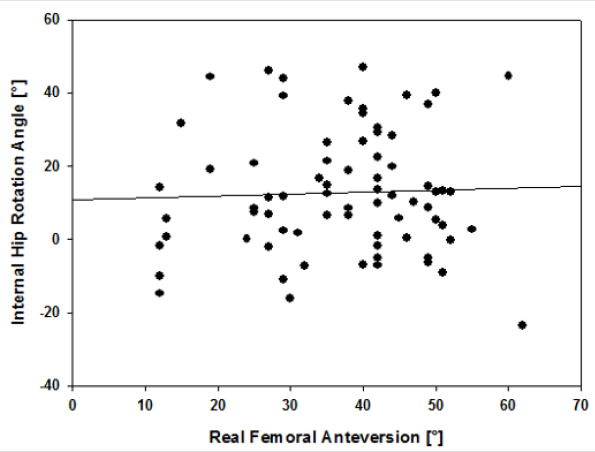
The analysis of the data showed a calculated rFAV of 37.1 ± 12.2°, a cFAV of 26.1 ± 5.9°, a cTT of 20.6 ± 10.3°, a hip cIR of 53.2 ± 10.2° and a hip cER of 32.6 ± 13.6°. The middle value of hip rotation (cMV) was 10.3 ± 8.9° towards internal. The results from 3-DGA presented a FP angle of 6.5 ± 19.8°, a FR angle of 7.8 ± 16.8°, and a HIR angle of 12.8 ± 16.7°. There was a positive correlation between rFAV and cIR (r = 0.32, p = 0.005) and negative correlation between rFAV and cTT (r = -0.27, p = 0.02) and FR (r = - 0.23, p = 0.05). cFAV correlated positively with cIR and cMV (r = 0.27 and 0.28, p = 0.02 and 0.02). There was no correlation, however, between rFAV and cFAV (r = 0.07, p =0.55). cTT correlated negatively with FP and HIR (r = -0.38 and -0.21, p = 0.001 and 0.08). FP correlated positively with FR and HIR (r = 0.48 and 0.41, p = 0.001 and 0.001). Interestingly there was no correlation between rFAV and HIR (r = 0.02, p = 0.85), see Figure 1. The results are summarized in Table 2.
Table 2: rFAV=Real Femoral Anteversion, cFAV=Clinical Femoral Anteversion, cTT=Clinical External Tibial Torsion, cER=Clinical Maximal Hip External Rotation in Extension, cIR=Clinical Maximal Hip External Rotation in Extension, cMV= Middle Value of Hip Rotation, FP=Foot Progression Angle in 3-DGA, FR=Foot Rotation Angle in 3-DGA, HIR= Hip Internal Rotation during Stance Phase in 3-DGA.
Note: Data highlighted in yellow are normally distributed. The first row shows the rho-correlation coefficient (r), the second the level of significance (p) respectively.
Figure 1: The correlation plot demonstrating the poor relationship between the real femoral anteversion and the internal hip rotation angle.
Discussion
Although FAV is commonly thought to be one of most important factors for IRG, our data do not show any correlation between radiologically assessed rFAV and HIR during stance phase assessed by 3-DGA in patients with CP. This result suggests that IRG may be independent from FAV. Indeed, it has been shown by modelling that FAV is a reaction on the external forces on the growing hip in CP [18]. It may even be questioned whether FAV persists after birth or whether it is a reactive shape according to the acting forces. The doctrine that the IRG is a compensatory mechanism to restore the abduction lever arm of the gluteus medius in patients with increased FAV [19] is in our opinion still debatable. Other results, such as the high recurrence or persistence rate of IRG after FDO [8,20] and studies on biomechanical connections [6,21] also argue for the existence of other factors influencing the rotation during gait in CP.
Our results confirm the hypothesis that there is no correlation between FAV (rFAV and cFAV) and HIR in the majority of patients with CP. Even if there would be a secondary bony deformation due to pathological forces, a correlation between FAV and IRG should have been obvious. In contrast to the studies of Kim et al [20] and de Morais Filho et al [8], where the FAV was measured in clinical examination and intraoperatively, we calculated the rFAV by standardized anteroposterior pelvic radiographs and the Dunn projection and took it as relevance value for FAV. In our study the rFAV and the cFAV did not correlate, which shows a limitation of one of the procedures and support the findings of Sangeux et al. [22]. The Dunn and ap assessment were favored against CT-scan torsional studies because it permits a picture where both levels are shown simultaneously. In CT scans in contrast, CP patients are not reliable to lie steadily and not rotate the leg internally between the scans.
Conclusion
Our results do not support the common doctrine that FAV is the most important factor which causes internal hip rotation during gait in cerebral palsy. There was no correlation between hip internal rotation during gait in cerebral palsy and real femoral anteversion determined radiologically. The latter, however, correlates with maximal hip internal rotation during clinical assessment with the hips extended. Distally, external tibial torsion in contrast correlates negatively with internal hip rotation and foot progression from 3-DGA. Therefore, other factors such as indirect effects resulting from spastic equinus [6] must be considered as a cause of hip internal rotation during gait.
Acknowledgement
The authors thank Alexsej Barg for the statistical analysis.
Conflicts of Interest
No conflicts of interest are to declare.
References
- Wren TA, Rethlefsen S, Kay RM (2005) Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Ortho 25(1): 79-83.
- O'Sullivan R, Walsh M, Hewart P, Jenkinson A, Ross LA, et al. (2006) Factors associated with internal hip rotation gait in patients with cerebral palsy. J Pediatr Orthop 26(4): 537-541.
- Sutherland DH, Schottstaedt ER, Larsen LJ, Ashley RK, Callander JN, et al. (1969) Clinical andelectromyographic study of seven spastic children with internalrotation gait. J Bone Joint Surg Am 51(6): 1070-1082.
- Arnold AS, Delp SL (2001) Rotational moment arms of the medial hamstrings and adductors vary with femoral geometry and limb position: implications for the treatment of internally rotated gait. J Biomech 34(4): 437-447.
- Presedo A, Oh CW, Dabney K W, Miller F (2005) Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J Bone Joint Surg Am 87(4): 832-841.
- Brunner R, Dreher T, Romkes J, Frigo C (2008) Effects of plantarflexion on pelvis and lower limb kinematics. Gait Posture 28(1): 150-156.
- Pirpiris M, Trivett A, Baker R, Rodda J, Nattrass GR, et al. (2003) Femoralderotation osteotomy in spastic diplegia. Proximal or distal? J Bone JointSurg Br 85(2): 265-272.
- de Morais Filho MC, Kawamura CM, dos Santos CA, Mattar R (2012) Outcomes of correction of internal hip rotation in patients with spastic cerebral palsy using proximal femoral osteotomy. Gait Posture 36(2): 201-204.
- Church C, Lennon N, Pineault K, Abousamra O, Niiler T, et al. (2017) Persistence and Recurrence Following Femoral Derotational Osteotomy in Ambulatory Children with Cerebral Palsy. J Pediatr Orthop 37(7): 447-453.
- Schwartz MH, Rozumalski A, Novacheck TF (2014) Femoral derotational osteotomy: surgical indications and outcomes in children with cerebral palsy. Gait Posture 39(2): 778-783.
- Bohannon R, Smith MB (1987) Interrater reliability of a Modified Ashworth Scale of muscle spasticity. Phys Ther 67(7): 206-207.
- Kadaba MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8(3): 383-392.
- SC Cuthbert, GJ Goodheart (2007) On the reliability and validity of manual muscletesting: a literature review. Chiropr Osteopat 15: 4.
- Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, et al. (2019) European Recommendations for Surface Electromyography (SENIAM).
- Baker R, McGinley JL, Schwartz MH, Beynon S, Rozumalski A, et al. (2009) The Gait Profile Score and Movement Analysis Profile. Gait Posture 30(3): 265-269.
- Schutte LM, Narayanan U, Stout JL, Selber P, Gage JR, et al. (2000) An index for quantifying deviations from normal gait. Gait Posture 11(1): 25-31.
- Schwartz MH, Rozumalski A (2008) The gait deviation index: a new comprehensive index of gait pathology. Gait Posture 28(3): 351-357.
- Carriero A, Jonkers I, Shefelbine SJ (2011) Mechanobiological prediction of proximal femoral deformities in children with cerebral palsy. Computer Methods in Biomechanics and Biomedical Engineering 14(3): 253-262.
- Arnold AS, Komattu AV, Delp SL (1997) Internal rotation gait: a compensatory mechanism to restore abduction capacity decreased by bone deformity. Dev Med Child Neurol 39(1): 40-44.
- Kim H, Aiona M, Sussman M (2005) Recurrence after femoral derotational osteotomy in cerebral palsy. J Pediatr Orthop 25(6): 739-743.
- Gaston MS, Rutz E, Dreher T, Brunner R (2011) Transverse plane rotation of the foot and transverse hip and pelvic kinematics in diplegic cerebral palsy. Gait Posture 34(2): 218-221.
- Sangeux M, Peters A, Baker R (2011) Hip joint centre localization: evaluation on normal subjects in the context of gait analysis. Gait Posture 34 (3): 324-328.

 Research Article
Research Article