Abstract
A 74-year old patient, admitted to the Intensive Care Unit due to septic shock, presented on the 10th day with anaemia and enlargement of the right thigh, after removal of a central venous catheter the previous day. CT angiography revealed a large haematoma posteriorly to the right Common Femoral Artery (CFA) without active extravasation. As anaemia persisted, ultrasonography (US) revealed an anechoic pulsating cavity (1.54 x 1.40 cm) communicating with the CFA. The diagnosis of CFA pseudoaneurysm was established as bidirectional flow was detected on color Doppler. Ultrasonographic Guided Compression Therapy (UGCT) over 1h thrombosed the pseudoaneurysm. Many access-related complications may occur during the femoral vessel puncture, some of which may warrant urgent surgery, especially in the case of retroperitoneal haemorrhage. For others, such as iatrogenic pseudoaneurysm formation, a watchful waiting approach may be adopted. However, critically ill patients may often present thrombocytopenia or coagulation defects. Therefore, a timely approach is warranted. Although thrombin injection is considered the treatment of choice in pseudoaneurysms, lack of experience and thrombin availability may pose delays in the critically-ill. Ultrasonographic Guided Compression of a pseudoaneurysm is an easy, effective, 24-hour available, bedside treatment modality in the setting of such complications in the critical care.
Case Report
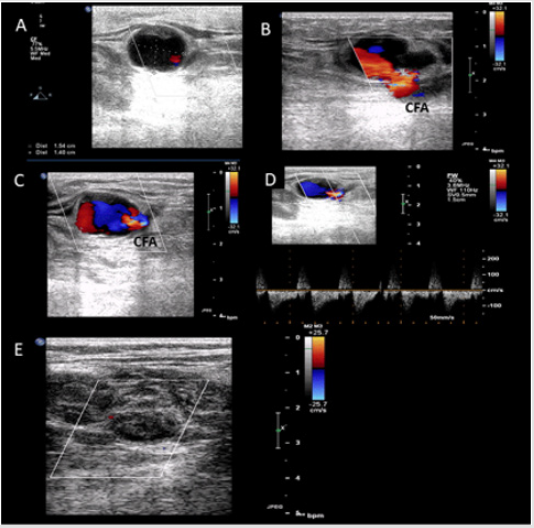
A 74-year old male patient, admitted to the Intensive Care Unit due to septic shock, presented on the 10th day with anaemia (Hct 20%, Platelets 98.000/μL) and enlargement of the right thigh. A central venous catheter had been removed the previous day and so hematoma was suspected. CT angiography revealed enlargement of the muscles of the right thigh and a fluid collection posteriorly to the right Common Femoral Artery (CFM) was evident, although without active extravasation. The patient was under Low Molecular Weight Heparin (LMWH) for thromboprophylaxis, as per protocol for all ICU patients unless there are individualized contraindications. Anaemia did not resolve during the next days, the patient was in need for daily red blood cell transfusions, so ultrasonography (US) was performed, which revealed an anechoic pulsating cavity (1.54 x 1.40 cm) communicating with the Common Femoral Artery (neck: 0.75 cm) (Figure 1). The diagnosis of CFA pseudoaneurysm was established as bidirectional flow was detected on color Doppler, probably having occurred from accidental puncture of the artery, during the central venous catheterization. Percutaneous Ultrasonographic Guided Compression over 1h thrombosed the pseudoaneurysm (Figure 1). The patient’s haematocrit was stabilized and follow up US in the next days confirmed the sealed arterial leak.
Discussion
Iatrogenic pseudoaneurysm formation is an access-related, rather common, complication occurring during the femoral artery puncture, even presenting in the setting of an accidental puncture of the femoral artery, especially in the critically ill [1]. Usually, localized extravasation of blood outside the arterial wall is confined and controlled by the pseudocapsule that develops. In our case, critical illness and the use of anticoagulation, led to persistent arterial bleeding and pseudoaneurysm formation, although information from the CT angiography did not support active extravasation. In ICU patients, under sedatives and analgesics as in our case, significant groin pain, which is the usual clinical finding in CFA pseudoaneurysm, may be overlooked. Suspicion for iatrogenic pseudoaneurysm (IPA) should be increased after any percutaneous femoral access that results in substantial tissue swelling, particularly among high risk patients (increasing age, use of anticoagulation). Typically, clinical findings suggestive of IPA are noted soon after the procedure, often within the first 24 hours after sheath removal.
Figure 1: A. Ultrasonographic examination of the right inguinal region revealing a cavity 1.54 cm x 1.40 in size (7,07 cm2). B and C. Color Doppler revealing active communication of the Common Femoral Artery with the cavity. In C bidirectional flow is evident (simultaneous visualization of red and blue color forming the “ying-yang” sign) D. Pulsed Wave Doppler demonstrating bidirectional blood flow in the neck of the cavity. E. One-hour Percutaneous Ultrasonographic Guided Compression resulted in thrombosis of the pseudoaneurysm.
The diagnosis of a CFA pseudoaneurysm is confirmed with duplex ultrasonography revealing hypoechoic collections, while color flow imaging differentiates a pseudoaneurysm from a simple hematoma collection, revealing bidirectional blood flow in the hypoechoic collection. Color flow can aid in the anatomic characterization of the aneurysm (size of the sack, neck diameter, number of sacks), and the characteristic demonstration of the “ying-yang” shape of the flow, as blood enters and leaves the aneurysmal sack [2,3]. Regarding treatment, a watchful waiting approach is adopted for uncomplicated pseudoaneurysms less than 3 cm in diameter [3]. The mean time to spontaneous thrombosis was 23 days in the largest published series of pseudoaneurysm observation [4]. Intervention is left for pseudoaneurysms that lead to acute onset of symptoms (pain, groin enlargement), or for the ones greater than 1 cm after a six weak follow up. Considering that critically ill patients often present coagulation defects and thrombocytopenia and warrant daily thromboprophylaxis, as in our case, who presented a sustained decrease in haematocrit (with presence of some schistocytes as a result of haemolysis topically in the sack), a definite aneurysmal treatment is needed. Retroperitoneal haematoma after aneurysmal rupture is another serious complication which may be rather difficult to diagnose in the critically-ill.
Ultrasonography is a valuable tool not only for the diagnosis of pseudoaneurysms but for the treatment as well. Two ultrasound- based approaches have been used: Percutaneous Ultrasonographic Guided Compression Therapy (UGCT), a totally non-invasive technique adopted from the 1990’s, and Ultrasonographic guided thrombin injection (UGTI) [5]. Based upon observational studies and one small randomized trial, ultrasound-guided thrombin injection (UGTI) is indicated as the first-line technique, rather than UGCT [6-8].
However, the data are extrapolated from studies including patients with vascular complications after cardiac and peripheral angiographic procedures. The reported advantages of UGTI were less pain, shorter hospital stays and possibly higher success rates. To our knowledge, there are no studies regarding the natural course and optimal treatment of pseudoaneurysms in ICU patients; hospital stay is not the matter in most of these patients as the length of stay depends on the severity of their illness, as in our case. Moreover, many of these patients are sedated, receiving analgesics, therefore pain is not a first line issue. In addition, although the complications following thrombin injection are reported as infrequent in pseudoaneurysms after angiographic procedures, arterial thrombosis or distal embolization, or even pseudoaneurysm rupture have not been evaluated in ICU patients. Allergic reactions related to bovine thrombin, may be an additional problem in this group of patients receiving multiple drugs.
Finally, UGCT may be the preferred technique depending on the experience of the center and availability of thrombin. Therefore, it seems really appealing in the critical care patients as it is an easy, effective, 24-hour available, bedside treatment modality offering a definite, totally non-invasive therapy.
Acknowledgment
This work has not been supported by any grants.
References
- Wong AVK, Arora N, Olusanya O, Sharif B, Lundin RM, et al. (2018) Insertion rates and complications of central lines in the UK population: A pilot study. J Intensive Care Soc 19(1): 19-25.
- Blanco P, Godoy C, Torre M (2016) Common femoral artery pseudoaneurysm. Intensive Care Med 42(12): 2087-2088.
- Stone P, Campbell J, AbuRahma A (2014) Femoral pseudoaneurysms after percutaneous access. J Vasc Surg 60(5): 1359-1366.
- Toursarkissian B, Allen BT, Petrinec D, Thompson RW, Rubin BG, et al. (1997) Spontaneous closure of selected iatrogenic pseudoaneurysms and arteriovenous fistulae. J Vasc Surg 25(5): 803-808.
- Stolt M, Braun-Dullaeus R, Herold J (2018) Do not underestimate the femoral pseudoaneurysm. Vasa 47(3): 177-185.
- Horn M, Strahlberg E, Goltz JP, Rodd C, Ellebrecht D, et al. (2017) Management of groin pseudoaneurysms; Indications and outcomes for thrombi injection vs. surgical treatment. J Vasc Med Surg 5: 1.
- Lönn L, Olmarker A, Geterud K, Risberg B (2004) Prospective randomized study comparing ultrasound-guided thrombin injection to compression in the treatment of femoral pseudoaneurysms. J Endovasc Ther 11(5): 570-576.
- Khoury M, Rebecca A, Greene K, Rama K, Colaiuta E, et al. (2002) Duplex scanning-guided thrombin injection for the treatment of iatrogenic pseudoaneurysms. J Vasc Surg 35(3): 517-521.

 Case Report
Case Report