Abstract
Background: The objective of this retrospective study was to investigate if introduction of the triceps splitting approach rather than olecranon osteotomy for reduction of intra-articular distal humeral fractures had had an adverse effect on extension strength, clinical scores, union rate, and ulnar nerve affection.
Methods: Eighty-two patients with distal humeral fracture AO/OTA type C were operated with parallel plates between 2003 and 2017. Fifty-one patients, mean age 58 years (18-89), attended follow-up after a mean 41 months (12-115). The approach was a triceps split in 35 and an olecranon osteotomy in 16. The ulnar nerve was in all cases decompressed in situ.
Results: Patients operated with a triceps split had 88% extension strength in the operated compared to the non-operated elbow whereas in the osteotomy group extension strength was 78% (p=0,014). No other differences were found. Among the 82 patients the non-union rate of the humerus was 2% and the olecranon osteotomies 6%. Of the 51 clinically examined 22% had ulnar nerve affection.
Discussion: This demonstrates that type C fractures of the distal humerus can be operated via a triceps split without significant loss of triceps strength, deteriorated function or healing disturbance. Ulnar nerve symptoms and reoperations were common.
Level of Evidence: III, Retrospective Comparative Study, Treatment study.
Keywords: Distal Humerus Fracture; Parallel Plating; Ulnar Nerve; Triceps Split; Olecranon Osteotomy
Abbreviations: MEPS: Mayo Elbow Performance Score; HHD: Hand-Held Dynamometer; ROM: Range of Motion; AVN: Avascular Necrosis
Introduction
Most fractures of the distal humerus need operative treatment with stable internal fixation to restore skeletal anatomy and allow early mobilization, prerequisites for satisfying outcomes [1-4]. Dual plate fixation has been proven most beneficial and the parallel concept biomechanically preferable even though not clearly demonstrated in clinical practice [5-16]. Fracture surgery of the distal humerus requires exposure of the fracture, usually by moving the triceps out of the way at the same time protecting the ulnar nerve, and several different methods have been described [17-20]. The predominating approach, especially for AO/OTA type C fractures, appears to be the olecranon osteotomy, another approach less investigated is the triceps split [21-23]. An olecranon osteotomy provides a wide exposure, particularly of the dorsal two thirds of the distal humerus which is sufficient for most of the intraarticular fractures.
The osteotomy however adds another fracture that needs fixation and is a potential source of non-union and hardware problems, something that has been demonstrated in several publications [22,24,25]. To reduce these problems, we introduced the triceps splitting approach in our department and encouraged its use to all surgeons involved in the management of distal humeral fractures. At the same time, bilateral plate positioning was advocated to improve fixation stability and reduce the problem of non-union. Therefore, the primary purposes of this retrospective study were to investigate if introduction of the triceps split in our department had had adverse effects on the outcomes and if non-union was a problem following internal fixation with parallel plating of distal humeral fractures. To this end we examined if extension power of the elbow was related to the surgical approach and also union rate, clinical outcome and ulnar nerve symptoms following parallel plating of distal humeral fractures type C according to the AO/OTA classification system [26].
Material and Methods
Material
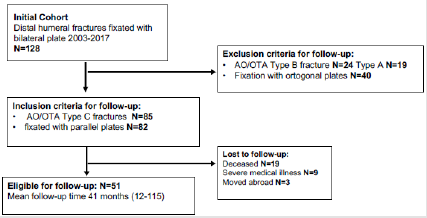
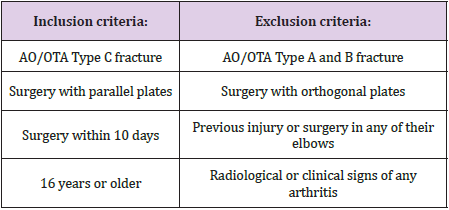
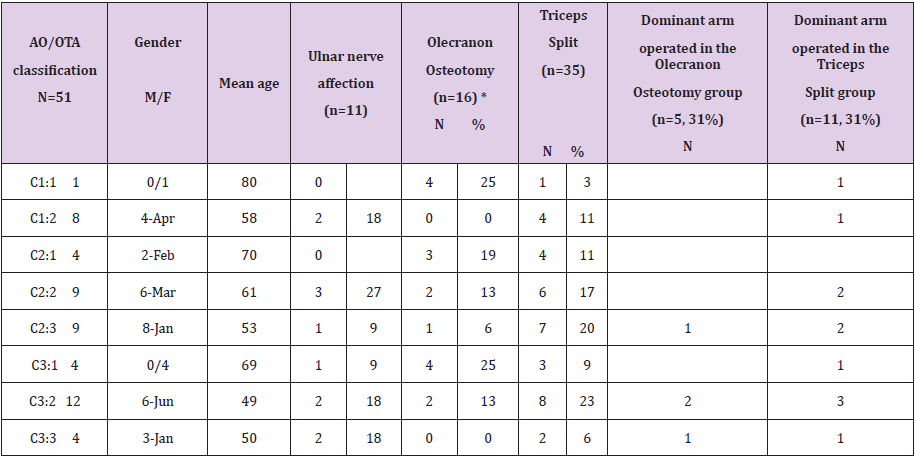
Through the hospitals internal database, 128 adult patients with distal humeral fractures were identified as treated with open reduction, plate and screw fixation between 2003 and 2017. Eighty-five patients were classified as AO/OTA type C and 82 of these had been treated with parallel plates (Figure 1). See (Table I) for inclusion and exclusion criteria. At the time of follow-up 19 patients were dead, 9 severely ill and 3 had moved abroad leaving 51 patients available for follow-up, all of whom were contacted by phone and regular mail and offered an examination. Seventeen men and 34 women with a mean age of 58 years (18-89 years) attended the clinical follow-up and signed informed consent to participate. Two assessors (BS, HBH) reviewed each patient’s medical record. The mean follow-up time was 41 months (12-115). The mechanism of injury included 24 simple falls, 10 bicycle accidents, 8 falls from a height, 7 motor vehicle accidents, 1 skiing and 1 pivot accident. The dominant extremity was involved in 16 of the 51 cases. The ulnar nerve function was, according to the records, preoperatively intact in all. The study was approved by the regional committee for medical ethics (Dnr 2010/171-31).
Surgical Method and Rehabilitation
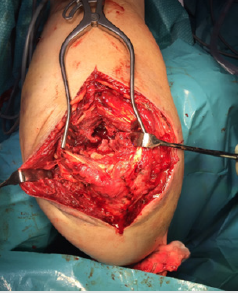
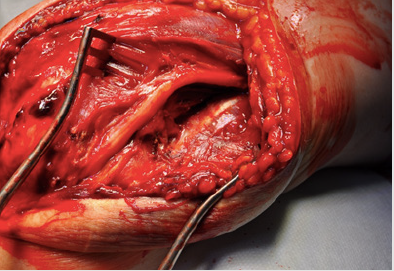
Four experienced surgeons operated all patients with bilateral parallel plates, one on each column, at an angle of approximately 160o between the plates. The fractures were exposed by a posterior skin incision and a mid-line triceps split in 35 patients and an olecranon osteotomy in [16]. Although the recommendation by the department at the time was to use a triceps split whenever possible, the decision of approach was based on the individual surgeons´ previous training, experience and assessment of fracture complexity. When the triceps splitting approach was used for reduction of the intra-articular fracture component the tendon was split in the midline from the tip of the olecranon extending 6-8cm proximally. After splitting the tendon in line with its fibres, the underlying muscle fibres were bluntly separated exposing the capsule and the fat pad in the olecranon fossa. The capsule was released from the olecranon underneath the tendon insertion and the deep soft tissues reflected medially to expose the olecranon fossa and proximal part of the trochlea (Figures 2 & 3).
Figure 2: Triceps tendon split in the midline from the tip of the olecranon extending 6-8 cm proximally.
Figure 3: Olecranon fossa and a distal humeral fracture, Type C, exposed after splitting of the triceps tendon, blunt separation of the underlying muscle fibres, release and reflection of the capsule and fat pad medially.
If a more distal exposure was necessary, the lateral part of the triceps tendon was released from the olecranon in continuity with the anconeus muscle and reflected laterally while carefully protecting the lateral collateral ligament complex. The plates were placed on the respective column by mobilisation of the triceps muscle and release of the medial intermuscular septum (Figure 4). When an olecranon osteotomy had been performed, this was done according to the traditional AO-recommendation with a chevron osteotomy proximal to the base of the coronoid process, through the bare area of the olecranon. In no case was it described that the anconeus muscle had been mobilized in continuity with the triceps. The osteotomies had been repaired with a plate in 6 patients or an intramedullary screw combined with tension band cerclage in 10. In all patients the ulnar nerve had been identified and decompressed (in situ) from the arcade of Struther to the medial ulno-humeral joint line but no anterior transposition was done (Figure 5).
Figure 4: Frontal and lateral projection of one of the distal humeral fractures, Type C, treated with a triceps split and parallel plating, reposition defined as good.
Figure 5: Ulnar nerve decompressed (in situ) from the arcade of Struther to the medial ulno-humeral joint line without transposition.
All patients were immobilised in a posterior plaster splint during 2 to 3 days. Active exercises monitored by a physiotherapist were initiated immediately after removal of the plaster. Light activities of daily living were allowed at all times while load bearing and strengthening exercises begun after 6 weeks. A short period of anti-inflammatory medication was given to prevent heterotrophic ossification.
Clinical Follow-Up
The follow-up included clinical evaluation by two assessors (BS, JN), not involved in the surgical procedures. The scores used were Mayo Elbow Performance Score (MEPS) and Disabilities of Arm, Shoulder and Hand form (DASH) [27]. The ulnar nerve function was assessed according to Dellon´s classification [28]. Isometric elbow extension strength for both sides was assessed with a Hand-Held Dynamometer (HHD) (Chatillon ® MSE100, AMETEK Test & Calibration Instruments 8600 Somerset Drive, Largo, Florida 33773, USA) with the patient supine on a padded table, the shoulder in neutral (adducted), the elbow flexed 90o and the forearm in neutral [21,29,30]. The dynamometer was applied just proximal to the ulnar head [31]. Strength was measured using isometric “make contractions” in which the patient was asked to build his/her force to maximum during 2 seconds and then to push maximally against the plate and the piston of the hand-held dynamometer for 5 seconds. The peak force values were recorded for each trial and the average of three contractions was calculated and values expressed in Newton-meters [31]. Range of Motion (ROM) including arc of flexion-extension and pronation-supination, was recorded with a handheld standard goniometer. The unaffected elbow served as a control for each patient in all of the assessments.
Radiography
Preoperative images, including CT scans, of all 82 patients having been treated with parallel plating, were studied and classified as type C according to the AO /OTA system (Tables 1 & 2). Postoperatively radiographs had been routinely taken and repeated as necessary until union and these were assessed for type of fixation, rate of union, signs of avascular necrosis, reduction, alignment, and heterotopic ossification. Reduction and alignment were defined as good when there was less than 10o of malalignment in any of the lateral or frontal views, step in joint surface less than 3mm and poor when these criteria were not met. Two of the authors (LA, HBH) and a radiologist, not otherwise involved in the study, independently assessed and classified all images. In case of disagreement a consensus discussion was held for final decision. Following classification, the fractures were related to the two different approaches (Table 2).
Table 2: Included patients according to AO/OTA classification.
Note: M= male, F=female, *=including 3 patients with olecranon fracture instead of osteotomy, all plate fixated.
Statistical Analyses
Statistical analyses were made using STATISTICA v.13.2 StatSoft, Inc. Summary measurements were expressed as mean, SD, and range. Student t-test and Mann-Whitney U tests were used to investigate differences between independent groups and between affected and unaffected sides. Correlations were investigated with use of Pearson product-moment correlation coefficients (r). Values of less than 0.25 indicate a weak correlation; between 0.25 and 0.49 mild, between 0.50 and 0.75 moderate, and values greater than 0.75 good correlation [32]. Frequencies were calculated as percentage of patients with available data and for comparison between groups with categorical data, Chi-square test or Fischer’s exact test was used to test the difference in proportions between groups. A p value of 0.05 or less was considered significant.
Results
Score Results
The cohort’s mean MEPS was 83 points (equivalent to “good”), SD 17 (40-100 points); 22 patients (43%) scored excellent; 16 (31%) good; 9 (18%) fair; and 4 patients (8%) poor. The mean MEPS did not correlate with patient age (r= - 0.07, p=0.61), or duration of follow-up (r= 0.06, p=0.66) and there was no significant difference between genders (p=0.95) nor between presence of ulnar nerve affliction or not (p=0.09). If the dominant arm was operated, the MEPS was significantly lower (p=0.03). The mean DASH score was 24 points, SD 21 (0-84 points). A significant difference was found in mean DASH score if the dominant arm was operated (p=0.03) and in case of ulnar symptoms (p=0.01). The DASH score was not related to gender (p=0.4) or time to follow-up (r= 0.11, p=0.44) but there was a mild correlation with mean age at follow-up (r= 0.27, p=0.05).
Strength Testing
Mean isometric extension strength of the injured elbow was 99 Nm, SD 39 (14-196 Nm), equivalent to 85% of the non-operated limb with a mean strength of 116 Nm, SD 41 (49-213Nm) (p=0.06).
Range of Motion
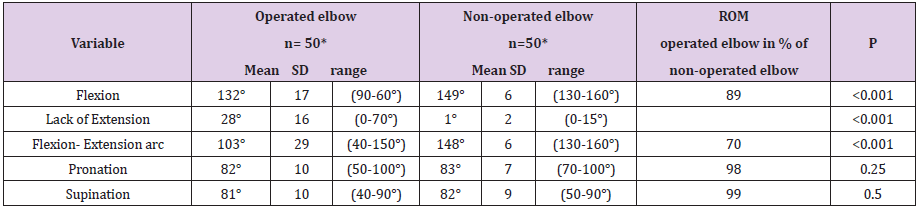
The mean supination and pronation of the injured elbow was almost fully restored, above 98%, and the mean flexion was 89% as compared with the non-operated elbow at follow up. The operated extremity however demonstrated a mean loss of 26°, SD 17 (0-70°) in extension as compared to the non-operated elbow. The total average arc of elbow flexion and extension of the operated arm was 103o, SD 29 (40-150o) equal to 70% of the non-operated elbow (Table 3).
Table 3: ROM measurements of operated and contralateral non-operated elbows.
Note: *One patient is missing all measurements
Nerve Symptoms
Ulnar nerve dysfunction was diagnosed in 11 patients (22%) [28]. Five patients had mild, 4 moderate, and 2 severe affection according to Dellon´s staging. There was no association with reoperation (p=0.13), age (p=0.59), gender (p=0.22) or time to followup (p=0.38). Four patients had had radial nerve palsy in connection with the injury. None of these was surgically explored or repaired and all subsequently recovered without residual symptoms.
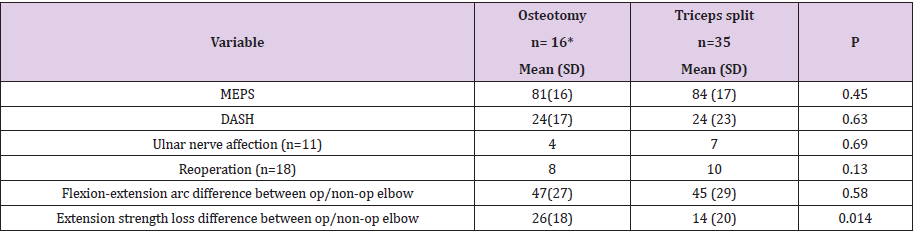
There was no difference in type of fracture, fracture complexity or dominant arm operated between the two groups (Table 2). None of the two surgical approaches; olecranon osteotomy or triceps split, was found superior when related to the functional outcome as assessed with MEPS, DASH or mean range of motion (flexionextension arc). Ulnar nerve symptoms or reoperations were neither associated with any of the two surgical approaches. Patients operated with olecranon osteotomy had 78% extension strength in the operated elbow as compared with the non-operated elbow while the extension strength in the triceps split group was 88% (p=0,014) (Table 4).
Table 4: Comparison between patients treated with olecranon osteotomy or triceps splitting approach.
Note: *3 of 16 patients had a concomitant olecranon fracture instead of an osteotomy used while approaching the distal humeral fracture.
Radiology
Of the 82 included patients, two had developed a pseudoarthrosis of the distal humerus and one of the olecranon osteotomies representing a non-union rate of 2% (2/82) and 6% (1/16) respectively. Two patients had Avascular Necrosis (AVN) and one of them had undergone arthroplasty with a hemiprothesis due to a major collapse of the distal humerus. Sixteen patients had heterotopic ossification and 3 patients had developed posttraumatic arthrosis. The reduction and alignment were good in 79 and poor in 3 patients.
Re-Operations and Complications
Of the 51 patients included in the clinical follow-up 18 (35%) had been re-operated; 11 with implant removal and 4 of these with concomitant ulnar nerve neurolysis. Three had been operated with new osteosynthesis, 2 due to non-union of the distal humeral fracture and 1 because of a non-united olecranon osteotomy. The 2 patients with non-union of the distal humerus fracture had been re-operated with the same parallel plate method, including bone grafting, and had then healed. The patient with olecranon pseudoarthrosis was operated with a new dorsal plate and bone grafting and went on to healing. Three had been operated with resection of heterotopic bone interfering with mobility and one of these with concomitant ulnar neurolysis. Two patients had had a postoperative infection; one of these were re-operated due to the infection.
Discussion
This study demonstrates that AO type C fractures of the distal humerus, can be operated via a triceps split without significant loss of triceps strength, difference in clinical scores, mal-reduction or ulnar nerve symptoms. We found a very high union rate, 98%, with parallel plating. Previous studies have reported a union rate between 87% and 100% [1,15,20,21,33-39]. The functional outcomes were good and the majority of patients (75%) ended up in the categories good or excellent according to the MEPS. These results compare well with other studies on treatment of intraarticular distal humeral fractures [20,21,33-36,39]. On the other hand, reoperations were quite frequent (35%) mostly due to implant removal and local ulnar nerve symptoms. Complications and re-operations seem to be within the array of most studies reporting a range of 21% to 50% reoperations and complications for this kind of fracture [1,4,12,20,34-36,39,40]. Olecranon osteotomy is the surgical approach most often used for plating distal humeral fractures, type C, as it is reported to provide better visualization of the articular part of the distal humerus compared with triceps reflecting and triceps splitting approaches [25].
According to a cadaver study by Wilkinson both osteotomy, triceps reflecting and triceps splitting approaches provided sufficient exposure to the medial and lateral columns to allow plate fixation but none of them allowed visualization of the anterior articular surface of the trochlea or the radial head 25. The downside of using an osteotomy is that the plate may cause skin irritation and the osteotomy may not heal, causing reoperations [22,24,25]. In the present study one osteotomy needed re-osteosynthesis with bone grafting. A previous study comparing olecranon osteotomy and triceps split for type C fractures reported inferior result after the triceps splitting approach. Their study group however included only 7 patients and extension strength was not examined [41]. Our results are however supported by a recent systematic review and meta-analysis, that could not find any differences in functional outcomes or complication rates between Bryan and Morrey or triceps split and olecranon osteotomy approaches [42]. The traditional osteotomy method jeopardizes the innervation to anconeus which may have a negative effect on extension strength and could explain the 10% inferior strength in the osteotomy group in our study. From the records it was however not entirely clear how the anconeus was handled during surgery and the results should be interpreted with some caution due to the uneven groups.
The mean extension strength of 85% in the operated elbow was also to some extent better than some other studies measuring with isometric strength testing of the elbow [35,39,43]. The strength measuring method may influence the result. We used a handheld dynamometer found reliable [44,45]. Altogether our findings support that also intraarticular fractures may be treated with a triceps splitting approach and we suggest that osteotomy may be reserved for the most complex fractures. Ulnar neuropraxia is a common complication associated with elbow fractures [3,17]. In the present study, 22% presented with ulnar nerve symptoms and these patients were often re-operated, even though the majority of symptoms were mild to moderate. The reported prevalence has been between 13-38% in patients treated surgically for distal humerus fractures without transposition of the ulnar nerve and about the same rate in patients with transposition [17,18,34,46- 48]. The reason for the ulnar nerve affection is unclear and may be due to the initial injury, manipulation, scaring and implant irritation [17,19,46,47]. It is previously described that ulnar nerve affection after distal humeral fracture is not infrequent even when no medial plate has been implanted which suggests that nerve affection could mainly be a consequence of the initial injury rather than the surgery [19].
Therefore, we do not believe that more extensive handling of the nerve than in situ decompression would have improved the outcome. The strategy within situ release and protection at surgery has also been supported by other authors [17,20,48,49]. The average DASH score of 24 points in our study reflects that most patients had a relatively good outcome since it is not far from the normative values of the average uninjured Scandinavian population of the same age [50]. We found however, that hand dominance significantly affected the DASH score negatively and the same finding applied to mean MEPS [51]. This finding is relevant when evaluating results after this kind of fracture and surgery. At least 100 o of both elbow flexion, extension and forearm rotation are required to perform most basic activities of daily living [3,52]. Our results of mean flexion- extension arc and mean fore-arm rotation of the operated arm are within the range of the above stipulated functional ROM, and within the results of other studies [4,21,33-36,39,40].
Biomechanical studies have demonstrated that parallel plating is significantly stronger and stiffer than perpendicular plating at least in resisting sagittal bending forces. We found few non-unions, 2 % after the first surgery, and after re-operation with the same method all fractures eventually healed. In summary, based on our experiences and available literature, our primary choice is a triceps split and parallel plating in the majority of type C fractures. Parallel and orthogonal plating should however be considered as complementary methods depending on the fracture appearance and complexity. It must also be emphasized that the method described and used here includes triceps mobilizing to place the plates on the respective column and deal with the extra-articular component of the fracture while the triceps split is used for reduction of the intraarticular part. The split allows visualization of approximately onethird of the posterior and proximal part of the trochlea which is sufficient for less complex fractures but for comminute fractures affecting the most distal and anterior parts, other approaches are often required.
Limitations and Strengths
This study has several limitations. Firstly, being a retrospective study, it cannot be ascertained that patients with markedly different outcomes may not have been lost to follow-up. Secondly the subgroup analyses on surgical approaches were based on uneven groups with fewer osteotomies. There is a risk of selection bias since the choice of surgical approach may have been influenced by the surgeon’s experience and interpretation of the fracture complexity. The readiness to use a new technique may also be due to the level of experience and it cannot be ruled out that the triceps split to a larger extent was adopted by high-volume elbow surgeons which in turn may have had an impact on the quality of reduction and functional outcome. The main strengths are the relatively large sample of 51 patients operated with two standardized surgical techniques and a reasonable follow-up time. Further we used a structured followup with assessment of radiographs, clinical PROMs and objective measurements performed by two independent assessors using the non-operated arm as controls. The methods used support the external validity.
Conclusion
Regardless of triceps split or olecranon osteotomy approach, there was no difference in the outcome measures MEPS, DASH, ulnar nerve compromise or range of motion. However, the extension strength was even significantly better in the triceps split group. Olecranon osteotomy may best be reserved for the most challenging fractures. Parallel plating appears reliable in terms of bone healing and functional outcome. However, ulnar nerve impairment is a common problem after distal humeral fracture surgeries and reoperations relatively frequent.
Declaration of Conflicting Interests
None of the authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Funding
No grants or other funding was received.
References
- Gofton WT, Macdermid JC, Patterson SD (2003) Functional outcome of AO type C distal humeral fractures. The Journal of hand surgery 28(2): 294-308.
- Jupiter JB (1995) Complex fractures of the distal part of the humerus and associated complications. Instructional course lectures 44: 187-198.
- Ring D, Jupiter JB (1999) Complex fractures of the distal humerus and their complications. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 8: 85-97.
- Aslam N, Willett K (2004) Functional outcome following internal fixation of intraarticular fractures of the distal humerus (AO type C). Acta orthopaedica Belgica 70(2): 118-122.
- Self J, Viegas SF, Buford WL (1995) A comparison of double-plate fixation methods for complex distal humerus fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 4: 10-16.
- Helfet DL, Hotchkiss RN (1990) Internal fixation of the distal humerus: a biomechanical comparison of methods. Journal of orthopaedic trauma 4(3): 260-264.
- Schemitsch EH, Tencer AF, Henley MB (1994) Biomechanical evaluation of methods of internal fixation of the distal humerus. Journal of orthopaedic trauma 8(6): 468-475.
- Arnander MW, Reeves A, Mac Leod IA, Thomas Pinto, Arshad Khaleel, et al. (2008) A biomechanical comparison of plate configuration in distal humerus fractures. Journal of orthopaedic trauma 22: 332-336.
- Stoffel K, Cunneen S, Morgan R, Nicholls R, Stachowiak G (2008) Comparative stability of perpendicular versus parallel double-locking plating systems in osteoporotic comminuted distal humerus fractures. Journal of orthopaedic research : official publication of the Orthopaedic Research Society 26(6): 778-784.
- Zalavras CG, Vercillo MT, Jun BJ, Itamura JM, Lee TQ, et al. (2011) Biomechanical evaluation of parallel versus orthogonal plate fixation of intra-articular distal humerus fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 20(1): 12-20.
- Atalar AC, Tunali O, Ersen A (2017) Biomechanical comparison of orthogonal versus parallel double plating systems in intraarticular distal humerus fractures. Acta orthopaedica et traumatologica turcica 51(1): 23-28.
- Shin SJ, Sohn HS, Do NH (2010) A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. Journal of shoulder and elbow surgery/ American Shoulder and Elbow Surgeons 19(1): 2-9.
- Vennettilli M, Athwal GS (2012) Parallel versus orthogonal plating for distal humerus fractures. The Journal of hand surgery 37(4): 819-820.
- Rebuzzi E, Vascellari A, Schiavetti S (2010) The use of parallel pre-contoured plates in the treatment of A and C fractures of the distal humerus. Musculoskeletal surgery 94: 9-16.
- Lee SK, Kim KJ, Park KH (2014) A comparison between orthogonal and parallel plating methods for distal humerus fractures: a prospective randomized trial. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie 24(7): 1123-1131.
- Kumar S, Singh S, Kumar D, Neeraj Kumar, Reetu Verma (2015) Intercondylar humerus fracture- parallel plating and its results. Journal of clinical and diagnostic research : JCDR 9(4): RC01-RC04.
- Shin R, Ring D (2007) The ulnar nerve in elbow trauma. The Journal of bone and joint surgery American volume 89: 1108-1116.
- Vazquez O, Rutgers M, Ring DC, Walsh M, Egol KA (2010) Fate of the ulnar nerve after operative fixation of distal humerus fractures. Journal of orthopaedic trauma 24(7): 395-399.
- Svernlov B, Nestorson J, Adolfsson L (2017) Subjective ulnar nerve dysfunction commonly following open reduction, internal fixation (ORIF) of distal humeral fractures and in situ decompression of the ulnar nerve. Strategies Trauma Limb Reconstr 12(1): 19-25.
- Flinkkila T, Toimela J, Sirnio K, Leppilahti J (2014) Results of parallel plate fixation of comminuted intra-articular distal humeral fractures. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 23(5): 701-707.
- Ali AM, Hassanin EY, El Ganainy AE, Abd Elmola T (2008) Management of intercondylar fractures of the humerus using the extensor mechanism-sparing paratricipital posterior approach. Acta orthopaedica Belgica 74(6): 747-752.
- Ljungquist KL, Beran MC, Awan H (2012) Effects of surgical approach on functional outcomes of open reduction and internal fixation of intra-articular distal humeral fractures: a systematic review. J Shoulder Elbow Surg 21(1): 126-135.
- Chen H, Li D, Zhang J (2017) Comparison of treatments in patients with distal humerus intercondylar fracture: a systematic review and meta-analysis. Ann Med 49(7): 613-625.
- Iwamoto T, Suzuki T, Matsumura N, Matsumoto M, Sato K, et al. (2017) Lateral Para-Olecranon Approach for the Treatment of Distal Humeral Fracture. J Hand Surg Am 42: 344-350.
- Wilkinson JM, Stanley D (2001) Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg 10(4): 380-382.
- Müller M, Koch P, Nazarian S, Schatzker J (1990) The Comprehenisve Classification of Fractures of Long Bones. Berlin: Springer Verlag.
- Longo UG, Franceschi F, Loppini M (2008) Rating systems for evaluation of the elbow. Br Med Bull 87: 131-161.
- Dellon AL (1989) Review of treatment results for ulnar nerve entrapment at the elbow. The Journal of hand surgery 14(4): 688-700.
- Amis AA, Dowson D, Wright V (1980) Elbow joint force predictions for some strenuous isometric actions. J Biomech 13(9): 765-775.
- Askew LJ, An KN, Morrey BF, Chao EY (1987) Isometric elbow strength in normal individuals. Clin Orthop Relat Res 222: 261-266.
- Bohannon RW (1997) Isometric strength data. Arch Phys Med Rehabil 78: 566-567.
- Turchin DC, Beaton DE, Richards RR (1998) Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. The Journal of bone and joint surgery American volume 80(2): 154-162.
- Sanchez Sotelo J, Torchia ME, ODriscoll SW (2007) Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. The Journal of bone and joint surgery American volume 89(5): 961-969.
- Athwal GS, Hoxie SC, Rispoli DM, Steinmann SP (2009) Precontoured parallel plate fixation of AO/OTA type C distal humerus fractures. Journal of orthopaedic trauma 23(8): 575-580.
- Theivendran K, Duggan PJ, Deshmukh SC (2010) Surgical treatment of complex distal humeral fractures: functional outcome after internal fixation using precontoured anatomic plates. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 19(4): 524-532.
- Huang JI, Paczas M, Hoyen HA (2011) Functional outcome after open reduction internal fixation of intra-articular fractures of the distal humerus in the elderly. Journal of orthopaedic trauma 25(5): 259-265.
- Kural C, Ercin E, Erkilinc M, Bilgili MG, Altun S, et al. (2017) Bicolumnar 90-90 plating of AO 13C type fractures. Acta orthopaedica et traumatologica turcica 51(2): 128-132.
- Coles CP, Barei DP, Nork SE, Hanel DP, Bradford Henley M, et al. (2006) The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. Journal of orthopaedic trauma 20(3): 164-171.
- Mc Kee MD, Wilson TL, Winston L (2000) Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. The Journal of bone and joint surgery American volume; 82-A: 1701-1707.
- Kamrani RS, Mehrpour SR, Aghamirsalim MR, Zargar Bashi R, Kaya A, et al. (2012) Pin and plate fixation in complex distal humerus fractures: surgical technique and results. International orthopaedics 36(4): 839-844.
- Pajarinen J, Bjorkenheim JM (2002) Operative treatment of type C intercondylar fractures of the distal humerus: results after a mean follow-up of 2 years in a series of 18 patients. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 11: 48-52.
- Sharma S, John R, Dhillon MS, Kishore K (2018) Surgical approaches for open reduction and internal fixation of intra-articular distal humerus fractures in adults: A systematic review and meta-analysis. Injury 49: 1381-1391.
- Greiner S, Haas NP, Bail HJ (2008) Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Archives of orthopaedic and trauma surgery 128(7): 723-729.
- Stratford PW, Balsor BE (1994) A comparison of make and break tests using a hand-held dynamometer and the Kin-Com. The Journal of orthopaedic and sports physical therapy 19: 28-32.
- Clarke M, Ni Mhuircheartaigh D, Walsh G (2011) Intra-tester and inter-tester reliability of the MicroFET 3 hand-held dynamometer. Phys Ther Ireland 32: 13-18.
- Chen RC, Harris DJ, Leduc S, Ricci WM, Tornetta P (2010) Is ulnar nerve transposition beneficial during open reduction internal fixation of distal humerus fractures? Journal of orthopaedic trauma 24(7): 391-394.
- Worden A, Ilyas AM (2012) Ulnar neuropathy following distal humerus fracture fixation. The Orthopedic clinics of North America 43: 509-514.
- Wiggers JK, Brouwer KM, Helmerhorst GT, Ring D (2012) Predictors of diagnosis of ulnar neuropathy after surgically treated distal humerus fractures. J Hand Surg Am 37(6): 1168-1172.
- Gay A, Liebeskind S, Mehta S (2011) Utility of ulnar nerve transposition associated with distal humerus fracture fixation. University of Pennsylvania Orthopaedic Journal.
- Aasheim T, Finsen V (2014) The DASH and the QuickDASH instruments. Normative values in the general population in Norway. J Hand Surg Eur Vol 39(2): 140-144.
- Kachooei AR, Moradi A, Janssen SJ, Ring D (2015) The influence of dominant limb involvement on DASH and QuickDASH. Hand (NY) 10(3): 512-515.
- Morrey BF, Askew LJ, Chao EY (1981) A biomechanical study of normal functional elbow motion. The Journal of bone and joint surgery American volume 63(6): 872-877.

 Research Article
Research Article