Abstract
Cholangiocarcinoma (CCA)’s qualitative diagnosis and determining the invasion depth is difficult using only imaging modalities. We investigated the relationship between endoscopic images and ex vivo CCA using Magnifying Narrow Band Imaging (M-NBI). Resected specimens of two cases who underwent pancreatoduodenectomy were used. We used an optical magnifying upper gastrointestinal endoscope. In this result, the mucosa of carcinoma was different from non-neoplastic mucosa without inflammation. As a new discovery, endoscopic findings differ in the invasion depth. By being careful about disappeared background vessels using Chol angioscopy, it can be possible to diagnose CCA, especially if it is associated with carcinoma in situ.
Keywords: Cholangiocarcinoma; Magnifying Narrow Band Imaging
Abbreviations: CCA: Cholangiocarcinoma; ERCP: Endoscopic Retrograde Cholangiopancreatography; SOC: Single Operator Chol Angioscopy; M-NBI: Magnifying Narrow Band Imaging; GI: Gastrointestinal; V: Microvascular Architecture; S: Micro Surface Structure; PD: Pancreatoduodenectomy; WLI: white light Images
Introduction
Cholangiocarcinoma (CCA) is the second most common primary hepatobiliary malignancy. Due to nonspecific early symptoms, the great majority of patients are detected at an advanced stage of the disease. Regarding treatment, surgery is better to improve the prognosis of CCA. In the previous study, ductal margin status was a strong independent prognostic factor. However, invasive carcinoma at ductal resection margins appear to have a strong adverse effect on patient survival, whereas residual carcinoma in situ does not [1]. Therefore, the diagnosis of the resection line is important. However, qualitative diagnosis and determining the invasion depth is difficult using only imaging modalities. Therefore, findings and pathological evidence obtained through endoscopic retrograde cholangiopancreatography (ERCP) are important. However, the result of pathological evidence under ERCP was variable accuracy and invasion depth diagnosis using intraductal ultrasonography was difficult [2,3]. Recently, a new device for digital single operator Chol angioscopy (SOC) was introduced to overcome these problems. However, the histological confirmation of SOC-guided biopsies is still relatively low and further improvements in the biopsy protocol are needed [4]. In order to improve endoscopic diagnostic accuracy, it is necessary to understand endoscopic images in further detail. Magnifying Narrow Band Imaging (M-NBI), which is routinely used for Gastrointestinal (GI) cancer, has been reported to be useful for diagnosis [5]. It can obtain clear images of the Microvascular Architecture (V) and the micro surface structure (S). There is a report that ex vivo M-NBI observation of bile duct mucosa. However, qualitative diagnosis is mentioned but determining the invasion depth is not mentioned [6]. Therefore, we investigated the relationship between endoscopic images and invasion depth of ex vivo CCA using M-NBI.
Case Report
Material and Methods
Resected specimens of two cases who underwent Pancreatoduodenectomy (PD) were used. Resected specimens were processed immediately and soaked in saline. All procedures were carried out with an optical magnifying upper GI endoscope (GIF-H260Z; Olympus Medical System, Tokyo, Japan) and a video processor (EVIS LUCERA ELITE CV-290; Olympus Medical System, Tokyo, Japan) under saline. We observed the tissue using white light images (WLI), NBI, and M-NBI. In the NBI mode, the structure enhancement function was constantly set at the A7, with the colour enhancement fixed at mode 3. The observation of the bile duct was performed by board certified fellow of the Japan Gastroenterological Endoscopy Society who engaged M-NBI.
Result
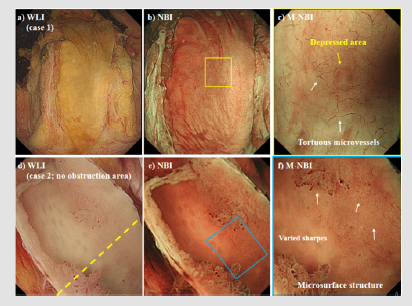
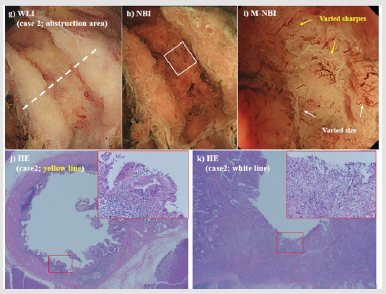
The first case was of pancreatic head cancer without bile duct invasion. The micro vessels were visualized using WLI and NBI (Figures 1a-1b). The micro vessels were clearly visualized using M-NBI. The morphology of V was a fine, regular tortuous micro vessels. In addition, it visualized oval-shaped, depress areas (Figure 1c). S was not clearly visualized using WLI, NBI and M-NBI. The pathological findings showed non-neoplastic mucosa without inflammation. The second case was extrahepatic CCA in the middle to lower part. In this case, the plastic stent (7Fr) was placed for middle bile duct obstruction. In the pathological findings, the lower bile duct was carcinoma in situ (no obstruction area) and the middle bile duct was invasive the serosa (obstruction area). The micro vessels were not visualized using WLI and NBI in the no obstruction area (Figures 1d-1e). However, S was visualized using M-NBI. The morphology of S varied in size and shape (Figure 1f). On the other hand, the micro vessels were visualized using WLI and NBI in the obstruction area (Figure 2g-2h). V and S was visualized using M-NBI. The morphology of V contained many calibre changes and varied sharps, and the density of it was high. The morphology of S also showed varied size and shapes (Figure 2i). The pathological findings of no obstruction area (Figure 2j) and obstruction area (Figure 2k) are shown.
Figure 1: a) First case: white light images (WLI) findings of the bile duct without cancer invasion. b) Narrow band imaging (NBI) findings: the micro vessels were visualized. c) Magnifying endoscopy with NBI findings: the morphology of V was a fine, regular tortuous micro vessels. In addition, it visualized oval-shaped, depress areas. d, e) Second case: WLI findings of the extrahepatic cholangiocarcinoma (CCA) in the lower part (no obstruction area). The micro vessels were not visualized using WLI and NBI. f) M-NBI findings of the CCA mucosa. Microvascular architecture (V): V was not visualized. Micro surface structure (S): the morphology of S varied in size and shape.
Discussion
The use of M-NBI for the bile duct enabled clear visualization of V and S. As a new discovery, endoscopic findings differ in the invasion depth. In carcinoma in situ, the background micro vessels disappeared, and S was irregular. However, in the serosa invasion, both V and S were irregular, and the density was high. The mucosa of carcinoma was clearly different from non-neoplastic mucosa without inflammation. M-NBI may be useful for qualitative and invasion depth diagnosis of CCA. Clinically, there is no Chol angioscopy with M-NBI and the observation of the obstruction area is difficult. However, the no obstruction area is able to observe using Chol angioscopy. The importance of this report is the first report of the invasion depth of ex vivo CCA using M-NBI images. In addition, it may contribute to the endoscopic diagnosis of carcinoma in situ. By being careful about disappeared background vessels using Chol angioscopy, it can be possible to diagnose CCA, especially if it is associated with carcinoma in situ. The combination of pathological evidence and endoscopic images are possible to diagnose carcinoma in situ, increasing the number of operable cases and improving the prognosis. Monitoring using M-NBI may be an appropriate way to improve the qualitative diagnosis of CCA and to determine its invasion depth.
Figure 2: g, h) Second case: white light images (WLI) findings of the extrahepatic cholangiocarcinoma (CCA) in the middle part (obstruction area). The micro vessels were visualized using WLI and Narrow band imaging (NBI). i) Magnifying endoscopy with NBI findings of the CCA mucosa. Microvascular architecture (V): the morphology of V contained many calibre changes and varied sharps. Micro surface structure (S): the morphology of S showed varied size and shapes. j) Pathological image of the yellow line in Figure 1d). In the pathological findings, the lower bile duct was carcinoma in situ. k) Pathological image of the white line in Figure 2g). In the pathological findings, the middle bile duct was invasive the serosa.
Acknowledgment
None.
Conflicts of Interest
Authors declare no conflict of interest for this article.
References
- Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K (2005) Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer 103(6): 1210-1216.
- Mansfield JC, Griffin SM, Wadehra V, Matthewson K (1997) A prospective evaluation of cytology from biliary strictures. Gut 40(5): 671-677.
- Domagk D, Poremba C, Dietl KH, Senninger N, Heinecke A, et al. (2002) Endoscopic transpapillary biopsies and intraductal ultrasonography in the diagnostics of the bile duct strictures: a prospective study. Gut 51(2): 240-244.
- Karagyozov P, Boeva I, Tishkov I (2019) Role of digital single operator cholangioscopy in the diagnosis and treatment of biliary disorders. World J Gastrointest Endosc 11(1): 31-40.
- Yao K (2015) Clinical application of Magnifying Endoscopy with Narrow-Band Imaging in the Stomach. Clin Endosc 48(6): 481-490.
- Ishida Y, Okabe Y, Yasumoto M, Naito Y, Nakama Y, et al. (2018) Ex vivo magnifying endoscopic observation of bile duct mucosa using narrowband imaging. J Hepatobiliary Pancreat Sci 25(10): 433-439.

 Case Report
Case Report