Abstract
Introduction: Obstructive sleep apnea (OSA), a pathology increasingly prevalent, is a complex treatable syndrome that impact morbidity and mortality with serious cardiovascular and metabolic consequences. The interest for this pathology has increased in last decades although the syndrome remains underdiagnosed. Therefore, we aimed to identify the main predictive factors and to assess the interrelationship between them and OSA severity.
Methods: To this end, we performed a prospective study in a Romanian population. The study occurred for 48 months, between October 2015-september 2019, in the Sleep Disorders Center from County Emergency Clinical Hospital of Constanta. Polygraphy, blood tests, anthropometric parameters, demographic aspects were recorded for each subject. Predictive factors were disclosed using multivariate regression analysis.
Results:198 patients who referred to the Sleep Disorders Center and had been evaluated for OSA were enrolled. The study population included 147 male and 51 female; age range 27-82 years old. Among the 198 individuals, 43.5% (86 patients) had moderate OSA and 56.5% (112 patients) had severe OSA. Neck circumference, waist-hip ratio, BMI, gender, age was found to be significant predictors for OSA. In addition, >50% of patients had metabolic alterations or had cardiovascular disorders.
Conclusion: No single factor was usefully predictive. Patients with OSA were more likely to be male, older, obese, have a thick neck, have a significant greater prevalence of habitual snoring and excessive daytime sleepiness, have hypertension or metabolic changes.
Keywords: Predictive Factors; Obstructive Sleep Apnea; Anthropometric Variables
Introduction
Sleep medicine is a field in continuous development, sleep disorders breathing representing a structure that comprises a variety of respiratory disturbances that occur during sleep [1,2]. Obstructive sleep apnea syndrome (OSA) is the most frequent sleep breathing disorder with an increasing prevalence in last decades, but largely underdiagnosed and undertreated. It is characterized by recurrent episodes of obstruction of upper airways leading to sleep fragmentation and intermittent hypoxia during sleep. On one hand, OSA is a complex entity that has serious cardio-metabolic complications[1,2] with a severe impact on the patient’s quality of life and requires multidisciplinary approach , on the other hand, it is a treatable pathology with an important influence on morbidity and mortality [3].
In Romania, this syndrome is still insufficiently well-known and studied with a variable prevalence in adult population due to differences in defining and diagnostic methods. However, the increasing number of sleep centers and the increasing number of patients who undergo a sleep study are raising awareness of this pathology but diagnostic test for suspected patients are limited due to cost and availability. Therefore, it is important to have a wellfounded approach to recognize patients with a high probability of being diagnosed with OSA. We hypothesis that identifying the main predictors for OSA will lead to the development of prediction formula that will help prioritizing patients to sleep study and treatment by the probability of severity of the disease.
Aim
We performed a prospective study in patients that were
evaluated for OSA in the Sleep Disorders Center from County
Emergency Clinical Hospital of Constanta, between October 2015 -
September 2019. Patient group consisted in subjects who referred
to our Sleep Laboratory for evaluation of OSA or subjects that
were referred by otolaryngologists with a high suspicion of sleep
pathology. 257 consecutive individuals were investigated and each
patient has signed the informed consent. All patients completed
the study chart (which included general information like age, sex,
occupation, use of alcohol, smoking and self-reported symptoms
like snoring, stopping breathing, sleepiness), sleep questionnaire
(Epworth Sleepiness Scale) and had a clinical evaluation with
measurement of anthropometric variables like weight, height,
BMI, neck circumference, waist circumference, waist-hip
ratio. Furthermore, several biological markers were evaluated
(glucose, cholesterol profile), blood pressure was measured and
otorhinolaryngology examination (with fibroscopy of the nasal
and pharyngeal cavity and Mallampati score assessment) was
performed for everyone.
Patient’s medical records were used to document comorbidities
(cardiovascular, metabolic, respiratory) or chronic treatments. In
addition, the presence of metabolic syndrome was evaluated using
the National Heart, Lung, and Blood Institute (NHLBI) and the
American Heart Association (AHA) guidelines. Metabolic syndrome
was diagnosed if the patients met 3 out of the 5 criteria:
a. abdominal obesity (waist circumference ≥94cm in men or
≥80cm in women),
b. a low level of highdensity lipoprotein cholesterol (<40mg/
dl in men or <50mg/dl in women) or receiving lipid-lowering
drug therapy,
c. elevated triglyceride level (≥150mg/dl) or receiving drug
therapy for hypertriglyceridemia,
d. elevated blood pressure (systolic ≥130mmHg or diastolic
>85mmHg) or receiving drug therapy for hypertension,
e. fasting plasma glucose level (≥100mg/dl) or receiving
drug therapy for hyperglycemia. Overnight respiratory
polygraphy study was conducted in each case and every record
was validated manually.
The following parameters were obtained: nasal airflow was
registered trough a cannula, thoracic and abdominal movements
were registered by using plethysmography belts, oxygen saturation
and heart rate were measured by a finger probe oximeter, body
position and number of snoring events were assessed by using
sensors situated on the chest.
According to American Academy of Sleep Medicine definition,
apnea was scored when the airflow signal drop by 80% or greater
with continuing respiratory effort with a duration of 10 seconds or
more. Hypopnea was scored when the peak signal excursions drop
by ≥30% of pre-event baseline using nasal pressure more than 10
seconds associated with a ≥ 4% oxygen desaturation from pre-event
baseline. Apnea-hypopnea index (AHI) consisted in the number
of apneas and hypopneas per hour of total sleep time. OSA was
graded using apnea-hypopnea index as follows: mild (AHI 5 - 15
events/h), moderate (AHI 15 - 30 events/h) and severe (AHI ≥ 30
events/h). For patients with AHI < 5 events/h OSA was ruled out.
In addition, in our study, patients with mild OSA (AHI between 5
and 15 events/h) were excluded since polysomnography was not
available in these cases for a definite diagnosis.
Patients that were eligible met the following inclusion criteria:
a) Age ≥ 18 years old
b) No previous diagnosis of OSA
c) AHI ≥ 15 events/hour
d) No secondary cause of hypertension
e) No family dyslipidemia
f) No type 1 diabetes
g) Informed consent was signed
Statistical data were processed using IBM SPSS version 2.0 and
Microsoft Excel. Qualitative data were characterized by frequency
and percentage whilst quantitative variables were described
using the mean and standard deviation. P value was considered
statistically significant at 0.05 or less.
Result
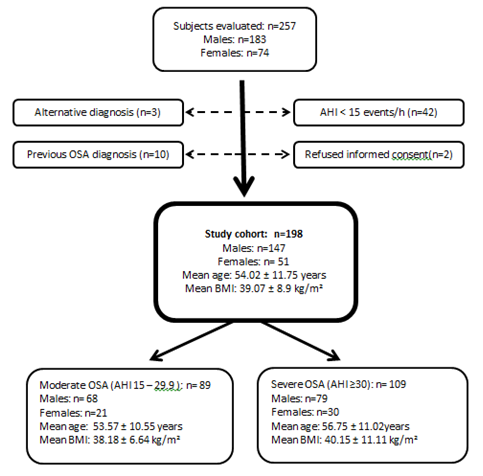
The study flow diagram is presented in Figure 1. From the total number of patients investigated in the Sleep Laboratory the study cohort counted 198 patients. The subjects who did not met the inclusion criteria wereexcluded. The 198 subjects enrolled included 141 (71.2%) men and 57 (28.7%) women, with a male-to-female ratio of 2.4:1. The mean age in the study group was 54.09 years. The youngest patient was 25 years old and the oldest patient was of 82 years old. A significantly increased prevalence of OSA was shown, in our study, in persons older than 40 years compared with individuals aged 20-40 years.The study group comprises 89(44.9%) individual with moderate OSA and 109 (55.1%) individuals with severe OSA. The mean AHI was 35.4±21.1 events/h in women and 39.1±24.3 events/h in men. Mean oxygen desaturation index was 40.3±19.7 for men and 36.7±18.2 for women. No significant correlation was found between gender and AHI severity.
Figure 1: Demographic aspects of the study group (Abbreviations: OSA – obstructive sleep apnea, AHI – apnea-hypopnea index, BMI – body mass index).
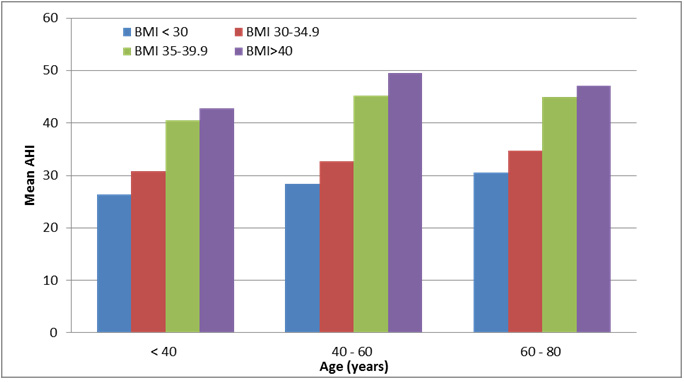
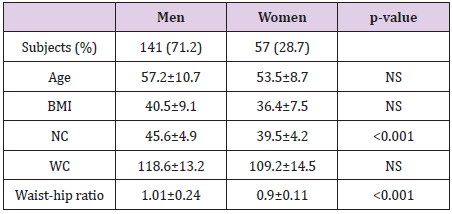
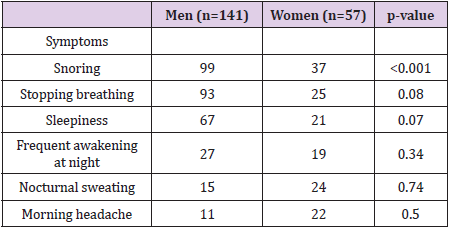
In terms of demographic characteristic, another specific marker assessed was BMI. (Figure 2). The study has shown that most patients (84.8 %), regardless of gender, had a degree of obesity and only 13.1 % were overweight. There was a small proportion (2.02%) of patients who had normal BMI. However, BMI is not sufficient to evaluate the wide variation in body fat distribution, thus, additional measurements were made. Neck and waist circumference, waist-hip ratio was assessed for all subjects. In our cohort, the mean neck circumference was 45.6±4.9cm in men and 39.5±4.2cm in women. Regarding waist circumference the mean values were 109.2±14.5cm for women and 118.6cm±13.2 for men. Waist-hip ratio cut-off values used were >0.9 in men and >0.85 for women. WHR measurements showed a mean value of 1.01±0.24 in male subjects and 0.9±0.11 in female subjects. (Table 1) OSA has multiple ways of presenting, therefore, each patient enrolled in the study has reported several symptoms. We considered the following complaints that were related more frequently: snoring (68.6%), stopping breathing (59.5%), sleepiness (44.4%), frequent awakening at night (23.2%), nocturnal sweating (19.6%) and morning headache (16.6%).A significant association was revealed between snoring and AHI severity.
Figure 2: Correlation between mean AHI, BMI, age in the study group (Abbreviations: AHI – apnea hypopnea index, BMI – body mass index).
Table 1: Characteristics of the group; Data are presented as mean±SD; Bold p value is statistical significant (Abbreviations: OSA – obstructive sleep apnea, , BMI – body mass index, NC – neck circumference, WC – waist circumference, WHR – waist-tohip ratio, NS refers to not significant p value).
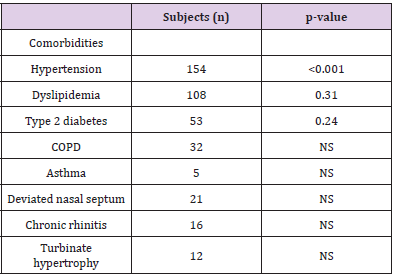
(Table 2) More than 50% of enrolled patients had not reported excessive daytime sleepiness. Consequently, for an objective evaluation, Epworth Sleepiness Scale questionnaire was used for every patient. ESS was interpreted as follows: 0-5 points lower/ normal daytime sleepiness, 6-10 points higher normal daytime sleepiness, 11-12 points mild excessive daytime sleepiness, 13-15 points moderate excessive daytime sleepiness, 16-24 points severe excessive daytime sleepiness. The mean value of ESS score in our cohort was 9.4±4.3 points. A significant correlation was found between high ESS score (>13 points) and AHI severity. Several comorbidities are very frequently associated in patients with OSA. In our study population, most common associated diseases found were: Hypertension (78%), Dyslipidemia (55%), Metabolic syndrome (58%), Type 2 diabetes (27%), COPD/Asthma (19%), ENT disorders (18%) (Table 3).
Table 3: Comorbidities distribution in the study population; Bold p value is statistically significant (Abbreviations: NS refers to not significant p value)
Discussion
Obstructive sleep apnea is a pathology that has a plurifactorial
etiology. In our study, one objective was to identify the
main predictors of OSA and correlate them with the severity of the
syndrome. Firstly, the research highlighted that there is an increased
incidence of OSA among male subjects. About two-thirds of enrolled
patients were men, resulting a 2.4/1 male-to-female ratio. These
observations are consistent with the literature, several studies had
previously reported a male predominance in patients with OSA.
Despite this finding, in the studied group, no correlation was found
between sex and OSA severity, meaning that both women and men
can have moderate or severe disease, regardless of gender. Another
factor that had been considered is age. In our studied population,
we have found that 76.76% of patients diagnosed with moderate
or severe OSA were aged 40 years or older, with an increased
prevalence as ageing. A peak had been emphasized for both women
and men in the fifth and sixth decade of life. These findings are
consistent with those reported in the literature, Malhotra et al. [4]
explaining it through the age dependent changes that arise in the
soft palate and pharynx.
Obesity is a major risk factor for OSA. In our study, most of
patients were overweight or had different degrees of obesity.
Evaluation of obesity included: BMI, NC, WC, WHR. The analysis of
these metrics of obesity showed that the best unvaried predictor
of AHI severity for each gender was waist-hip ratio, independently
of BMI. In addition, for male subjects, a significant correlation
between neck circumference and OSA severity was disclosed. In
terms of symptoms, snoring was the most common manifestation
reported for which patients were evaluated for a sleep disorder.
Daytime sleepiness was assessed by using Epworth Sleepiness
Scale questionnaire. Although the study comprises individuals with
moderate and severe OSA, more than 50% of the patients did not
report excessive daytime sleepiness and we concluded that, most
frequently, sleepiness was underestimated. A significant correlation
was found between snoring, BMI and moderate to severe ESS
scores, but a singular predictor is only marginally useful.
Several studies had demonstrated the cardiovascular and
metabolic implications of obstructive sleep apnea disclosing
that the link between OSA and comorbidities can have serious
consequences. In our cohort, most frequent newly diagnosed
or pre-existent cardio-metabolic disorders were hypertension,
metabolic syndrome, dyslipidemia and type 2 diabetes, out of which
hypertension and MS have a strong correlation with AHI severity.
Thus, the association needs to emphasize the role of OSA screening
in patients with metabolic changes, hypertension and vice versa,
considering that treating the sleep disorder has a positive impact
on general outcome. In our study population, other comorbidities
like COPD, Asthma and ENT pathologies were evaluated but no
correlation with AHI severity was found. However, it is important
to mention that ENT disorders can interfere with the treatment of
OSA or can have a role in syndrome’s physiopathology,therefore is
mandatory to assess and treat these conditions.
Conclusion
OSA is a multifaceted disease with severe cardiovascular and metabolic repercussions which needs to be better understood and early diagnosed. Early identification of atrisk patients is still challenging, therefore recognizing these predictive factors and patterns should acknowledge the need of OSA screening prioritizing the access to sleep study (polygraphy / polysomnogram) for specific patients group.
The syndrome is a treatable condition therefore promptly recognition will not only improve the quality of life by its therapy, but also the life expectancy by meliorating the severity of the associated diseases.
Acknowledgements
The authors have no acknowledgements.
Conflict of Interest
No conflict of interest is to declare.
References
- Ferran Barbé, Jean-Louis Pépin(2015) Obstructive Sleep Apnoea, Edited by Book, ISBN 978-1-84984-060-6.
- Anita K Simonds, Wilfried de Backer (2012) ERS Handbook of Respiratory Sleep Medicine, European Respiratory Society, ISBN978-1-84984-024-8.
- Meir Kryger, Thomas Roth, William C Dement, (2017) Principles and Practice of Sleep Medicine, 6th(Edn), Elsevier, ISBN 978-0-323-24288-2.
- Ohad Ronen, Atul Malhotra, Giora Pillar (2007) Influence of Gender and Age on Upper-Airway Length During Development, Pediatrics 120(4): e1028-e1034.

 Research Article
Research Article