Abstract
A 28-year-old female positive for COVID-19 gave birth to a full-term fetus. The baby girl was negative for COVID-19. Microscopic examination of placenta showed proximal stem villi vasculitis as a possible placenta reaction to viral infection.
Case Report
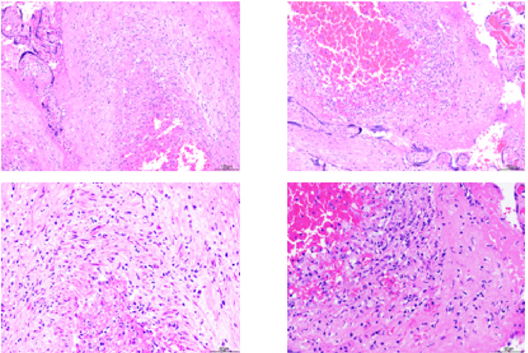
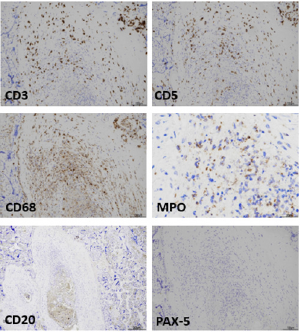
A 28-year-old female (Gravida 2, Para 1) who was 40 weeks pregnant was admitted to hospital with vaginal bleeding and uterine contractures. Tests for hepatitis B and group B streptococci were negative. Her peripheral blood showed mild thrombocytopenia (116 x 10^9/L, Range: 150-400 x10^9) but no lymphocytopenia. The nasopharyngeal swab sent for corona virus RT-PCR test confirmed COVID-19 infection. However, she had no upper respiratory symptom. The induction with amniotomy and oxytocin resulted in spontaneous vaginal delivery of a live baby girl (Apgar score 9 at 1 and 5 minutes) weighs 3463 grams with no morphological abnormality. The nasopharyngeal swab sent for corona virus RT-PCR test on day 1 and 3 after birth were negative for COVID-19. The macroscopic examination of placenta showed 466 grams term placenta (25-35 percentile for age) with attached cords and membranes. Microscopic examination shows multiple foci of proximal stem villi vasculitis (Figure 1). The immunohistochemistry showed that the vascular walls are invaded mainly by T-cells (CD3 and CD5 positive) and histiocytes (CD68 positive) and scattered neutrophils (myeloperoxidase positive). Although there were B-cells (CD20 and PAX-5 positive) identified in the fetal blood vessels, there was no B-cell among inflammatory cells invading the vascular walls (Figure 2). There was no evidence of chorioamnionitis or inflammation of cord.
Figure 1: Two examples of proximal stem villi vasculitis. The top row shows two separate foci and the bottom row is the higher power of the top row images.
Figure 2: Immunohistochemistry identifies T-cells (CD3 and CD5 left and right top row), histiocytes (CD68 left middle row) and neutrophils (MPO right middle row). Although the B cells are seen in the fetal blood circulation (CD20 left bottom row), there is non in the vasculitis focus (CD20 and PAX-5 left and right bottom row).
Discussion
There are two main studies of placenta pathology in COVID-19 pregnancies [1,2]. Maternal and fetal vascular anomalies and injuries have been shown in both studies. However, to our best knowledge, the proximal stem villi vasculitis has not been reported yet. This finding needs to be investigated in more COVID-19 pregnancies.
References
- Rebecca N Baergen, Debra S Heller (2020) Placental Pathology in Covid-19 Positive Mothers: Preliminary Findings. Pediatr Dev Pathol 23(3): 177-180.
- Elisheva D Shanes, Leena B Mithal, Sebastian Otero, Hooman A Azad, Emily S Miller, et al. Placental Pathology in COVID-19. Am J Clin Pathol 154(1): 23-32.

 Case Report
Case Report