Introduction
Prostate cancer (PCa) remains the second cause of cancer death in men, it is a public health problem especially in elderly patients with 35.5% cases diagnosed after 75 years. it is rare before the age of 60 with 9%. The risk factors for PCa are the age melanoderm ethnicity and a family history of PCa, in which case they occur five to ten years earlier than in the general population [1,2]. The heterogeneity of its genetic an environmental factor, make this cancer an uncertain prognosis and its real incidence in young men is difficult to assess because most men of this age do not have screening, and varies according to countries, ethnicity and age [1-4]. The Screening of Pca is based on digital rectal examination (DRE) and rate of the prostate specific antigen (PSA) [5-7]. Since the use of PSA as a test for Pca, more and more young men are diagnosed in the early stages of the disease [5,6]. Few published data regarding PCa in young men have reported conflicting results. Some have suggested that PCa in young men has a better prognosis than that in older men, while others have reported an unfavorable prognosis [7,8].
Radical prostatectomy (RP) remains the standard treatment for localized PCa, reducing mortality by 10 to 15% at 10 years, through its efficacy in terms of cancer control and increased overall survival [9-11]. Through the study 20 cases of localized PCa in patients under 60 years treated by RP carried out in the urology department of the military teaching hospital of Rabat and a review of the different published series, we propose to analyze the particularities of this cancer in this age group.
Materials and Methods
This is a retrospective study including all patients treated for localized PCa by RP and whose age is less than 60 years at the Mohamed V Military teaching Hospital in Rabat between January 2004 and October 2014.To analyze the particularities of localized PCa in patients aged less than 60 years, we were interested in the following parameters: age, diagnostic circumstances, PSA level, extension assessment, TNM stage, preoperative and postoperative clinical and pathological evaluation. The data were collected by an exhaustive search in the medical files, radiological, operative and anatomopathological reports available in the archives of the urology department of mohamed V military teaching hospital. The statistical analyzes were carried out using software Microsoft Office Excel.
Results
Clinical Results
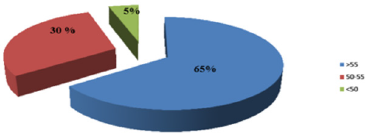
Age: The average age at the time of diagnosis was 55.5 years, with extremes of age 47 years and 59 years. The age groups are distributed as follows: 65% between 50 and 55 years old, and 5% are 50 years old (Figure 1).
A. Reasons for Consultation: most often they are voiding disorders such as dysuria and pollakiuria, found in 70% of cases and 30% of patients have been asymptomatic (Figure 2).
Digital Rectal Examination (DRE)
The DRE was considered normal by the urologist in 80% of the cases, and 4 patients presented with induration or a palpable prostate nodule with the DRE (Figure 3). The results of the paraclinical examinations for diagnostic purposes:
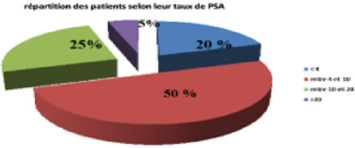
The Prostate Specific Antigen (PSA): The mean PSA level was 9.8 ng / ml (1.26-44.34 ng / ml. The prevalence of CaP located in the PSA section <10 ng / ml was 20%. 70% of patients treated with PRP had PSA <10, however the rest of the patients (30%) had PSA> 10 ng / ml, including 1 with PSA> 20ng / ml (Figure 4).
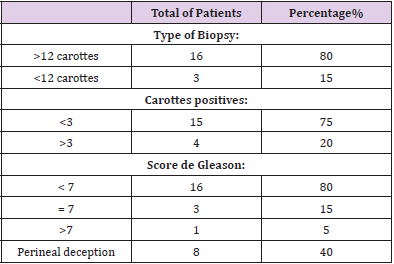
Analysis of the prostate biopsy data (Table 1) reveals that the majority of localized CaPs diagnosed in this series:
a. 80%, by an extensive biopsy (12> carrots).
b. The number of positive carrots per patient was <3
c. in 75% of cases and> 3 in 4 patients
while the diagnosis in 1 patient was obtained on the histological data of the TURP. adenocarcinoma was found in all patients. The biopsy Gleason score was <7 in 80% of cases, equal to 7 in 15% of cases and> 7 in 5% of cases. The percentage of invasion of positive biopsies was also evaluated, it varied between 0 to 80%, with an average of 41.25%.Peri-nervous sheathing was found in 40% of the cases (Table 1).
The Results of the Extension Assessment
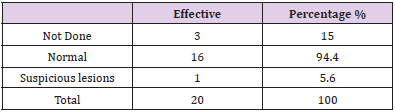
Magnetic Resonance Imaging: Carried out in 14 patients (70%), most of the patients had a tumor. limited to the organ without lymph node extension. The extra capsular extension was noted in one patient (5%).
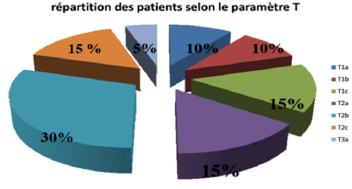
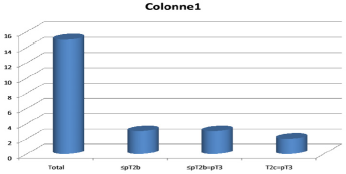
Bone Scintigraphy: There was suspicion of a secondary lesion in one patient and CT scan with a bone window helped to correct the diagnosis and rule out the metastatic nature of this lesion, which was in fact arthritis (Table 2). After the extension assessment, the most frequent stage was the T2b stage present in 30% of the patients, followed by the T1c, T2a and T2c stages present in 15% of the patients for each, the T1a and T1b stages present in two patients, then stage T3a present in a single patient which represents 5% of the sample studied. All patients were classified as N0.
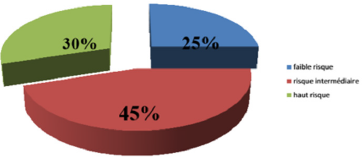
According to D’Amico criteria, the CaP located in our series was located in a low-risk group (≤T2a and G≤6 and PSA <10) in 25% of cases, at intermediate risk (T2b or G = 7 or 10 < PSA ≤20) in 45% of cases, and at high risk (T2c or G> 7 or PSA> 20) in 30% of cases (Figure 5 & 6).
Therapeutic Choice
Radical Prostatectomy: the standard treatment of localized PCa in patients with a life expectancy greater than 10 years. Classically reserved for organ-confined tumors, RP can also be considered for tumors with limited extra-capsular extension (clinical T3a, biopsy or MRI), partly young patients. In our series, all patients underwent radical public prostatectomy with lymph node dissection and preservation of the two neurovascular bundels in 15 cases, right unilateral in 3 cases, left unilateral in 2 cases.
Pathology Results of the Operating Specimen
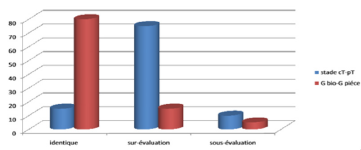
The correlation between the clinical data (stage cT and GS) and those of the pathological study prostate specimen was identical in 15% of the cases for the stages cT –pT and 80% of the cases for the Gleason scores (SGb SGp) (Figure 7). upstaging of the Gleason stage and / or grade to a higher level was observed in 75% and 15% of the cases, respectively. Downward migration of the Gleason stage or grade was observed in 10 % and 5% of cases respectively. When we analyze more closely the cases of upgrading from the clinical stage to the (15 patients) (Figure 8) We find that the progression of the stage occurred in the same group of low risk (≤Pt2b). However, in the rest of the cases (80%), we only moved to a high-risk group (≥ pT2c). Upgrading from an organ-confined stage (≤cT2c) to a locally advanced stage (pT3a-b) was observed in 5 patients.
‘A downgrading of the clinical stage on the PRR part was observed in two patients, the two patients initially evaluated cT2c, were pT2a. Regarding the upgrading of the biopsy Gleason score and grade on prostate surgical specimen (3 patients): only 1 patient had a significant prognostic migration of the Gleason score (SGp≥7). In the rest of the cases, the migration of the Gleason grade was done in the same prognosis group, not eliminating the advantage of performing a RP.
Adjuvant Therapy
The rate of positive surgical margins in our series was 25%. In the 5 patients, the surgical margins were focal and very limited (R1), The status of surgical margins is one of the major factors of biological recurrence which determines whether or not an adjuvant treatment is necessary after surgery. The attitude in our service is to monitor patients (PSA) and treat only in the event of a biological recurrence (PSA> 0.2 ng / ml confirmed at two successive dosages). In our series 2 patients had benefited from external radiotherapy Combined with short-term hormone therapy, and one patient received hormone therapy alone.
Post-Operative Monitoring and Evaluation
Marked by a Biological and Clinical Evaluation: On the biological level, the PSA dosage made it possible to judge the oncologic results at a distance from the intervention and found at 1 month three patients had a PSA> 0.2 ng / ml, at 3 months only one patient had a PSA equal to 0.2 ng/ ml, at 6 months the PSA was undetectable and at 12 months a patient 1 patient had increased his PSA. On the clinical level, the postoperative evaluation in the 9 patients still followed at the time of this work, had shown 1 case of absence of erection: 1 case of urinary incontinence, 1 case of nocturia.
Discussion
Prostate cancer is a real public health problem by its frequency, with great variability in incidence and mortality worldwide. The incidence of prostate cancer varies by more than 25 times worldwide, and according to GLOBOCAN 2012, Morocco has been classified in the zone where the incidence varies between 10.8 and 19.5 / 100,000 [12,13]. Some studies preceding the era of PSA use have estimated the incidence of CaP in young men to be between 0.8 and 4%. The actual incidence of young subjects is difficult to assess in the general population, since most men of this age do not have screening. Mortality rates are generally high in the predominantly black populations, According to GLOBOCAN 2012 Morocco has been classified in the area where mortality varies between 10 and 13.9 / 100,000. In our series, the average age at diagnosis was 55.5 years, with extremes of 47 and 59 years of age [14,15]. The age groups are distributed as follows: 65% of patients are over 55 years of age, 30% between 50 and 55 years of age, and 5% are under 50 years of age.
The circumstances of discovery are often during a screening by PSA or following the appearance of urinary disorders, 70% of our patients were already symptomatic and screening was done following urinary disorders of the lower urinary tract. The discovery of cancer was fortuitous during an individual screening in 30 % of our patients, this rate does not exceed 6% in the study by Amégbor, et al. and Reached 15% in the study by Filella, et al. and 18% in the study by BALLA, et al. (HMIV in 2009). The TR has a positive predictive value estimated between 21% and 53%, In our series the TR was considered normal by the urologist in 80% of the cases and that 4 patients presented a induration or a palpable prostate nodule at the TR. Active surveillance as a therapeutic option is reserved for requesting patients who have a localized tumor with a very good prognosis.
Active surveillance leads to the identification of the most aggressive forms, to delaying treatment for a few years and thereby delaying the date of onset of urinary and sexual complications from treatment. However, active surveillance has not yet been validated as an alternative to immediate treatment in young men [16,17]. Total prostatectomy is one of the benchmark treatments for CaP localized in patients whose life expectancy, estimated by age and associated poly-pathologies, is greater than or equal to 10 years [18-20]. External radiotherapy is a validated alternative to total prostatectomy, with similar carcinological results in the medium term [22-27]. In young men, few studies are available concerning external radiotherapy for CaP [22-25]. Rosser, et al. [24] compared the results of external radiotherapy in 98 patients under the age of 60 and 866 older patients in one study and this concluded that young age thus appears to be a factor in poor prognosis [22-24].
Brachytherapy is an alternative to total prostatectomy for tumors with a low risk of progression, its carcinological results at 12 years are similar to those of total prostatectomy. Few data have been published regarding prostate cancer (CaP) in young men. In addition, the few studies that have analyzed the prognosis of CaP in this population have resulted in conflicting results [28].
Carcinological Results
In 1995, an American study analyzed the impact of age on survival without biological recurrence after total prostatectomy [29]. The rate of biological recurrence was significantly lower in young patients than in older patients. The study by Magheli et al. [30], including very young patients 435 patients aged 45 or less were compared to three other age groups 70: 46–55 years, 56–65 years and above or equal to 66 years. The number of patients has made it possible to conclude that the impact of age on the cancer outcome of patients remains uncertain, due to the lack of large prospective controlled studies. Total prostatectomy seems to have at least equivalent results in terms of effectiveness in young patients compared to an older population.
Functional Results
Age in itself represents, outside of any surgical context, a predictor of incontinence by sphincter insufficiency and a predictor of erectile dysfunction by vascular obstruction. This remains true after total prostatectomy. An American team retrospectively compared the results of total prostatectomy in 66 young patients and 724 older patients. Surgical complications and rates of biological recurrence were similar between the two groups. Among patients who had bilateral vasculo-nervous preservation, 100% of young patients versus 81.4% of older patients had satisfactory postoperative erections without or with treatment (phosphodiesterase-5 inhibitor or cavernous injections). Even if the rare retrospective series published are based on an imperfect methodology, it appears that young age is associated with less urinary and sexual sequelae of the intervention. This notion is well known in current practice.
Young patients are less likely to experience severe postoperative urinary incontinence and permanent loss of their erections than elderly patients. A prospective analysis of clinical data from 2334 patients who underwent a prostate biopsy in the urology department of the H.M.I.M. V between January 2000 and December 2008:
The Indications for the Prostate Biopsy were
a total PSA level ≥4 ng / ml regardless of the digital rectal examination.
Conclusion
The PCa of the young man does not have characteristics different from that of the older man. Young age does not seem to influence the oncologic results of the different treatments. On the other hand, young men seem to have less risk of severe urinary and sexual complications, especially after RP. There are no specific recommendations for the management of PCa in young men. a localized PCa, two options can be conceived, the first option is to want to limit the urinary and sexual complications of radical prostatectomy. treatment such as brachytherapy, or even active surveillance, can meet this objective. The second option, on the contrary, consists in being more “aggressive” from the outset, given the usual long-life expectancy. Offering a total prostatectomy makes it possible to reserve for the patient the possibility of adjuvant or remedial radiotherapy in the event of locally advanced disease or local recurrence.
References
- Jawad EL-AZHARI (2009) Prostate cancer at the Mohamed V Military Hospital: epidemiological profile, clinical-histological and therapeutic aspects (about 568 cases). these n pp.199.
- Brawley OW, Knopf K, Merrill R (1998) The epidemiology of prostate cancer part I: descriptive epidemiology. Semin Urol Oncol 16: 187-192.
- Valeri A, Moineau MP, Azzouzi AR, Cormier L, Baschet F, et al. (2008) Étude française sur le dépistage du cancer de la prostate dans les familles à risque : bilan à 5ans dans le groupe 40–49 ans. Prog Urol 18: 736.
- Carter HB, Allaf ME, Partin AW (2007) Diagnosis and staging of prostate cancer. Campbell-Walsh Urology. Philadelphia: Saunders Elsevier pp. 2912-2931.
- Villers A, Pommier P, Bataillard A, Fervers B, Bachaud JM, et al. (2001) Standards, options et recommandations pour la prise en charge des patients atteints de cancer de la prostate non mé Janvier.
- Catalona WJ, Smith DS, Ratliff TL, Dodds KM, Coplen DE, et al. (1991) Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med 324: 1156-1161.
- Riopel M, Polascik T, Partin A, et al. (1995) Radical prostatectomy in men less than 50 years old. Urol Oncol 1: 80-83.
- Magheli A, Rais-Bahrami S, Humphreys EB, HJ Peck, Bruce JT, et al. (2007) Impact of patient age on biochemical recurrence rates following radical prostatectomy. J Urol 178(5): 1933-1938.
- Moran PS, O’Neill M, Teljeur C, Flattery M, Murphy LA, et al. (2013) Robot- assisted radical prostatectomy compared with open and laparoscopic approaches: A systematic review and meta- analysis. Int J Urol 20(3): 312-321.
- Shikanov S, Woo J, Al- Ahmadi H, Katz MH, Zagaja GP, et al. (2009) Extrafascial versus interfascial nerve- sparing robotic assisted laparoscopic radical prostatectomy: comparison of functional outcomes and positive surgical margins characteristics. Urology 74(3): 611-616.
- Marien T, Sankin A, Lepor H (2009) Factors predicting preservation of erectile function in men undergoing open radical retropubic prostatectomy. J Urol 181(4): 1817-1822.
- Cochran JS, Kadesky MC (1981) A private practice experience with adenocarcinoma of the prostate in men less than 50 years old. J Urol 125: 220-221.
- Huben R, Natarajan N, Pontes E, Mettlin C, Smart CR, et al. (1982) Carcinoma of prostate in men less than fifty years old. Data from American College of Surgeons’ National Survey. Urology 20(6): 585-588.
- (2012) Fichier des tumeurs et estimations et projections démographiques, ministère de la santé et des services sociaux. Plan commun de surveillance produit par l’infocentre de santé publique à l’Institut national de santé publique du Qué Mise à jour de l’indicateur.
- Klotz L (2004) Active surveillance with selective delayed intervention: using natural history to guide treatment in good risk prostate cancer. J Urol 172(5): S48-50.
- Dall’era MA, Konety BR, Cowan JE (2008) Active surveillance for the management of prostate cancer in a contemporary cohort. Cancer 112: 1650-1659.
- Bill-Axelson A, Holmberg L, Filen F (2008) Radical prostatectomy versus watchful waiting in localized prostate cancer: the Scandinavia prostate cancergroup-4 randomized trial. J Natl Cancer Inst 100: 1144-1154.
- Moran PS, O’Neill M, Teljeur C, Flattery M, Murphy LA, et al. (2013) Robot- assisted radical prostatectomy compared with open and laparoscopic approaches: A systematic review and meta- analysis. Int J Urol 20(3): 312-321.
- Shikanov S, Woo J, Al- Ahmadi H, Katz MH, Zagaja GP, et al. (2009) Extrafascial versus interfascial nerve- sparing roboticassisted laparoscopic radical prostatectomy: comparison of functional outcomes and positive surgical margins characteristics. Urology 74(3): 611-616.
- Marien T, Sankin A, Lepor H (2009) Factors predicting preservation of erectile function in men undergoing open radical retropubic prostatectomy. J Urol 181(4): 1817-1822.
- Kupelian PA, Elshaikh M, Reddy CA (2002) Comparison of the efficacy of local therapies for localized prostate cancer in the prostatespecific antigen era: a large single-institution experience with radical prostatectomy and external-beam radiotherapy. J Clin Oncol 20: 3376-3385.
- Nguyen TD, Poortmans PM, Van den Hulst M, O Thomas, Marco K, et al. (2005) The curative role of radiotherapy in adenocarcinoma of the prostate in patients under 55 years of age: a rare cancer network retrospective study. Radiother Oncol 77(3): 286-289.
- Rosser CJ, Chichakli R, Levy LB, DA Kuban, LG Smith, et al. (2002) Biochemical disease-free survival in men younger than 60 years with prostate cancer treated with external beam radiation. J Urol 168(2): 536-541.
- Park SS, McGrath S, Ghilezan M (2008) Impact of young age on clinical outcome in prostate cancer treated with high-dose RT in the modern era. Int J Radiat Oncol Biol Phys (72).
- Brenner DJ, Curtis RE, Hall EJ (2000) Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery. Cancer 88(2): 398-406.
- Nieder AM, Porter MP, Soloway MS (2008) Radiation therapy for prostate cancer increases subsequent risk of bladder and rectal cancer: a population based cohort study. J Urol 180(5): 2005-2009.
- Sharkey J, Cantor A, Solc Z, W Huff, Stanley DC, et al. (2005) 103Pd brachytherapy versus radical prostatectomy in patients with clinically-localized prostate cancer: a 12- year experience from a single group practice. Brachytherapy 4(1): 34-44.
- Twiss C, Slova D, Lepor H (2005) Outcomes for men younger than 50 years undergoing radical prostatectomy. Urology 66(1): 141-146.
- Magheli A, Rais-Bahrami S, Humphreys EB, Hugh JP, Bruce JT, et al. (2007) Impact of patient age on biochemical recurrence rates following radical prostatectomy. J Urol 178(5): 1933-1938.
- Twiss C, Slova D, Lepor H (2005) Outcomes for men younger than 50 years undergoing radical prostatectomy. Urology 66(1): 141-146.

 Research Article
Research Article