Abstract
The Government of India has focused on digitizing its health care, including Electronic Health Records (EHR) to provide better patient data management, seamless coordination between healthcare providers, and improving healthcare research. This paper, based on secondary information analysis and a primary survey, discusses the policies to support EHR adoption in India, the status of EHR adoption the policy gaps, infrastructure barriers, financial barriers, and other obstacles. It provides the Government of India and the health service providers with recommendations to overcome the obstacles faced and successfully implement EHR systems. For EHR to be successful, there is a need for increased funding from the private sector, the government, and partnerships/collaborations. The paper suggests ways to streamline the data collection and compilation process and address the infrastructure gaps. It presents examples of how India can learn from global best practices of implementing EHR.
Keywords: Electronic Health Records; India; Health Policy; Health Information Technology; Universal Health Coverage
Introduction
As a developing country, with the second-largest population in the world, India has an ever-growing need for quality health care. Digitalizing health care is one of the key objectives of the government to ensure equal access to treatment at a reasonable cost. The Indian government is also keen on affordable drug discoveries and health care research through the use of data generated in the country. Electronic Health Records (EHR) are at the core of India’s goals of digitalizing the health care system and moving towards universal health coverage (UHC). India is taking cognizance of the benefits of EHR systems in terms of improved patient coordination, increased patient participation, improved medical research, and reduction in health care costs.
In 2018, the Government of India (GoI) launched the UHC scheme, known as the Ayushman Bharat Yojana [1]. This national health insurance scheme has two main components - (i) the Pradhan Mantri Jan Arogya Yojana (PM-JAY) which aims to provide an INR 5,00,000 cover to the bottom 40 percent of the population for secondary and tertiary care [2] and (ii) the establishment of around 1,50,000 health and wellness centers across the country for primary care, especially in rural areas. As a result, health data is being regularly collected for the said beneficiaries and there is a mandate from the government to digitize these records and take steps towards implementing EHR systems. Several national-level policies such as National Digital Health Blueprint (2019) are being formulated to create a pan-India digital health record system. At the provider-level, large health systems like Tata Memorial Hospital and Max Hospitals Private Limited have implemented electronic medical record (EMR) systems and are moving towards EHR. However, the status of EHR adoption is not aggressively tracked, and through our survey, we try to understand the progress India has made in EHR adoption.
In this study, exploiting India’s ongoing drive of digitalizing health care in the country, we discuss the obstacles in realizing EHR systems in India and provide recommendations to help the GoI. In the subsequent sections, we discuss (a) the policies in place to support EHR adoption in India (b) the realities of EHR adoption in India (c) barriers experienced in the implementation process, and (d) the way forward to successfully implement EHRs in India.
Methodology
The study is based on policy analysis, literature review, secondary data analysis, and key informant interviews (KIIs) across 15 hospitals in India (private and government-owned) located in Delhi-National Capital Region, Tamil Nadu, and Karnataka. These states are known as the medical hubs for India and have domestic and global health systems. This pilot survey was conducted between June-October (2019) through face-toface interviews and video conferencing facilities. It focused on technology adoption, initiatives towards accelerating growth of the health-tech market in India, issues faced by hospitals in the adoption of technology with a focus on EHR, and their suggestions on way forward. The survey looked at rates of EHR adoption and perceived benefits of health information technology (IT) amongst health care providers. The hospitals included 13 private hospitals and 2 government-run hospitals with multi-specialty facilities, multiple access clinics, out-patient departments (OPD), and other remote access clinics across the country. Some of these hospitals have established global presence. Interviews were conducted with physicians, chief technical officers (CTO), chief operating officers (COO), chief information officers (CIO) or IT heads of the hospitals. The survey contained semi-structured questionnaires with some structured questions and some open-ended questions to elicit more information.
Policies to Enable EHR Adoption in India
India follows a quasi-federal structure of governance and health is a state subject in the Constitution of India. Therefore, it is up to the state governments’ discretion to implement policies formulated by the central government. Health care policies are largely formulated and implemented by the Ministry of Health and Family Welfare (MoHFW) and the government’s policy think-tank, National Institution for Transforming India (NITI) Aayog, supports the MoHFW in its endeavors. A number of schemes like the “Ayushman Bharat Yojana” is jointly managed by the MoHFW and NITI Aayog. Some key policy and strategy documents supporting the move towards EHR include MoHFW’s National Digital Health Blueprint (NDHB) of 2019 [3] and the NITI Aayog’s Health System for New India: Building Blocks (NITI Aayog, 2019), released in 2019 [4].
The NDHB (2019) provides an action plan for realizing digital health. It recognizes the need to establish a specialized organization, the National Digital Health Mission (NDHM) to drive the implementation of NDHB and facilitate the evolution of a national digital health ecosystem. The key features of the blueprint include a federated architecture, a set of architectural principles, a five-layered system of architectural building blocks, Unique Health ID (UHID), privacy and consent management, national portability, EHR, applicable standards and regulations, health analytics, MyHealth App for increased patient participation, multiple access channels like call centers for support, and the Digital Health India portal for increased data sharing between healthcare providers and patients.
While the NDHB (2019) lays out the blueprint to create a National Health Exchange (NHE) accessible to all citizens, the NITI Aayog (2019) discusses the key issues being faced as well as components and standards required for the success of digital health in India. The report outlines six “pillars” of digital health in India. These include the selection of a governance entity, registries for health data, a strategy for the development of a unified health information system, design for health insurance information systems, EHRs for patients and health care providers, and the creation of a health information infrastructure for the integration of all the mentioned components. Given that the policies are fairly recent, the next section presents the current status of EHR adoption in India.
Findings from the Primary Survey
Perceived Benefits of EHR Adoption
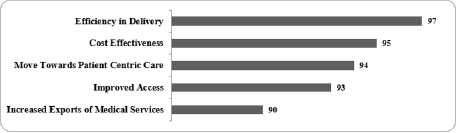
Our survey participants pointed out that by leveraging digital technologies, healthcare can be made affordable, accessible, and equitable. Additionally, it can (a) contribute to economic growth through increased investment, job creation and increase in exports of newer health products and services (b) reduce reliance on imported medical devices, and (c) allow for a more patient-centric approach. Figure 1 shows the top 5 perceived benefits of EHR implementation.
Figure 1: Perceived Benefits of the Health-tech Sector in India.
Percentage of Survey Respondents; Source: Primary Survey; Note: These responses are based on a multiple-choice questions.
Status of EHR Adoption
In India, EMR adoption gained popularity in the last decade. In our sample, all private hospitals have some form of EMR system while the public hospitals said that in villages and remote areas, there are digital access issues, and they maintain paper records. Only 8 out of the 13 hospitals were using the EMR system to record clinical data. They used this data for analysis, for quality assurance and to identify areas of improvement in hospitals. The other 5 EMR systems had health information systems (HIS), which were being used for billing and inventory management. EMRs provide improved patient data tracking. However, EMRs are not designed to be shared outside a particular practice which makes EMRs hard to be shared across medical facilities like labs, pharmacies, and specialists.
All hospitals that were surveyed have plans to either expand their EMR systems towards EHR or implement an EMR system to ease the process of recording and sharing data and leverage the same to improve health outcomes. For example- a CTO pointed out that they intend to create a biobank of diagnostic images and use it in the future for appropriately designing care for cancer. However, given the low IT budgets of the hospitals and other issues, these goals and their implementations are at a nascent stage.
Barriers to Implementing EHR Systems in India
The barriers to EHR implementations as identified by the survey and in order of their ranking is given below:
Low Public Health Expenditure
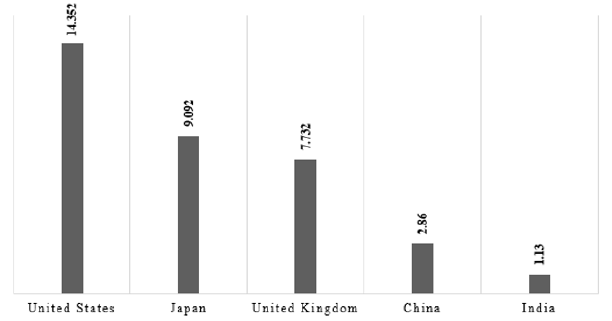
The Indian government spends only 1.13 percent of its gross domestic product (GDP) on health care (NITI Aayog (2019). Data from the Organisation for Economic Co-operation and Development (OECD) [5] shows that India’s average spending on health care is lower than that of both developed and developing countries (Figure 2).
Figure 2: India’s Total Health Expenditure (as a % of GDP) vis-à-vis other developed and developing Economies -2017
A. Infrastructure Readiness
The government hospitals pointed out that in many hospitals there is a shortage of computers for basic data entry and the data storage facility is extremely poor. According to survey participants, there has to be a basic level of technology usage across hospitals for digital healthcare government initiatives in digitalization to be successful. In addition, as of 2018, more than 4 percent of the Indian population did not have access to electricity and only 20 percent of the population used the internet [6]. Given that a large number of rural hospitals are public hospitals, uniform EHR implementation is difficult without addressing this issue.
Policy Gaps
The survey identified two key policy gaps, given below, which are essential for implementation of EHR.
A. Issues with Data Sharing and Data Security
EHR systems across the globe are maintained through the effective use of a unique identifier. In the USA, the social security number and in the UK, the national insurance or NHS number is used for this purpose. Additionally, stringent laws like the Health Insurance Portability and Accountability Act (HIPAA) of 1996 in the US and the General Data Protection Regulation GDPR in the European Union (EU) ensure that health data remains secure. India does not have a comprehensive or sector specific (for health care) data security Act. India has a unique identifier called Aadhaar. However, the lack of regulatory frameworks and policy with respect to the security of Aadhar makes it difficult for use in handling sensitive patient information. More recently, the government is trying to use Aadhar for ensuring COVID-19 related vaccination but there are issues related to how to use it in the most efficient way without compromising on data security. The Aarogya Setu or the Indian COVID–19 contact tracing, syndromic mapping and selfassessment mobile app, which was implemented by the government in the year 2020 came under several criticism on grounds of data security and could not be made mandatory.
B. Lack of Minimum Viable Standards
Survey participants pointed out that the government has not specified any technical standards standard for an integrated system of health care and service delivery. The EHR Standards 2016 mentions a list of ISO standards that hospitals may comply with. However, hospitals can voluntarily choose which standards they want to comply with. In countries such as Australia and the USA, there are minimum standard requirements that entities must abide by for effective record management and interoperability. During the survey, only a select number of health care providers follow certain standards, and even then, there is no uniformity of standards across this select group/global best practices, making it difficult to integrate EHR systems.
Other Issues
Apart from poor infrastructure and broadband connectivity, which is core to an efficient digitalization process, there are some issues like low information technology (IT) budget of the hospitals for EHR implementation. In comparison to many countries that spend close to 5 percent of the total hospital budget on IT, Indian private hospitals tend to spend only 2.5 percent of the total hospital budgets on IT. The corresponding share is much lower in government hospitals. Compared to health IT, most of the budget is spent on revenue generating components such as hospital beds and wards. Further, there is a skill and training gaps. Many governmentrun medical and nursing colleges at the state level, do have courses on the use of technology as part of their curriculum of medical degree courses. Therefore, doctors, nurses and other medical staff are ill equipped to enter the data online and hospitals have to spend time and money on training of their staff in technology. In some cases, the staff themselves are not willing to enter patient data online as they pointed out that the number of patients per doctor is very high in India and data entry is time consuming.
Recommendations and Way Forward
India may need to address the above issues, examine EHR models followed in developed countries, and customize the models to meet the requirements of the country. Some recommendations to address these issues are discussed below.
Need to Increase Funding by Government and Private Sector
As per the National Health Policy of 2017, the government wants to increase public health expenditure to 2.5 percent of GDP by 2025 from 1.5 percent in 2017. Survey participants pointed out that the target of 2.5 percent should be aggressively pursued, with a focused budget allocation towards digitization, along with attracting more investment through conducive policies and incentives. This should also include the cost of training medical professionals with the EHR systems, rules, and standards. There should be clear targets of complete digitalization of district-level hospitals and primary health care centers.
Focus on Pan-India Minimum Quality of Health Care Delivery through Private Partnership
Private hospitals account for close to 60 percent of the health care system in India. These are concentrated in urban areas while public hospitals have a larger presence in rural areas. There is a need to equip all hospitals with basic technology, infrastructure, and training. Following this pilot survey, a pan-India survey of hospitals to understand needs and gaps can help facilitate this.
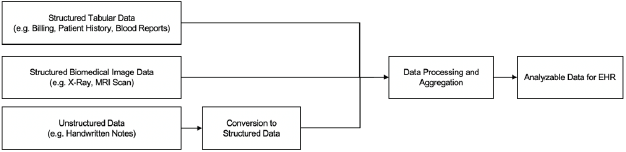
Streamline the Data Collection and Analysis
A robust data collection system is integral to EHR. It is important to define the data required, prioritize fields, and divide data fields across various user roles and stakeholders. The various datasets (e.g. laboratory results, diagnosis, clinical data, etc.) in a central repository for access and use. For benefitting from NHE, the use of fields supported by the central repository needs to be mandatorily followed by all individual EHR systems. Also, as shown in Figure 3, for unstructured data (like images, doctors’ notes, etc.), a mechanism to convert to structured data as defined by the repository should be implemented making health data easier to maintain. For identification, the UHID can be supported along with the Aadhaar card to provide more security in the form of dual authentication. For regions with low infrastructure, a process should be outlined to assist secure digitized data at regular intervals.
Enforce Minimum Viable Standards
The National electronic Health Authority (NeHA) [7] was set up in 2015 under the MoHFW and the MoHFW drafted the Digital Information Security in Healthcare Act (DISHA) [8] in 2017 to address the growing concerns for EHR Standards. However, these standards were not enforced and stakeholders raised multiple concerns. Thus, in order to ensure secure interoperability, the MoHFW in line with global best practices should specify appropriate global EHR standards such as the Fast Healthcare Interoperability Resources (FHIR) standards so that patient records are readily “available, discoverable, and understandable” [9].
Addressing Infrastructure and Training Gaps
Modern EHR systems require computers, high-speed seamless broadband connectivity along with quality power supply. It is essential to first set up the required infrastructure before boosting health-tech. In order to allow for the easy implementation of health record systems, the government can give a mandate that clinical establishments across countries should have basic computers with, internet connectivity. As a step ahead, the government in its primary care centers under the Ayushman Bharat Yojana should also provide practitioners with these facilities along with smartphones/ tablets, to allow real-time data collection. At the same time students in healthcare should be trained in use of technology as part of their course curriculum. The National Skill Development Council can partner with medical schools and hospitals on digital training. In this context, India can look at how some other countries have implemented their digitalization process and there can be more collaboration and partnerships through platform like G20 for which India is going to take up the Presidency in 2022.
Conclusion
The GoI and the Indian health care industry understand the widespread benefits of implementing EHR systems. As a result, they are committed to adopting these systems on a grand scale. As of date, the adoption of such systems is limited to the private health industry. Our survey identified several issues at the government and health care provider levels impeding the efforts towards EHR adoption. Based on the findings, we make recommendations towards increasing funding, focusing on business and government partnerships, streamlining the data collection process, enforcing minimum viable standards, and addressing infrastructure barriers to increase EHR adoption in the country. India can learn from global best practices of implementing EHR and customize it to the country’s requirements.
Acknowledgements
We would like to thank ICRIER for giving us opportunity to work in this area and to and the Confederation of Indian Industries (CII) for connecting to their members. We are grateful to our survey participants for taking the time out to participate in the interviews. This research is part of the on-going study by ICRIER on providing inputs to Indian government on healthcare sector in the context of doemstic reforms and G20 discussions.
References
- (2018) Press Information Bureau. Ayushman Bharat for a new India -2022.
- (2019) World Economic Forum. What India's route to universal health coverage can teach the world.
- (2019) Ministry of Health & Family Welfare, Government of India. Final Report on National Digital Health Blueprint.
- (2019) National Institute for Transforming India (NITI) Aayog. Health System for A New India: Building Blocks.
- (2020) OECD. Health spending (indicator). doi: 10.1787/8643de7e-en.
- (2020) World Bank. World Bank Open Data.
- (2013) NeHA. National eHealth Authority (NeHA). National Health Portal of India.
- (2017) Ministry of Health & Family Welfare, Government of India. Digital Information Security in Healthcare.
- Saripalle R, Runyan C, Russell M (2019) Using HL7 FHIR to achieve interoperability in patient health record. J Biomed Inform 94: 103188.

 Review Article
Review Article