Abstract
Introduction: An Intensive Care Unit (ICU) is an autonomous department, which requires the cooperation of specialized health care professionals and the use of advanced technology in order to provide intensive patient care. The most common infections occurring in the ICU are urinary tract infections, Ventilator Associated Pneumonia, intravascular catheter infections and infectious diarrhoea.
Purpose: To investigate the knowledge and attitudes of ICU nursing staff concerning the prevention and treatment of infection.
Methodology: Experimental design was used. Only the experimental group attended an interactive lecture based on the newly constructed protocol by actively participating in the program. The information was collected using a questionnaire.
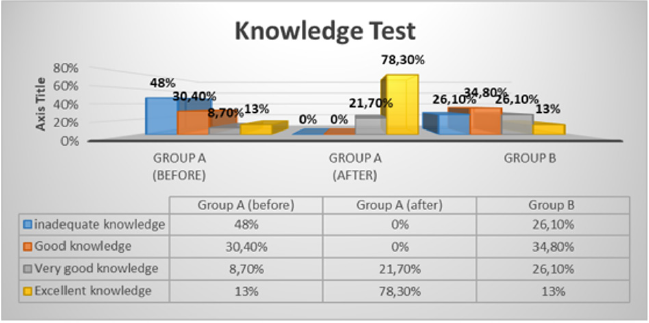
Result: Upon completion of the lecture regarding necessary infection control interventions, the percentage of the experimental group’s (Group A) knowledge increased significantly (78.3% rated excellent). Although nurses agree that nursing protocols help nurses to provide a high level of nursing care, ICU nursing staff agree that the implementation of nursing protocols reduces the rate of infections.
Conclusion: Establishing new and contemporary nursing protocols and updating guidelines regarding infection control in the ICU, continuous education and webinar courses can prevent nosocomial infection and improve the quality of nursing care provided.
Keywords: Nosocomial Infections; ICU; Nursing Interventions; Protocols
Introduction
In recent years there is an increase in nosocomial infections worldwide. Bacteria spread mainly through the air, direct or indirect contact with contaminated objects and surfaces as well as among patients and health care professionals. The main factor associated with nosocomial infections is prolonged hospitalization, especially for critically ill patients in Intensive Care Units (ICUs) [1]. In addition, there is a direct link between nosocomial infections and medical or nursing interventions such as urinary catheter placement, endovascular catheters, tracheal or tracheostomy care, and ventilator use [2]. The incidence of nosocomial infections in the ICU has been reported to be approximately 2 to 5 times higher than in other hospital departments [3]. The increased morbidity and mortality associated with nosocomial infections in the ICU is a matter of serious concern. More than one hundred thousand cases of nosocomial infections are recorded each year in the U.K., causing five thousand deaths at a cost of more than 1.6 billion euros [4]. According to the Centre for Disease Control and Prevention (CDC), nosocomial infections are one of the leading causes of death in the United States [5].
Causes of Infection
The majority of nosocomial infections (90%) are mainly caused by bacteria [6], while immunosuppressed patients with malignant disease or HIV are considered to be high risk. Gramnegative bacteria, such as coliforms, Enterobacteriaceae, clepsiella, and pseudomonas, are most common in patients with nosocomial infections [7]. In recent years, acinetobacter seems to be appearing more often in the ICU. Gram-positive bacteria, Staphylococcus aureus (cutaneous and epidermidis) and enterococcus are becoming more common due to the extensive use of catheters [8].
Risk Factors
They are classified into two main categories. The first category includes factors that allow pathogenic microorganisms to invade areas of the patient’s body that are more easily infected, due to surgery, catheter insertion, intravenous delivery, tracheal intubation, or use of technical equipment such as respirators [9]. The second category includes factors that reduce the patient’s immune resistance due to a disorder of chemical or cellular immunity, such as the nature and severity of the patient’s underlying disease, the type of medication provided and radiotherapy [10].
Intensive Care Unit (ICU)
Approximately 12% of the total number of hospital beds (within a hospital), are allocated to intensive care services within the ICU [11]. Intensive care includes, 24-hour continuous monitoring, 1:1 nurse -patient ratio, interdisciplinary care, patient support regarding organ and system deficiencies as well as continuous training and education of medical and nursing staff [12]. The role of the nurse in the ICU is not limited to the performance of simple nursing duties such as measuring and recording but provides a holistic approach to the disease manifestation and to the patient.
Nursing education should focus on the development of knowledge and skills as well as promote continuing education and research thus, providing quality nursing care [13]. Highly trained nursing staff maintains and improves the quality of care provided. According to the literature quality indicators such as errors in medication due to staff stress as well as nosocomial infections are significantly reduced through continuing education (CE) and increasing the number of competent staff members [14]. Simultaneously, nursing science can evolve through continuing education and the nurses themselves can gain autonomy, confidence and satisfaction from their work. Providing continuing education for nurses is very important to patients’ positive outcome, creating a reliable professional identity as well enhancing cooperation between nurses [15].
A study by Nia et al. [16] included 10 general hospitals in China involving 2,727 nurses, found that 97.3% had participated in a continuing education program in the last 12 months and 92.2% claimed they were familiar with the value of continuing education. Also, Wolff-Skaalvik, Gaski and Norbye [17], while conducting a study in Norway, found that 56% of nurses employed in a position with a corresponding specialization had voluntarily participated in a continuing education program, while 31% had completed more than one educational program. However, in Greece, the shortage of nursing staff does not facilitate their availability to participate in continuing education programs and in addition and the lack of funds are some obstacles regarding the implementation of such programs [18]. Furthermore, even though progress has been made in recent years, it is necessary to increase the number of ICU beds. After a relevant study, Zakynthinos and Vrettou [19] estimated that the real needs for ICU beds in the hospitals are 4% of the total beds for local hospitals and over 10% of those for regional or university hospitals. After the covid-19 pandemic, the situation has improved considerably since according to the Ministry of Health the available beds in ICUs in the regional hospitals have increased by 30%.
Infections in the ICU
The most common infections in the ICU are the following:
a) Urinary tract infections: Although urinary tract infections (UTIs) are considered to have a good prognosis, the mortality of microbial urinary tract infections is close to 30% [20]. Risk factors for the development of microbial UTI are gender (women outnumber men), diabetes, old age and microbial colonization of the urinary tract [21].
b) Intravascular catheter infections are one of the three leading causes of nosocomial sepsis, often including up to 20% of all ICU infections [22]. Despite the development of antibiotics and the better understanding of the mechanism of this type of infection, the mortality from bacteremia associated with catheters remains high (10-20%) [23]. A review by Shah et al. [24] concluded that the incidence of Catheter-related bloodstream infection (CRBSI) is between 0.1% and 22.5% and between 0.1 and 2.7 per 1000 days, respectively.
c) Hospital-acquired pneumonia (HAP) and ventilatorassociated pneumonia (VAP) are the leading causes of morbidity and mortality, despite improved antimicrobial therapy, hospital care and prevention measures [25]. VAP usually affects critically ill patients admitted to the ICU, while resulting in an increase in hospitalization days and a mortality rate of up to 20-30% [26].
d) Infections that develop in immunosuppressed patients such as, infectious diarrhoea. Diarrhoea that occurs in the ICU is a very common problem. Its cause is often based on many factors, can lead to a high number of adverse clinical symptoms, and is associated with extended hospitalization and mortality in ICU patients [27].
Effects of Nosocomial Infections
Nosocomial infections are responsible for increasing mortality, morbidity, rising costs and extended hospitalization (Shepherd & Pottinger, 2013). Specifically, the overall mortality of nosocomial infections is estimated at 3% [28]. Seventy-five per cent (75%) of patients with nosocomial pneumonia and 25% of patients with bacteremia will die, while patients with a catheter infection are three times more likely to die than patients without a urinary catheter (Mody et al, 2017). In addition, the direct financial cost due to the onset of patient infection in the hospital constitutes a significant percentage of a country’s annual expenditure. It is estimated that in the United States this cost is 3.5 - 6.7 billion dollars per year [29], in England 1.3 - 1.6 billion euros total cost per year and in Italy 2.5 - 5.0 billion euros [30], while the economic cost in Europe is 7 billion euros [31]. The cost of treating patients with an infection caused by antibiotic-resistant strains of Acinetobacter, Enterobacter, E. Coli, Klebsiella, and Pseudomonas increased by 29.3% compared to patients with infections caused by antibiotic resistant bacteria strains [29].
Finally, a patient staying in a hospital for longer periods of time is psychologically affected. Being confined in the hospital increases anxiety and fear with patients showing signs of depression and anger. Finally, there is a similar effect on the patients’ family, which continues after the patients’ discharge from the hospital. Research on this subject has been conducted by Davies et al. [32], in England and Wales, who studied the use of guidelines for the diagnosis and management of burn infections in children. Saint et al. [33] studied the prevention of urinary tract infections associated with the use of a catheter while Brewster, Tarrant, and Dixon-Woods [34] conducted a qualitative study of views and effective management of health care-related infections. Finally, Cason et al. [35] examined the application of the Nursing Guidelines to respiratory-related pneumonia.
An extensive review of the literature involving Greek data demonstrated that there are reviews of ICU infections such as central venous catheter treatment [36]. Most research is descriptive, focusing on hand hygiene protocol guidelines [37], knowledge related to preventing and treating bed sores, safety tactics for the prevention of surgical infections [38] and methods of preventing respiratory-related pneumonia [39], as well as the effect of the nursing workload on the incidence of infections and mortality of ICU patients. It seems that there is a lack of research studies in Greece on the attitudes and knowledge of nursing staff working in the ICU concerning the prevention and treatment of infections, while examining the four main infections that occur in the ICU.
Materials & Methods
Experimental design was used in order to investigate and compare the knowledge and attitudes of nurses regarding the prevention and treatment of infections that occur in the ICU in public hospitals in the region of Western Greece. An experiment offers the possibility of future repetition, provides time for conclusions, accurate measurements and finally provides the possibility of constructing a graph of the results. In the present study a pre-post study design between groups was used. The research hypotheses were:
a) Nursing staff knowledge concerning catheter infections is incomplete.
b) Nursing staff knowledge will increase significantly after the implementation and completion of a training program concerning urinary tract infections.
c) Nursing staff knowledge of respiratory infections (VAP) is incomplete.
d) Nursing staff knowledge will increase significantly after the implementation and completion of a training program concerning respiratory infections (VAP).
Data Collection Method
Data were collected using a questionnaire with a total of 34 questions constructed by the researchers. The questionnaire consisted of three parts, in which the content, structure and wording were the same in both groups. In the first part of the questionnaire, 10 questions were related to knowledge of infections in the ICU. The questions were developed according to recent literature and protocols used in the U.K. and the U.S.A with a response of true or false as a possible answer where the 10 questions examined knowledge of infections in the ICU. Each question had a score of 1, so the minimum score was 0 (none correct) and the maximum was 10. The Greek academic knowledge scale which is divided into 4 categories was used: 0-4.9 incomplete knowledge, 5-6,4 good knowledge, 6.5-8.4 very good knowledge and 8.5-10 excellent knowledge.
The second part included 11 questions examining the nursing staff’s attitudes on infections in the ICU, 4 questions examining nursing protocols and 3 questions regarding the training of nurses on infections in the ICU. A 5-point Likert scale (Strongly Agree to Strongly Disagree), 3-point scale (yes, no, I do not know/ do not answer) and rating scales from “too much” to “none” were used. Finally, the 3rd part consisted of demographic questions (6 in total). In addition, the degree of reliability and validity of the research was examined. The Cronbach alpha (a) reliability index was 0.69 which is considered satisfactory. The knowledge test was designed based on the literature review and in order to establish its reliability was evaluated by a panel of experts which included a professor of nursing specialized in intensive care and two nurses who had postgraduate degrees and at least 10 years of working experience in the ICU. Therefore, they concluded that the structure and content of the questionnaire was satisfactory. A pilot survey was conducted including a sample of five (5) ICU nurses in order to identify possible discrepancies with the questionnaire. The results showed that the participating nurses did not encounter any problems in understanding and answering the questionnaire.
Procedure
The study was carried out in adult ICUs public hospitals within the region of Western Greece. The research protocols were approved by each hospital’s ethics committee (1. Name: Scientific Board for Research Ethics and Deontology, University General Hospital of Patras “Panagia Boithia”, Approval number: 14412/30-5-2018, 2. Name: Scientific Board for Research Ethics, General Hospital of Patras “St Andreas”, Approval number: 13767/23-4-2018). The sample was randomly divided (in alphabetical order) into two groups (control- experimental). The ICU nurse managers were informed about the division of the nurses into groups and provided a list of the nursing staff. When the teams were established, the researchers informed the staff about the study.
Due to the fact that protocols on urinary tract infections, intravascular catheters, ventilator and sepsis infections, either do not exist or are not applied (they are not contemporary), a new and modern protocol was developed from the literature [40]. The experimental group attended an interactive lecture based on newly constructed protocols by actively participating in the program, contrary to the control group. Audio-visual media (laptops and projectors) were used to conduct the lectures. Each lecture (PowerPoint) lasted 40-50 minutes and took place in the hospitals. Due to the morning shift increased workload, the lectures were held in the afternoons in consultation with the nurse managers. It was difficult for the members of the staff to participate due to rotation schedules. As a result, the lectures were presented to groups of 5-6 nurses. Finally, measurements were repeated after the administration of the experimental intervention.
Sample
In the present study, convenience sampling was used due to financial resources. The study included ICU nurses from two public hospitals within the region of Western Greece. A total of 53 nurses were approached while, 45 participated in the survey (84.9%). Group A (experimental group) was divided into 2 sub-groups of 15 nurses each: before and after the effect and group B (control group) included 15 nurses.
Statistical Analysis
The collected data were analysed using the statistical program SPSS 24. Statistical significance level was set at p <0.05.
Survey Results
Sample Characteristics: Τhe majority of the participants were women, aged 26-63 years (x = 40.42), did not hold a postgraduate master’s degree while their clinical experience ranged from 1-36 years (x = 11.84).
Knowledge Test Results: Graph 1: Knowledge test of groups A (before and after the intervention) and Group B (control). Group A demonstrated an inadequate knowledge level before the intervention (48%) (x = 5.13), while after the intervention the vast majority of the participants (78.3%) had excellent knowledge (x = 9.22). In Group B (control group) 34.8% had good knowledge and 26.1% very good (x = 6.09). The nurses of group A (after intervention) have statistically better knowledge than the other two groups (x2 = 46.672, df = 16, p <0.05).
Questionnaire Results (Opinions): The majority, of both groups (control & experimental) strongly agree that they should wash hands after removing gloves (73.1% and 69.5% respectively), however the lack of time (56.4% and 52.8%) and personal protective equipment (PPE) such as gloves, aprons, and masks (52% and 69.4%) make it difficult for them to follow precautionary measures. In addition, the majority of groups strongly agree that nursing protocols help them provide a high level of nursing care (65.2% and 52.1%) and consider that their implementation reduces the rate of infections (91.3% and 90.7%).
It is noteworthy that the majority of nurses, in both groups, report that there are no nursing care protocols used in the ICU for the treatment of intravascular catheters and tracheobronchial aspiration (91.3% and 60.9% respectively). Finally, the nursing staff in all groups claim that the knowledge they received during their undergraduate education concerning infections offered them minimal to no help in the management of infections in the ICU (73.9% and 63.7%), while nursing personnel continuing education and training department of the hospital which they work in has not offered any information concerning infection control (86.5% and 73.8%).
Correlation Per Group
The study showed statistically significant results in the following correlations:
a) Group A (before the intervention): nurses employed in hospital A have better knowledge than the nurses at hospital B (x2 = 5.481, p <0.05).
b) Group A: Although knowledge increased in both groups, hospital A nursing staff performed better (x2 = 5.759, p <0.05).
c) Group B: Nurses with experience in ICU between 9-16 years, demonstrated a higher level of knowledge (x2 = 11.165, p <0.05).
Discussion
Infections in ICU patients are accompanied by high mortality, increased length of hospital stay [41] thus affecting patient recovery and increasing costs for the hospital as well as the patient. The role of the nurse in the ICU is multidimensional, knowledge, skills and abilities to carry out appropriate nursing interventions and provide a high level of nursing care are needed. Nursing education should be continuously updated focusing on knowledge as well as skills, continuing education and nursing research [42].
The present study demonstrated that the knowledge of nurses regarding the most common infections in the ICU (respiratoryrelated pneumonia (VAP) and intravascular catheter) is inadequate. This is probably due to the fact that the protocols for nursing interventions to prevent and treat these infections are either outdated or non-existent. Most developed countries have up-todate protocols, thus educating staff on the latest infection data. However, the nurses’ knowledge increased significantly (78.3% excellent level of knowledge) after the lecture on infection control was completed.
Additionally, nurses in both groups agreed that aseptic technique should be applied when treating intravascular catheters. Most infections can be prevented by using aseptic technique when inserting, treating and changing catheters [43]. Still, hand hygiene is the most important and effective skill for preventing and controlling the spread of hospital-related infections. Fligou et al. [44] in a prospective study, found that the implementation of intensive hand hygiene protocols by ICU staff in conjunction with total indoor reconstruction projects can lead to a statistically significant reduction in the frequency of VAP. A study by Juneja et al. [45] showed that 94.4% and 97.6% of health care professionals working in the ICU mentioned premature ventilator weaning and hand washing as key preventative measures, respectively.
It is also important to note that in the present study, the majority of nurses in all groups agree that nursing protocols help provide a high level of nursing care thus decreasing the number of infections. Nursing protocols are comprehensive structured plans describing the procedure a nurse should follow during an intervention. The widespread interest in clinical protocols stems from issues most healthcare systems are dealing with such as, the rising cost of healthcare and the growing demand for quality care [46].
The importance of nursing protocols was shown in the present research as the intervention team significantly increased their knowledge after the lectures. One of the most important advantages of nursing protocols is the quality they have as “evidence”, which are the basic rules of quality. The application of the most up-todate knowledge in daily clinical practice aims mainly at reducing ineffective and costly practices [47]. In addition, with the existence and implementation of protocols there is an interdisciplinary and holistic approach to patient problems resulting in health care professionals being more satisfied with their work. It is important to mention that more than half of the Greek hospital ICUs, do not use nursing intervention protocols thus, resulting in poor quality nursing care, professional burnout, low professional satisfaction and increased hospital stay, increased costs and a shortage of ICU beds.
Another issue highlighted by this study, the majority of nurses mentioned that the nursing personnel continuing education and training department did not offer information concerning infection control. According to the literature, training and continuing education programs are important in reducing VAP [48]. The educational programs that can be applied in all ICUs of hospitals contribute significantly to the control of nosocomial infections, reducing patient morbidity rates, as well as hospital stay and costs [47].
Undergraduate Nursing programs play an important role in providing quality nursing care. Each program’s objective is to prepare nurses who are able to promote, protect, maintain and restore health. Nevertheless, this study has shown that the knowledge acquired at the undergraduate level regarding the treatment of infections in the ICU did not offer them help in the management of infections. Finally, group B (control group) has shown that the greater the experience in the department the better the scores of the nursing staff in the knowledge test. Similar results were found in the study of Blot et al. [49] which showed that experienced nurses have a higher level of knowledge compared to nurses with less than 5 years of experience [50].
Study Limitations
A limitation of this research study is the small sample from one Region. Although the research provided important data on the knowledge and attitudes of ICU nursing staff concerning prevention and treatment of infections, it is considered necessary in the future to conduct a study with a larger sample working in hospitals in various Greek cities.
Conclusion
Nosocomial infections have increased since the bacteria that cause these infections have become antibiotic resistant. Also, the lack of funding and understaffing of public hospitals contribute to the increase of nosocomial infections. Greece has high rates of antibiotic use thus prevention plays a crucial role in the treatment of infections. This study demonstrates both the necessity of continuous education and training programs for the prevention and treatment infections in the ICU and the importance of the implementation of new and up to date protocols for their prevention. The results of the ICU nurses’ knowledge test of most common infections were not very satisfactory but after the researchers intervened by conducting lectures the level of knowledge increased significantly. Establishing training programs for nurses and encouraging them to continue their education and training as well as establishing new and up to date nursing protocols, are the key points in preventing and treating infections in the ICU.
Suggestions
According to the results of this study, the following proposals are made:
a) Increasing ICU nursing staff
b) Establish new and up to date nursing protocols related to infections in ICUs.
c) Continuous education and training, updated with new instructions on how to prevent infection in the ICU provided by the nursing personnel continuing education and training department.
d) Cooperation between educational institutions and the nursing personnel continuing education and training department in order to offer courses in hospitals (distance learning, e-learning). Creating webinars (4 to 5 lectures per month), which include new data on infections, such as clinical guidelines and nursing interventions.
Implications for Clinical Practice
a) Establishing new and up to date nursing protocols, are the key points in preventing and treating infections in the ICU.
b) Implementing nursing protocols will reduce the cost of healthcare and improve quality of care.
c) Continuous education and training programs are necessary for the prevention and treatment infections in the ICU.
Acknowledgement
All contributing authors have significantly contributed to the research and writing of the manuscript and approved the content before submission.
Source of Funding
Self-funding.
Conflict of Interest
Nil.
References
- Göçmez C, Çelik F, Tekin R, Kamaşak K, Turan Y, et al. (2014) Evaluation of risk factors affecting hospital-acquired infections in the neurosurgery intensive care unit. Int J Neurosci 124 (7): 503-508.
- Hsieh YH, Liu J, Tzeng YH, Wu JJ (2014) Impact of visitors and hospital staff on nosocomial transmission and spread to community. Theor Biol 356: 20-29.
- Huang HP, Chen B, Wang HY, He M (2016) The efficacy of daily chlorhexidine bathing for preventing healthcare-associated infections in adult intensive care units. Korean J Intern Med 31(6): 1159-1170.
- Kadambari S, Pollard AJ, Goldacre MJ, Goldacre R (2020) Congenital viral infections in England over five decades: a population-based observational study. Lancet Infect Dis 20(2): 220-229.
- Baker D, Quinn B (2018) Hospital Acquired Pneumonia Prevention Initiative-2: Incidence of nonventilator hospital-acquired pneumonia in the United States. Am J Infect Control 46(1): 2-7.
- Freestone PP, Al-Dayan N, Lyte M (2016) Staphylococci, Catecholamine Inotropes and Hospital-Acquired Infections. Adv Exp Med Biol 874: 183-199.
- MacVane SH (2017) Antimicrobial Resistance in the Intensive Care Unit: A Focus on Gram-Negative Bacterial Infections. J Intensive Care Med 32 (1): 25-37.
- Dasgupta S, Das S, Chawan N, Hazra A (2015) Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med 19(1): 14-20.
- Chen LX, Zhang XX, Gong CX, Hua Xi Kou, Qiang Yi, et al. (2019) The risk factors and preventive measures of hospital infections on preoperative children with cleft lips and palates. West China Journal of Stomatology 37(3): 290-294.
- Wałaszek M, Kosiarska A, Gniadek A, Kołpa M, Wolak Z, et al. (2016) The risk factors for hospital-acquired pneumonia in the Intensive Care Unit. Epidemiol 70(1): 15-20, 107-110.
- Chowdhury D, Duggal AK (2017) Intensive care unit models: Do you want them to be open or closed? A critical review. Neurol India 65(1): 39-45.
- Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, et al. (2017) The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med 43(8): 1105-1122.
- Conneely A, Hunter D (2012) Introducing first-year student placements in critical care. Nurs Stand 26(23): 35-40.
- Ross K, Barr J, Stevens J (2013) Mandatory continuing professional development requirements: what does this mean for Australian nurses. BMC Nursing 12: 9.
- Megginson LA (2008) Education: 21st century barriers and incentives. Journal of Nursing Management 16: 47-55.
- Nia C, Huaa Y, Wallenb G, XuaS., Lic L (2014) Continuing education among Chinese nurses: a general hospital – based study. Nurse Educ 34(4): 592-597.
- Wolff-Skaalvik M, Gaski M, Norbye B (2014) Decentralized nursing education in Northern Norway: a basis for continuing education to meet competence needs in rural Arctic healthcare services. Int. J. Circumpolar Health 73: 10.3402.
- Κadda Ο (2013) The necessity of continuing nursing education. The Step of Asclepius 12 (2): 105-107.
- Zakithinos S, Vrettou X (2015) Issues in Intensive Care Units. Association of Greek Academic Libraries, Athens, Greece.
- Tedja R, Wentink J, O'Horo JC, Thompson R, Sampathkumar P (2015) Catheter-Associated Urinary Tract Infections in Intensive Care Unit Patients. Infect Control Hosp Epidemiol 36(11): 1330-1334.
- Lo E, Nicolle E, Coffin S, Gould C, Maragakis L, et al. (2014) Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 35: 464-479.
- Rupp ME, Karnatak R (2018) Intravascular Catheter-Related Bloodstream Infections. Infect Dis Clin North Am 32(4): 765-787.
- Patterson J, Malani P, Maragakis L (2010) Infection control in the intensive care unit: Progress and challenges in system and accountability. Critical Care Medicine 38: S363-S372.
- Shah H, Bosch W, Thompson K, Hellinger W (2013) Intravascular Catheter-Related Bloodstream Infection. Neurohospitalist 3(3): 144-151.
- Martin-Loeches I, Rodriguez AH, Torres A (2018) New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe. Curr Opin Crit Care 24(5): 347-352.
- Letchford E, Bench S (2018) Ventilator-associated pneumonia and suction: a review of the literature. Br J Nurs 27(1): 13-18.
- Tirlapur N, Puthucheary Z, Cooper J, Sanders J, Coen P, et al. (2016) Diarrhoea in the critically ill is common, associated with poor outcome, and rarely due to Clostridium difficile. Sci Rep 6: 24691.
- Fleischmann C, Thomas-Rueddel DO, Hartmann M, Hartog CS, Welte T, et al. (2016) Hospital Incidence and Mortality Rates of Sepsis. Dtsch Arztebl Int 113(10): 159-166.
- Stone PW, Kunches L, Hirschhorn L (2009) Cost of hospital-associated infections in Massachusetts. American Journal of Infection Control 37(3): 210-214.
- Agozzino E, Di Palma MA, Gimigliano A, Piro A (2008) Economic impact of healthcare-associated infections. Igiene e Sanita Pubblica 64(5): 655-670.
- (2010) WHO. A Brief Synopsis on Patient Safety. WHO, Geneva, Switzerland.
- Davies A, Spickett-Jones F, Brock P, Coy K, Young A (2017) Variations in guideline use and practice relating to diagnosis and management of infection in paediatric burns services in England and Wales: A national survey. Burns 43(1): 215-222.
- Saint S, Greene T, Krein S, Rogers M, Ratz D, et al. (2016) A Program to Prevent Catheter-Associated Urinary Tract Infection in Acute Care. N Engl J Med 374: 2111-2119.
- Brewster, L, Tarrant C, Dixon-Woods M (2016) Qualitative study of views and experiences of performance management for healthcare-associated infections, Journal of Hospital Infection 94(1): 41-47.
- Cason C, Tyner T, Saunders S, Broome L (2007) Nurses’ Implementation of Guidelines for Ventilator-Associated Pneumonia from the Centers for Disease Control and Prevention. Am J Crit Care 16 (1): 28-37.
- Kollia T, Previzi Ε (2015) Care of central venous catheters in ICU. The Step of Asclepius 14 (2): 125-135.
- Stafilidis S, Triantafillidou S, Sita B, Kafkia T (2015) Investigate the degree of compliance of the nursing staff in the implementation and observance of hand hygiene protocols. The Step of Asclepius 14 (4): 185-193.
- Tsianti E, Zougou T, Rozeberg T (2016) Investigate the nurse’s knowledge in the techniques for the prevention of surgical infections. Perioperative Nursing 5 (1): 35-43.
- Levidiotou Ε, Papakosta -Papadimitriou L, Troupis G, Mathaiou P, Baseta Α, et al. (2013) Investigate nurses' knowledge to prevent respiratory-derived pneumonia. Perioperative Nursing 1 (1): 10-17.
- (2015) The Faculty of Intensive Care Medicine - The Intensive Care Society. (2015) Guidelines for the Provision of Intensive Care Services, UK.
- Shepherd AK, Pottinger PS (2013) Management of urinary tract infections in the era of increasing antimicrobial resistance. Med Clin North Am 97(4): 737-757.
- Sibandze BT, Scafide KN (2018) Among nurses, how does education level impact professional values? A systematic review. Int Nurs Rev 65(1): 65-77.
- Esposito M, Guillari A, Angelillo F (2017) Knowledge, attitudes, and practice on the prevention of central line-associated bloodstream infections among nurses in oncological care: A cross-sectional study in an area of southern Italy. PLoS ONE 12(6): e0180473.
- Fligou F, Gotsi Α, Zotou Α, Sarakatsanos Ι, Boulovana Μ, et al. (2011) Reduction of respiratory-related pneumonia and mortality in the ICU following hygiene protocols and staff training program. Greek Anesthesiology 44 (1): 56-63.
- Juneja D, Singh O, Javeri Y, Arora V, Dang R, et al. (2011) Prevention and management of ventilator-associated pneumonia: A survey on current practices by intensivists practicing in the Indian subcontinent. Indian J Anaesth 55(2): 122-128.
- Chong V, Schultz TJ, Donnelly F (2019) Clinical protocols for adults with acute abdominal pain in Australian emergency departments. J Eval Clin Pract 25(3): 412-419.
- Durant DJ (2017) Nurse-driven protocols and the prevention of catheter-associated urinary tract infections: A systematic review. Am J Infect Control 45(12): 1331-1341.
- Hill C (2016) Nurse-led implementation of a ventilator-associated pneumonia care bundle in a children's critical care unit. Nurs Child Young People 28(4): 23-27.
- Blot SI, Labeau S, Vandijck D, Van Aken P, Claes B (2007) Executive Board of the Flemish Society for Critical Care Nurses. Evidence based guidelines for the prevention of ventilator-associated pneumonia: results of a knowledge test among intensive care nurses. Intensive Care Med 33(8): 1463-1467.
- (2017) Public Health England. 2017 Management and treatment of common infections, Antibiotic guidance for primary care: For consultation and local adaptation. London.

 Research Article
Research Article