Abstract
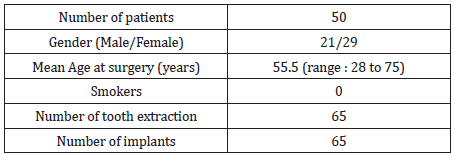
This study documents the long-term performance of the Supercrit® viral-inactivated bone allografts in extraction sockets grafting with immediate implant placement. Data were collected from files of 50 patients (29 females, 21 males, mean age of 55.5 years) undergoing immediate implant placement into fresh extraction socket with the supercritical CO2 viral-inactivated allogenic bone grafts (Supercrit® process, BIOBank, Lieusaint, France). 65 implants were placed mainly in the posterior maxilla. At a mean 9.7 years (range: 9 to 10 years), 62 implants were well osseointegrated and functioning. 3 implants failed due to non-osteointegration and were removed 6, 8, and 9-months postsurgery, respectively. The overall implant 10-year survival rate was 95.4% (CI: 90.3 to 100%). The mean marginal bone loss was 0.5 mm (SD:1.6) at the latest follow-up. Within the limitations of this study, the supercritical CO2 viral inactivated bone allograft as a grafting material during immediate implant placement in extraction sockets is a valuable option allowing short treatment time and high long-term implant survival (Figure 1).
Introduction
Allogeneic bone grafts, whether fresh, frozen, or freeze-dried, have several advantages, including reduced surgical morbidity, shorter operating times, and greater availability and quantity per autogenic bone [1,2]. Histological and histomorphometric results show that allogeneic bone has osteoconductive properties like autogenic bone [3]. The supercritical CO2 (Supercrit®) process viral-inactivated allogenic bone grafts (BIOBank, 3, rue Georges Charpak - 77127 Lieusaint – France) are derived exclusively from human femoral heads collected from living donors who have undergone hip replacement surgery in accordance with European regulations. The femoral heads are cleaned and viral- inactivated using supercritical CO2 extraction. A terminal gamma irradiation step at 25 kGy renders the packaged bone grafts completely sterile. The supercritical CO2 process has no effect on the mineral and collagen composition of the bone matrix, preserving trabecular bone tissue integrity and mechanical strength comparable to fresh bone.
As a result, the supercritical CO2 process has osteoconductive properties. Following the extraction of one or more teeth, oral implants inserted into alveolar cavities filled with various graft materials demonstrated a high survival rate greater than 94 percent at a minimum 5-year follow-up [4-7]. There has been little research on the long-term clinical efficacy of bone graft in post-extraction filling and the preservation of bone volume in the alveolar ridge [4-9]. The goal of this study is to document the long-term efficacy and safety of using BIOBank supercritical CO2 viral-inactivated allogenic bone graft in extraction socket filling and alveolar ridge augmentation. The results of osteointegration, implant survival, and radiographic changes in the graft area were compared to previous studies on other graft materials.
Materials and Methods
Patient
Fifty patients who underwent extraction socket bone grafting
with the supercritical CO2 cancellous bone powder in the Oral
Surgery Department, Clinique du Parc in Lyon from May 2009 to
October 2010 were recruited in this study. The eligible criteria
were:
(a) At least 18 years of age;
(b) Absence of any local, or systematic diseases that might
contraindicate the tooth extraction surgery;
(c) In need for tooth extraction with immediate implant placement,
including osteotomy
(d) Evaluated preoperatively, at immediate postoperative and at
long-term by means of a cone-beam computed tomography
(CBCT) and/or panoramic radiographs, and
(e) Patients able to read and understand the patient information
form.
This study was conducted in accordance with all applicable
regulations including the French Data Protection Authority (the
CNIL) Reference Methodology MR003 and with the principles of
the Declaration of Helsinki. All eligible patients were informed and
consented before participating in any study-related activities. This
was a post-market surveillance data collection as part of regulatory
requirements in compliance with MEDDEV 2.7/1 rev.4 and MDR
2017/745.
Graft Material
The graft material used was the BIOBank viral-inactivated cancellous bone allograft powder processed by the supercritical CO2 technology. The allografts were prepared from living donor femoral heads treated by the supercritical CO2 process through degreasing steps and a gentle chemical oxidation of the residual proteins with preserved bone architecture. Before sinus filling, the bone allograft powder drawn from the cleaned femoral head and packed in syringe or vial was hydrated using Metronidazole 0.5% solution (B-Braun).
Surgical Technique
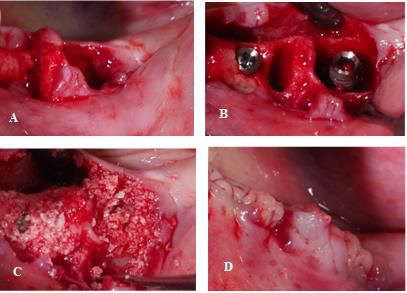
All the surgical procedures were performed by the same surgeon. Sulcular incision and syndesmotomy were made using a blade knife 15 (Swann Morton) followed by atraumatic tooth extraction, with minimal intervention on soft tissues and preservation of the vestibular bone table. A careful alveolar curettage was made to remove all soft tissues and possible granulation and if necessary, rinse with Betadine® in case of infectious site. The bone wall integrity was checked. Crestal drilling, was then carried out according to pre-implant analysis. The drilling extends beyond the alveola to optimize the primary stability of the implant. In the event of an apical lesion, drilling is carried out beyond this lesion to remove the infected tissue and seek reliable anchorage in a healthy tissue. The implant was screwed with an insertion torque of 50 N.cm. Periimplant filling was performed with the cancellous allogeneic bone powder. PRF membranes were placed to cover the ridge and the extraction site to ensure graft stabilization before hermetic closure using resorbable sutures (Covidien-Biosyn Resorbable SuturesTM- 4-0) (Figure 1).
Patients then received the following prophylactic medication: antibiotic therapy consisting of 2g of amoxicillin-clavulanic acid for two to three days before surgery and six days post-surgery; anti-inflammatory coverage with Cortisone for three days, paracetamol codeine analgesic and local care with mouthwashes using Chlorhexidine gluconate Solution and Parodium healing gel. All patients were assessed preoperatively to determine both their dental and general health status, and the following assessments were performed at the post grafting visits:
Outcome Measures
Implant survival defined as:
- The implant is present, functional, and stable.
- No radiolucencies areas around the implant.
- No persistent and/or irreversible subjective and objective
clinical signs (suppuration or pain).
Any complications such as chronic pain, infection.
Figure 1:
A) Extraction of teeth n°36 and 37.
B) Implants placed in positions 36 and 37.
C) BIOBank bone allograft packed into the extraction socket.
D) Ridge and extraction sites covered with PRF membranes.
Radiographic Analysis
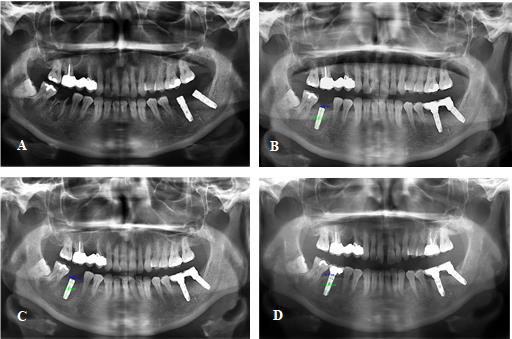
Radiographic analysis was performed using cone-beam computed tomography (CBCT) and/or panoramic radiographs taken before and after grafting and at long-term follow up (Figure 2). Software programs were used to calculate bone height in millimetres (Planmeca Romexis® 2D and 3D images viewer, Planmeca Oy, Asentajankatu 6, Helsinki, Finland). Linear marginal peri-implant bone loss around the implant was measured at the mesial and distal levels (mean value) (Figure 2B, 2C & 2D).
Figure 2:
A) Preoperative panoramic radiography showing the extraction socket position 46.
B) Postoperative panoramic radiography showing the augmented ridge of 2.6 mm measured at implant position 26.
C) 6-month postoperative panoramic radiography showing augmented ridge of 2.1mm (mesial) and 1.8 mm (distal) measured
at implant position 26.
D) 9-year postoperative panoramic radiography showing evidence of osseointegration of implants 26. The peri-implant
marginal bone loss measured at the mesial and distal levels of implant 26 was 0 and -0.5 mm, respectively.
Statistical Analysis
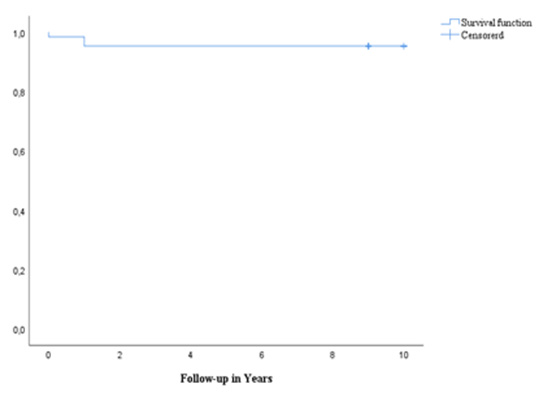
Statistical analyses were carried out in IBM SPSS Statistics 26 (SPSS Inc. Chicago, USA). All included cases were reviewed, and the summary statistics were analyzed as means (standard deviations) for continuous variables and percentages for categorial variables. Cumulative survival rate was calculated using the Kaplan-Meir method.
Results
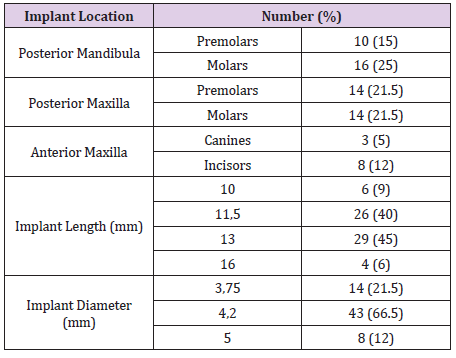
Fifty patients, 29 females and 21 males, with a mean age of 55.5 years (ranged 28 to 75 years) were included in the same centre and underwent tooth extraction. The reason for extraction was mainly due to peri apical dental cyst (62%), dental decay (26%) and furcation defect (12%). All the patients received the supercritical CO2 processed cancellous bone allograft. A mean of 0.8 cm3 of graft was placed (range: 0.25 to 1.5 cm3). No patients were smokers. Demographic details are provided in Table 1. In total, 65 implants were inserted simultaneously to the grafting procedure. Implants were placed mainly in the posterior maxilla and were most frequently 13 mm in length and 4.2 mm in diameter (Table 2).
No complications were recorded during surgery. All the implants displayed primary stability with an average torque of 50 N-cm, regardless of their design, diameter, and length. The mean follow-up from the graft surgery was 9.7 years (range: 9 to 10 years). During this period, 1 peri-implantitis with pain was reported 10 years post-surgery with no consequences for the implant stability. Radiologic results showed mean marginal bone loss of 2.8 mm (range: 0 to 8.8 mm) at immediate post-op, 1.9 mm (range: -2.4 to 8.3 mm) at 6 months follow-up and 0.5 mm (range: -1.9 to 3.4 mm) at 10 years follow-up. At a mean of 9.7 years from the graft surgery, 62 implants (95.4%) were well osseointegrated and functioning. A total of 3 implants (4.6%) failed due to non-osteointegration and were removed: 1 implant failed at 6 months post-surgery for unknown reason; 1 implant failed at 8 months post-surgery due to repeated mucous support of temporary dental equipment leading to non-consolidation; 1 implant failed 9 months post- surgery due to mechanical stress on the screw after immediate loading. The overall implant 10-year survival rate was 95.4% (CI: 90.3 to 100%) (Figure 3).
Discussion
Tooth extraction frequently results in the loss of alveolar bone height and width. A socket filling with bone graft is recommended after a dental extraction to compensate for the lack of volume and optimize functional results [10-13]. Various bone graft materials with osteoinductive and/or osteoconductive properties are used to preserve the alveolar ridge after extraction and to speed up the healing process. Autogenous bone grafts are still thought to be an ideal regenerative material. However, their availability is limited, and the morbidity associated with the second surgical site is significant [14]. Among the alternatives to autografts, allogenic bone use has demonstrated that bone allografts are a suitable alternative in terms of implant osteointegration, bone neoformation, and bone quality. The bone allografts used in this study were derived entirely from living donors’ femoral heads, which were collected after hip replacement surgery and processed using supercritical CO2 extraction technology. The supercritical CO2 process, which is widely used in the pharmaceutical and food industries for the splitting, extraction, and decontamination of organic materials, is a combination of a supercritical CO2 degreasing step and a gentle chemical oxidation of the bone network’s residual proteins. Preclinical studies have shown that this process used on bone has neutral effects on the bone tissue composition; preserves its architecture and mechanical properties, particularly its high wettability, and thus improves performance [15-17].
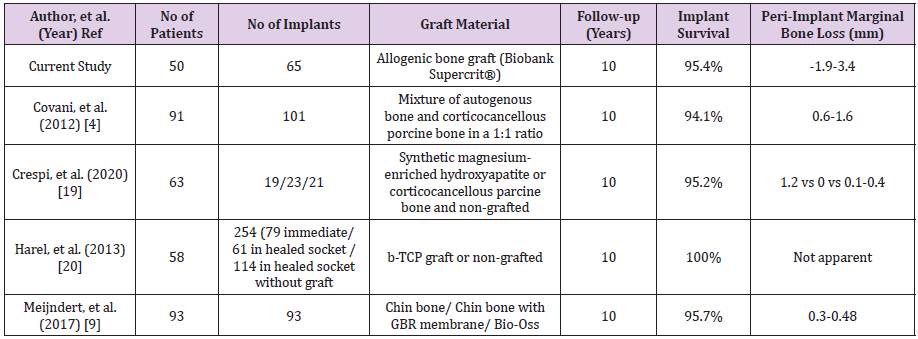
The current study sought to document the long-term clinical and radiological outcomes of implants placed immediately in sockets preserved with supercritical CO2 viral-inactivated bone allograft. Although immediate implant placement in fresh sockets with bone filling is a difficult technique [18], it has several advantages: Reducing soft tissue handling to improve aesthetic results, limiting hard tissue resorption, providing adequate bone volume, optimizing healing through vascular intake, reducing the number of interventions, and shortening treatment time. Dehiscence of the wound, intraoperative or postoperative hemorrhage, infection, graft resorption, and loss of the graft or implants are all risks and complications. There were no perioperative complications reported in this study. One case of peri-implantitis with pain occurred ten years after surgery, with no effect on implant stability. At a 10-year follow-up, the average marginal bone level was 0.2 mm. Over a 10- year period, the mean implant survival rate with the supercritical CO2 viral-inactivated bone allograft was 95.4 percent, which was comparable to the mean 10-year survival rates of 94 percent to 100 percent reported in the scientific literature for autogenous bone graft, a mixture of autogenous bone graft and bone substitutes, or bone substitutes alone (Table 3) [4,9,19,20].
Conclusion
The clinical and radiographic results of the current study using the supercritical CO2 viral-inactivated bone allograft confirm the material’s long-term osseointegration, which is consistent with other graft materials reported in the literature.
References
- Gomes KU, Carlini JL, Biron C, Rapoport A, Dedivitis RA (2008) Use of Allogeneic Bone Graft in Maxillary Reconstruction for Installation of Dental Implants. J. Oral Maxillofac. Surg 66(11): 2335-2338.
- Viscioni A, Franco M, Paolin A, Cogliati E, Callegari M, et al. (2011) Effectiveness of fresh frozen and cryopreserved homologue iliac crest grafts used in sinus lifting: A comparative study. Cell Tissue Bank 12(4): 263-271.
- Xavier, S, Silva E, Kahn A, Chaushu L, Chaushu G (2015) Maxillary Sinus Grafting with Autograft Versus Fresh-Frozen Allograft: A Split-Mouth Evaluation of Bone Volume Dynamics. Int J Oral Maxillofac Implants 30(5): 1137-1142.
- Covani U, Chiappe G, Bosco M, Orlando B, Quaranta A, et al. (2012) A 10-Year Evaluation of Implants Placed in Fresh Extraction Sockets: A Prospective Cohort Study. J Periodontol 83(10): 1226-1234.
- Polizzi G, Grunder U, Goené R, Hatano N, Henry P, et al. (2000) Immediate and delayed implant placement into extraction sockets: A 5-year report. Clin Implant Dent Relat Res 2(2): 93-99.
- Huys LW (2001) Replacement Therapy and the Immediate Post-Extraction Dental Implant. Implant Dent 10(2): 93-102.
- Schwartz Arad D, Chaushu G (1997) Placement of Implants into Fresh Extraction Sites: 4 to 7 Years Retrospective Evaluation of 95 Immediate Implants. J Periodontol 68(11): 1110-1116.
- Kuchler U, Chappuis V, Gruber R, Lang NP, Salvi GE (2016) Immediate implant placement with simultaneous guided bone regeneration in the esthetic zone: 10-year clinical and radiographic outcomes. Clin Oral Implants Res 27(2): 253-257.
- Meijndert CM, Raghoebar GM, Meijndert L, Stellingsma K, Vissink A, et al. (2017) Single implants in the aesthetic region preceded by local ridge augmentation; a 10-year randomized controlled trial. Clin Oral Implants Res 28(4): 388-395.
- Maiorana C, Poli PP, Deflorian M, Testori T, Mandelli F, et al. (2017) Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix. J Periodontal Implant Sci 47(4): 194-210.
- Barone A, Orlando B, Cingano L, Marconcini S, Derchi G, et al. (2012) A randomized clinical trial to evaluate and compare implants placed in augmented versus non-augmented extraction sockets: 3-year results. J Periodontol 83(7): 836-846.
- Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, et al. (2012) Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res 23 Suppl 5: 22-38.
- Allegrini S, Koening B, Allegrini MRF, Yoshimoto M, Gedrange T, et al. (2008) Alveolar ridge sockets preservation with bone grafting--review. Ann Acad Med Stetin 54(1): 70-81.
- Barone A, Ricci M, Mangano F, Covani U (2011) Morbidity associated with iliac crest harvesting in the treatment of maxillary and mandibular atrophies: a 10-year analysis. J Oral Maxillofac Surg 69(9): 2298-2304.
- Frayssinet P, Rouquet N, Mathon D, Autefage A, Fages, J (1998) Histological integration of allogeneic cancellous bone tissue treated by supercritical CO2 implanted in sheep bones. Biomaterial 19(24): 2247-2253.
- Mitton, D, Rappeneau J, Bardonnet R (2005) Effect of a supercritical CO2 based treatment on mechanical properties of human cancellous bone. Eur J Orthop Surg Traumatol 15(4): 264-269.
- Vastel L, Masse C, Mesnil P, Crozier E, Padilla F, et al. (2009) Comparative ultrasound evaluation of human trabecular bone graft properties after treatment with different sterilization procedures. J Biomed Mater Res B Appl Biomater 90(1): 430-437.
- Ortega Martínez J, Pérez Pascual T, Mareque Bueno S, Hernández Alfaro F, Ferrés Padró E (2012) Immediate implants following tooth extraction. A systematic review. Med Oral Patol Oral Cir Bucal 17(2): 251-261.
- Crespi R, Toti P, Covani U, Crespi G, Brevi B, et al. (2020) Bone Assessment in Grafted and Ungrafted Sockets After Dental Implant Placement: A 10-year Follow-up Study. Int J Oral Maxillofac Implants 35(3): 576-584.
- Harel N, Moses O, Palti A, Ormianer Z (2013) Long-Term Results of Implants Immediately Placed into Extraction Sockets Grafted With b-Tricalcium Phosphate: A Retrospective Study. J Oral Maxillofac Surg 71(2): e63-68.

 Research Article
Research Article