Abstract
Purpose: Light disturbances are common sources of complains in pseudophakic patients with multifocal contact lenses. The purpose of this study was to evaluate the changes in visual performance of patients bilaterally implanted with multifocal intraocular lenses (IOLs) after cataract extraction or refractive lens exchange using new metrics of visual performance under reduced illumination conditions.
Methods: A total of 57 patients were enrolled in this prospective case series and followed for 6 months after binocular implantation of multifocal IOLs. Light disturbances resulting from halo, starburst and glare were evaluated in a dark room with a prototype under monocular and binocular conditions. Subjective quality of vision was also assessed with the Quality of Vision (QoV) questionnaire as scores of Frequency, Severity and Bothersome from 0 to 100. Evaluations were scheduled at 1, 3 and 6 months after surgery in the second eye.
Results: Main outcome measures included objective and subjective measures of light disturbances.Light disturbance index decreased from 39±16% at 1 month to 35±15% at 6 months visit (p=0.043). QoV scores decreased from 49±16 to 43±12 from 1 to 6 months (p=0.008); bothersome decreased more significantly from 37±19 to 21±17 from 1 to 6 months (p<0.001).
Conclusion: In spite of a stable near, intermediate and distance performance over the post-operative period, symptoms and objective metrics of visual performance under dim illumination conditions improved from 1 to 6 months particularly for the subjective perception of bothersome.
Keywords: Cataract; Pseudophakia; Multifocal IOL; Dysphotopsias; Quality of Vision
Introduction
Cataract extraction with implantation of intra-ocular lenses (IOL) has become a routine procedure since the third quarter of the past century. As a result of the advances in lens design, biometric methods and intra-ocular lens calculation, implantation of multifocal, toric and multifocal toric [1,2] intra-ocular lenses (MIOLs) has become increasingly common in patients with clear lens and with cataract opening the era of the so called Premium intraocular surgery. Despite high levels of success in emmetropizing the eye and providing near and distance vision, multifocal IOLs have been under scrutiny due to frequent complains of dysphotoptic phenomena. These physical phenomena are originated by the different power of the IOL across the pupil area and formation of different foci at different distances in front of the retina, are more noticeable under dim light conditions (i.e. bright lights against dark backgrounds) and in some cases justify explantation of the IOL. Most of the reports of visual complains are based on subjective questionnaires but it has not been until recently that the quantification of these phenomena has become an objective and quantifiable examination. Pieh [3] was the first to report an objective measure of the increased disturbance originated by a multifocal IOL compared to a monofocal IOL. Since them, the first systematic reports were more frequent as the implantation of these devices increased over the last 5 to 10 years using devices called halometers or light disturbance analyzers [4-6]. Nowadays is possible to quantify the effects of the light disturbances, and more importantly follow-up patients and record changes overtime.
In preliminary studies conducted by this group, we have been able to proof that one prototype analyzer (Light Disturbance Analyzer or LDA) is able to differentiate the size, shape and regularity of disturbances induced by different intra-ocular devices [5,7,8]. This devices also open the opportunity to evaluate potential adaptation phenomena overtime to corroborate clinical observations, and eventually contributing with new information for the management of the patients implanted. This might be of particular relevance for presbyopic patients undergoing clear lens extraction with implantation of MFIOLs as this patients are younger and typically have higher expectations on their procedure. In a recent work conducted by the authors, we have observed that in patients undergoing clear lens extraction, visual performance improved between 1 to 3 months after surgery. Furthermore, were identified pre-operative parameters that predicted this improvement after surgery [9]. However, some authors suggest that the adaptation to multifocality after surgery will occur after 4 months of surgery, [10] and therefore we might have been not able to identify further improvements with that short follow-up.
Therefore, the present study was designed to test the hypothesis that there is a significant improvement in the medium term from 1, through 3 and 6 months in the objective perception of light disturbances measured with a light disturbance analyzer, and the subjective perception obtained with a quality of vision questionnaire. The main purpose of this study was to evaluate if there are any short-term changes in visual function and dysphotopsias, reported subjectively and measured objectively, under low illumination conditions in cataract or RLE presbyopic patients implanted with multifocal intraocular lenses. A secondary goal was to evaluate if there are parameters measured in the shortterm post-operative examination (1 month) that might predict the improvement occurring in the medium term at 3 and 6 months.
Material and Methods
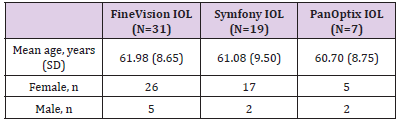
This study was conducted at Hospital da Luz, Lisbon. The protocol was approved by the Ethics Committee of the Hospital and the research was settled in collaboration with the Clinical and Experimental Research Laboratory (CEORLab) at University of Minho in Braga, Portugal. The principles of Good Clinical Practice were adhered to throughout in accordance with the Declaration of Helsinki. A prospective longitudinal not masked study was conducted in consecutive candidates to sequential bilateral cataract surgery or refractive lens exchange from April 2015 to February 2016 ending the follow up in September 2016. Postoperative outcomes were assessed 1, 3 and 6 months after second eye surgery. Before data collection patients were instructed on the purpose of the study and procedures used, and signed a consent form before formal enrollment. A total of 57 eligible patients (48 females and 9 males) aged 42 to 79 years (mean 61.53±8.92 years) were identified by participating surgeon at their preoperative assessment, given an explanation of the study and its aims and detailed information to be comprehensible to a non-expert person.
The main inclusion criteria were motivation, ability to return for follow-up up to 6 months post-surgery and ability to sign the informed consent. Exclusion criteria included amblyopia, glaucoma history, corneal disease, previous corneal or intraocular surgery, severe dry eye, abnormalities of iris or pupil disability, retinal pathology or history of ocular inflammation, post-op refractive error higher than ±0.50 and unaided post-op visual acuity below 0.10 logMAR or worse. Also was required that patients had not been subjected to additional secondary refractive procedures prior or after IOL implantation. Our study was powered to have 80% chance of detecting a 10 unit change in quality of vision symptoms after bilateral multifocal IOL implantation using significance threshold set at P<0.017 considering the multiple comparisons over the 3 follow-up visits. The null hypothesis was that symptoms would not change over the follow-up period. By allowing for 10% patient dropout, a recruitment target of 40 patients in total was set. This power analysis is based on background data from a previous study8 considering a mean score in subjective QoV of 45 ±15 to detect a variation of 15 units in score using the same methodological procedures.
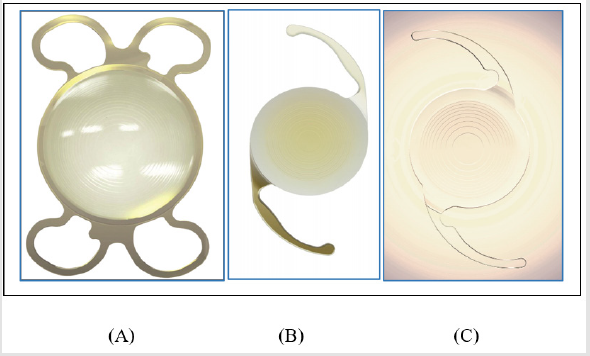
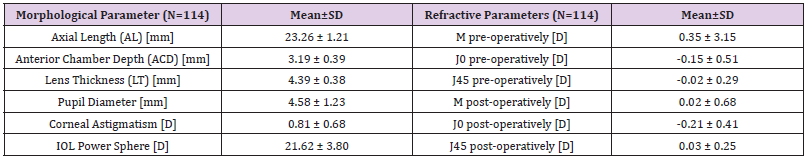
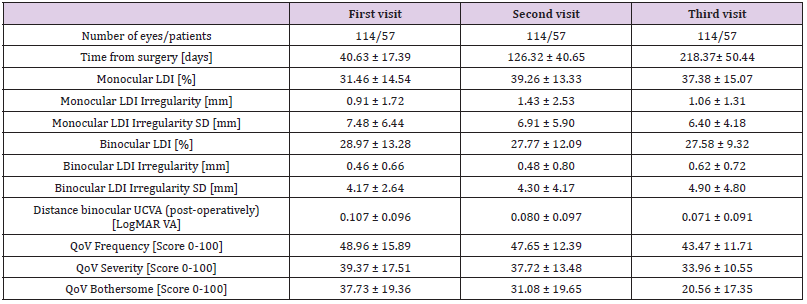
Prior to surgery, a comprehensive ophthalmologic examination was performed, including manifest and cycloplegic refraction, keratometry, corneal topography to assess preoperative astigmatism, slit–lamp biomicroscopy, Goldmann applanation tonometry, and dilated fundal examination. Surgical procedures were conducted by the same experienced surgeon (F.J.R.) under local anesthesia through a microincision of 2.2mm. Ophthalmological examination also included optical biometry and anterior surface optical tomography for the calculation of the power of the IOL using a semi-customized ray tracing method [11]. Optical biometry was performed with the Lenstar LS 900 (Haag-Streit AG, Koeniz, Switzerland) and anterior surface optical tomography with the Orbscan Topography System II (Orbscan, Inc., Salt Lake City, UT, USA). The targeted refraction was emmetropia in both eyes. All biometry was carried out by a single, experienced ophthalmic technician. Surgical procedures with IOL implantation were conducted with a difference of 7 days between eyes. Phacoemulsification was followed by irrigation and aspiration of the cortex and IOL implantation in the capsular bag. All the procedures were uneventful, and none of the patients had any significant intraoperative complications. Multifocal IOLs implanted were trifocal lenses and extended depth of focus (EDoF). Trifocal lenses were FineVision® Pod F (PhysIOL, Liège, BE) and AcrySof® IQ PanOptixTM (TFNT00) (Alcon Laboratories, Fort Worth, Texas, USA) and EDoF lenses were TECNIS® Symfony model ZXR00 (Abbott Medical Optics, Santa Ana, USA) (Figure 1). In total, 38 patients were implanted with trifocal lenses (19 FineVision and 7 PanOptix) and 19 patients were implanted with Symfony effecting a total sample of 57 patients. Baseline characteristics of sample is shown in Table 1.
Figure 1:Figures showing the different implants used:
A. Trifocal FineVision
B. Extended depth of focus Symfony
C. Trifocal PanOptix.
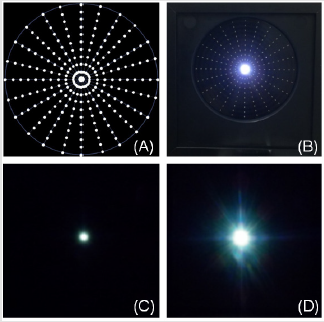
Main outcome measures will be the binocular high contrast visual acuity (VA) for different levels of defocus from +1.00 to -3.00 in 0.50 steps, contrast sensitivity function (CSF) for 1.5, 3.0, 6.0, 12.0 and 18.0 cycles per degree (cpd) without and with glare at 28 lux, subjective quality of vision (QoV) questionnaire [12] and light distortion (LD) analysis for size, shape and regularity of the halo surrounding a source of glare [4,13]. All measures were done 1, 3, and 6 months after second eye surgery. The examiner was not masked to the lens type and binocular defocus curves were measured with no correction. Light distortion was analyzed with an experimental prototype, the Light Distortion Analyzer (CEORLab, University of Minho, Portugal), which consists of a central light source (LED) surrounded by 240 small LED sources distributed in 24 semi-meridians with an angular separation of 15º (Figure 2). Characteristics of the device, examination routines and main outcome measures have been previously described and validated in clinical populations [13,14] including pseudophakic patients [4,7]. Statistical analysis was conducted using SPSS for Windows software (version 22, SPSS, Inc.). Analyses include descriptive data for patient demographics and visual and refractive outcomes. The results on VA and contrast sensitivity are reported as binocular outcomes. Normality of data distribution was assessed using the Shapiro-Wilk test. One-way analysis of variance (ANOVA) were used for parametric data with a post hoc Bonferroni test or Kruskal-Wallis with multiple post-hoc comparisons was used to compare the results between assessed moments. Correlations were assessed using Pearson Correlation or non-parametric Spearman correlation. For all statistical analyses the level of significance was a P value was lower than 0.05. Multiple post-hoc comparisons were considered significant when P value was under 0.05/3 = 0.017
Figure 2:A. Distribution of the main central light source and smaller peripheral light stimuli in accordance with the display used in the prototype light-distortion analyzer
B. Actual appearance of the LED hardware with the central glare source and one peripheral stimuli (5th circle at 30º) turned-on
C. Central glare source presented in total darkness displaying very small distortion
D. Central glare source presented in total darkness displaying large distortion.
Results
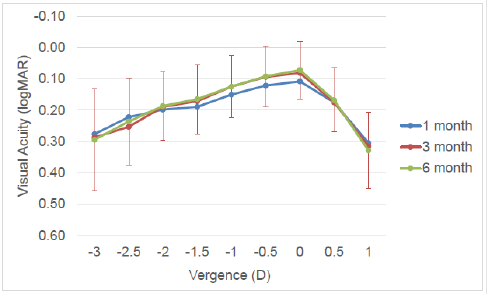
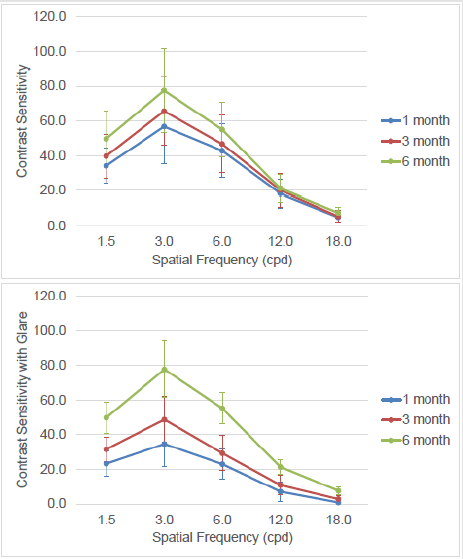
A total of 57 patients were recruited and followed for 6 to 8 months after cataract extraction with binocular implantation of multifocal IOLs. Nineteen of them received an extended depthof- focus (EDoF) IOL and thirty-eight received a trifocal IOL. Table 2 shows the demographic data. Examinations were performed at 40±17 days (1.35 months), 126±41 days (4.21 months) and 218±50 days (7.28 months) after surgery. Main outcomes in each examination are shown in Table 3. Visual performance measured with high contrast visual acuity at distance and at different vergences (defocus curves) did not change significantly over the follow-up period after surgery. None of the parameters measured showed statistically significant changes in the short and mediumterm after surgery (p>0.05, Kruskal-Wallis test) (Figure 3). Despite the stable visual performance under habitual clinical metrics (high contrast acuity at different distances), contrast sensitivity function showed a significant improvement in the low and medium spatial frequencies. Contrast sensitivity without and with glare improved significantly from 1 to 6 months for 1.5, 3.0 and 6.0 spatial frequencies. These differences were statistically significant (p<0.008) when comparing 1 month with 3 and 6 months, but not when compared 3 months with 6 months results as shown in Figure 4.
Figure 3:Defocus curves as logMAR units for each vergence at 1, 3 and 6 month visits. Error bars reporting 1xSD are only included for the 3 month visit for clarity.
Figure 4:Contrast sensitivity function under normal photopic (top) and mesopic with glare (bottom) at 1, 3 and 6 month visits. Error bars represent 1xSD.
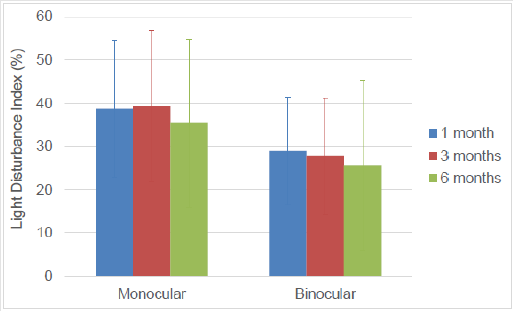
Figure 5:Light disturbance index (%) under monocular and binocular conditions at 1, 3 and 6 months visits. Error bars represent 1xSD.
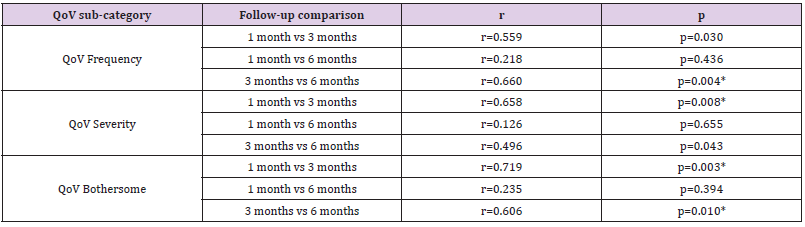
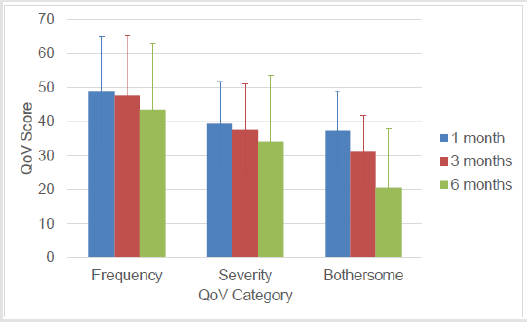
Light disturbance index decreased from 39±16% at 1 moth to 35±15% at 6 months visit (p=0.043). Despite this small reduction overtime from 1 to 6 months, the most remarkable finding is the increased binocular summation observed from 1 month (binocular LDI 25% smaller than monocular value) to 3 and 6 months (28 to 30% reduction in binocular LDI compared to monocular) (Figure 5). Results of the QoV questionnaire showed a decrease from 49±16 to 43±12 from 1 to 6 months (p=0.008); Bothersome showed the more remarkable decrease from 37±19 at 1 month to 21±17 at 6 months (p<0.001) (Figure 6). The larger improvement occurred indeed from the month 3 to month 6 (-10.5±14.7, post-hoc pair-wise correction p<0.001) compared to the reduction from 1 to 3 month (-6.2±16.6, post-hoc pair-wise correction p=0.006). To explore the correlation between QoV subcategory scores at different times over the follow-up correlations were produced and presented in Table 4. We assume that the stronger correlations suggest that we can predict the results in the medium term (i.e. 3 or 6 months) from the short-term (1 month) follow-up visits.
Figure 6:Quality of vision scores for frequency, severity and bothersome at 1, 3 and 6 months follow-up visits. Error bars represent 1xSD.
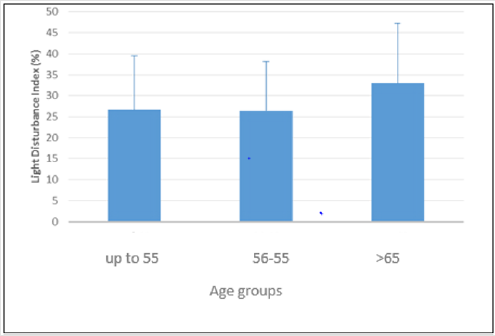
Figure 7:Light disturbance index (%) under binocular conditions at 6 months visit by age group. Error bars represent 1xSD.
Correlation analysis revealed that age was not a significant parameter influencing other visual functions in this study at any point in the follow-up (1, 3 or 6 months). Visual acuity at distance (vergence 0.00 D) was significantly correlated with acuity at all the remaining vergences (Rho=0.500 to 0.800, P>0.008) at all follow-up visits (1, 3 and 6 months). Contrast sensitivity and light disturbance index were negatively correlated at the 6 months visit for the photopic condition without glare and for 3, 6, 12 and 18 cycles per degree frequencies (Rho=-0.370 to -0.471; p<0.005) and for the mesopic condition with glare for 1.5, 6.0, 12.0 and 18.0 cpd frequencies (Rho=-0.383 to -0.457; p<0.003). Such correlations were somewhat present also at the 3 and 1 month visits but were weaker and present in fewer spatial frequencies. Despite age was not determinant when correlated with other visual metrics, light disturbance index in older patients was moderately higher. Indeed, when sample was divided in three groups by age, until 55 years, between 56 and 65 years, and more than 65 years, binocular LDI parameter measured at six months was 26.67±12.86, 26.43±11.78 and 33.07±14.22 respectively (Figure 7).
Discussion
This study investigated visual performance after bilateral multifocal IOLs implantation over a minimum of 6 months follow-up with new methods and metrics to better understand visual behavior, eventual complaints under dim illumination and their evolution in time. Present research is the first study to quantify visual symptoms after multifocal IOL implantation using in the routine protocol at 1, 3 and 6 months a QoV psychometric questionnaire related to dysphotopsias complaints and an objective method to assess light disturbances under dim illumination conditions besides the classic metrics to analyze visual outcomes after implant-refractive surgery like defocus curves (VA) and contrast sensitivity function measured also under presence of a source of disability glare in dark conditions. In the present research it is observed that in the short (1 to 3 months) and medium term (3 to 6 months) after surgery there is a continuous, thought non-linear improvement in visual performance with implantation of multifocal IOLs after cataract and clear lens extraction. This improvement is not present in common clinical tests such as high contrast visual acuity. Indeed, defocus curves showed to remain stable overtime. Other objective parameters such as the light disturbance index, did not change significantly overtime in the present study suggesting that the dysphotopsias arising from multifocal IOL implantation remain present in the short and medium term after surgery. In fact, light disturbance values are above the values observed in patients implanted with monofocal IOLs in cataract patients [4,7,8].
This is in agreement with the expected optical effect that is inherent to the design of the IOLs. More interestingly, other aspects perhaps related with perceptual issues have demonstrated a change over the 6 months follow-up period. This has been the case of subjective quality of vision score. Indeed, while patients report that frequency and severity of symptoms remain quite stable, in line with the dysphotopsia measurements, “bothersome” sub-category has been the one with the stronger reduction over the follow-up period. This suggests to us that while the photic phenomena are still present and quite stable as demonstrated objectively by LDA instrument, patients start reducing their concerns about this in the medium term. This is in agreement with authors that reported an improvement in their results 4 months after surgery. At the same time, contrast sensitivity showed a marked trend to improve in the medium-term at 3 and 6 months after surgery compared to 1 month. This enhances our hypothesis of a perceptual change overtime. Furthermore, the trend for contrast sensitivity and light disturbance to be more correlated in the longer term is also an interesting finding of this study. This negative correlation, means that the larger the light disturbance, the lower the contrast sensitivity values and vice-versa. We understand that both parameters might reflect different aspects of visual performance, and they are also measured under different conditions. However, we interpret this finding as an improvement of the visual perception of patients in the medium term that might affect both functions. It has been previously demonstrated that multifocal IOL devices decrease the contrast sensitivity function in the short term, with a trend towards recovery in the medium and longer term. In our previous study with younger presbyopic patients undergoing clear lens extraction, we observed such drop in the short term and a trend towards improvement after 3 months [9].
In the present study, we have observed a further improvement in the medium term at 6 month visit, particularly in the low and medium frequencies. This is in agreement with other studies [15,16]. Such improvement in CSF has been attributed to a perception change derived from the new conditions of viewing under more challenging conditions as a consequence of new distribution of light across different foci. If this is the case, it might also have a consequence in the performance of the patient under the light disturbance analysis conditions. A stronger perception might also be reflected as an increased ability (absolute or relative) in the medium-term after surgery as it has been the case in the present study and render lower values of LDI parameter. Changes in contrast sensitivity function between the third (6 months) and first visit (1 month) do not depend on either the age of patients or the type of implanted lens, either EDoF or trifocal (Kruskal-Wallis test, p>0,05). Although of very modest values, the correlations calculations revealed a slight negative correlation between the age and the bothersome variable at 3 and 6 months after the surgery, that is to say, at a younger age, more medium-term complaints regarding vision dysphotopsias would appear.
We could hypothesized that the younger patients, with a more active and visually challenging life, could have high expectations with the outcomes after the surgery, although the age in our population is relatively homogeneous. It would be interesting to evaluate this relationship in populations with different ages in further research. Age is also well correlated with contrast sensitivity function especially in under night conditions with glare, which is agree with previous studies related with this physiological variation in such visual performance metric. It seems that at 6 months to the older group (over 65 years) are less uncomfortable than the younger ones (less than 65 years), perhaps because of the expectations generated, although there are no significant differences in the variation of the QoV parameters related to the age range in which the patients are. Two major limitations are present in our study. The first one is related with the indication for surgery, with cataract and clear lens patients being mixed. Despite this, we do not believe that this makes a significant different in our outcomes as the age of our patients was within a quite narrow range with 68.42% of patients within a range of 45 to 65 years of age. The second one is related with the different lenses implanted, being trifocal and extended range of focus IOLs. However, our previous studies showed that with the exception of defocus performance at vergences from 2.00 to 3.00, is not expected that patients perform significantly different with them and present similar symptoms Overall, levels of overall satisfaction related to vision at near, medium and far distance were generally high. But visual symptoms quantified, both objective and subjectively, 1 to 6 months after surgery, and halo in particular, were more bothersome for recipients of these contemporary multifocal lenses at the beginning of follow-up having a tendency to attenuate in bothersome at stage of 6 months after second eye surgery.
Although the association between IOL optic performance and visual symptoms could have been examined in a pure context by systematically correcting all remaining refractive error, this would not reproduce IOL performance in the real world. There is no a correspondence between visual symptoms and spectacle freedom for patients receiving multifocal IOL implantation although subjective complaints have a tendency to decrease in the medium term around 6 months after the intervention which confer reasonable levels of satisfaction in patients, although not always their expectations are fulfilled in relation to the absence of complaints of night vision, and confidence to surgeons who implant such novel devices. What needs to be investigated further is whether or not neuroadaptation process in retina or in superior level of vision exist. The unknown element is the patient’s ability to adapt to the new retinal image, and a small proportion of patients will always experience persistent photic phenomena. Although visual complaints such as glare and halos often subside as the patient neurally adapts, it is not always possible to predict which patients will report symptoms. We strongly suggest new studies to investigate the impact in retina of multifocal optics induced by novel IOLs. An electrophysiological approach could better understand what happens when a new optics is used trying to compensate accommodation failure due to presbyopia.
Funding
This study has been funded in part Portuguese Foundation for Science and Technology (FCT) in the framework of projects PTDC/ SAU-BEB/098391/2008, PTDC/SAU-BEB/098392/2008 and the Strategic Funding UID/FIS/04650/2013.
Acknowledgement and Disclosure
JMGM is co-inventor in patent application involving one experimental device used in this study. Remaining Authors do not have any financial interest in the methods used in the study. This study has been funded in part Portuguese Foundation for Science and Technology (FCT) in the framework of projects PTDC/ SAU-BEB/098391/2008, PTDC/SAU-BEB/098392/2008 and the Strategic Funding UID/FIS/04650/2013.
References
- Escandón-García S, Ribeiro FJ, McAlinden C, González-Méijome JM (2018) Through-focus and night vision clinical performance of 3 new intraocular lenses for presbyopia correction. Ournal of ophthalmology, p. 1-8.
- Escandón-García S, Ribeiro FJ, McAlinden C, González-Méijome JM. Visual performance, effect of glare and binocular summation with monofocal, EDoF and trifocal toric IOLs: pilot study.
- Pieh S, Lackner B, Hanselmayer G, Zöhrer R, Sticker M, et al. (2001) Halo size under distance and near conditions in refractive multifocal intraocular lenses. Br J Ophthalmol 85(7): 816-821.
- Brito P, Salgado-Borges J, Neves H, Gonzalez-Meijome J, Monteiro M (2015) Light-distortion analysis as a possible indicator of visual quality after refractive lens exchange with diffractive multifocal intraocular lenses. J Cataract Refract Surg 41(3): 613-622.
- Sheppard AL, Shah S, Bhatt U, Bhogal G, Wolffsohn JS (2013) Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg 39(3): 343-349.
- Puell MC, Pérez-Carrasco MJ, Hurtado-Ceña FJ, Álvarez-Rementería L (2015) Disk halo size measured in individuals with monofocal versus diffractive multifocal intraocular lenses. J Cataract Refract Surg 41(11): 2417-2423.
- Salgado-Borges J, Dias L, Costa J, Ferreira-Neves HI, Peixoto-de-Matos SC, et al. (2015) Light distortion and ocular scattering with glistening and aberration-free pseudophakic IOL: Pilot Study. J Emmetropia 6(3): 127-132.
- Escandón-García S, Ribeiro FJ, McAlinden C, González-Méijome JM. Light distortion and contrast sensitivity function in pseudophakic population implanted with monofocal and multifocal IOLs.
- Escandón-García S, Ribeiro FJ, McAlinden C, González-Méijome JM. Light distortion as an indicator of adaptation to multifocality after refractive lens exchange (RLE).
- Braga-Mele R, Chang D, Dewey S, Foster G, Henderson BA, et al. (2014) Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg 40(2): 313-322.
- Ribeiro FJ, Castanheira-Dinis A, Dias JM (2012) Personalized pseudophakic model for refractive assessment. PLoS ONE 7(10): e46780.
- McAlinden C, Pesudovs K, Moore JE (2010) The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci 51(11): 5537-5545.
- Ferreira-Neves H, Macedo-de-Araújo R, Rico-del-Viejo L, Silva AC, Queirós A, et al. (2015) Validation of a method to measure light distortion surrounding a source of glare. J Biomed Optics 20(7): 75002.
- Linhares JMM, Neves H, Lopes-Ferreira D, Faria-Ribeiro M, Peixoto-de-Matos SC, et al. (2013) Radiometric characterization of a novel led array system for visual assessment. Journal of Modern Optics 60(14): 1136-1144.
- Cochener B (2016) Prospective Clinical Comparison of Patient Outcomes Following Implantation of Trifocal or Bifocal Intraocular Lenses. J Refract Surg 32(3): 146-151.
- Alio JL, Grzybowski A, El Aswad A, Romaniuk D (2014) Refractive lens exchange. Surv Ophthalmol 59(6): 579-598.

 Research Article
Research Article