Abstract
The case of a previously healthy 17-year-old pediatric patient is presented, who is admitted with a history of platelet penia and generalized weakness. Imaging studies show no brain lesions. Given the clinical picture and findings in the hemogram, a peripheral blood smear was performed, confirming the diagnosis of idiopathic thrombocytopenic purpura.
Keywords: Idiopathic Thrombocytopenic Purpura; Pediatrics
Introduction
Thrombotic thrombocytopenic purpura (TTP) also known as Moschcowitz disease, since it was mentioned for the first time by Eli Moschcowitz in 1924, is a disease that is part of thrombotic microangiopathies together with hemolytic uremic syndrome, atypical hemolytic uremic syndrome and microangiopathies of pregnancy [1]. Thrombotic thrombocytopenic purpura is a rare hematologic disorder of immune origin. characterized by microangiopathic hemolytic anemia, thrombocytopenia, fever, renal and neurological involvement. It affects women to a greater extent and has a poor prognosis, with a mortality close to 90% without treatment. It can be acquired or congenital. Its incidence is estimated at 1 to 10 cases per 3.4 million inhabitants [2]. It is mainly caused by the deficiency or malfunction of the ADAMTS13 protein [2]. The basis of its treatment is based on daily plasmapheresis. Although plasmapheresis associated with the use of corticosteroids is the priority treatment [3]. In this article we present the case of a pediatric patient with a diagnosis of idiopathic TTP [3].
Clinical Case
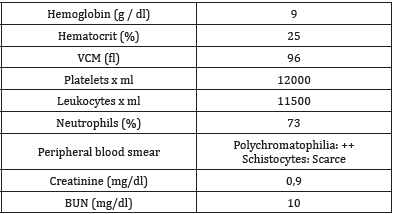
A 17-year-old female patient with a history of plaquetopenia and generalized weakness who was admitted due to a 5-day history of symptoms consisting of asthenia, adynamia, vertigo and headache of mild to moderate intensity. The patient consulted the Rio Grande health center, where a hemogram was performed in which moderate plaquetopenia was documented, for which they were referred to our hospital. Upon admission to our institution, it was documented that he had presented disorientation, without evidence of an infectious clinical focus in the physical examination or alterations in the neurological examination, no focalization, or other abnormalities. Moderate thrombocytopenia anemia is documented in admission paraclinics. Multiple schistocytes are documented in the peripheral blood smear. without impaired renal function (Table 1). Given the data of a patient with non-immune hemolytic anemia classified as microangiopathic due to the presence of schistocytes in peripheral blood, associated with moderate thrombocytopenia, fever and neurological alterations, the diagnosis of thrombocytopenia secondary to idiopathic purple thrombocytopenia is considered, for which ADAMTS 13, which were reported as under 40%. Management was started with methylprednisolone and 2 units of platelets were transfused. Patient who later presented platelet count in 22,000, without alterations in the red line, with manual platelet count in 32,000, without data of active bleeding, without indication of platelet transfusion, for which it was decided to give medical discharge with follow-up for pediatric hematology and management with outpatient methylprednisolone.
Discussion
Idiopathic purple thrombocytopenia, due to the rarity of its presentation, creates a challenge for its diagnosis because its clinical manifestations do not always begin with the known clinical pentad: fever, thrombocytopenia, microangiopathic hemolytic anemia, neurological abnormalities and kidney involvement, making it difficult timely treatment [4]. The case presented shows us an atypical presentation of idiopathic purple thrombocytopenia characterized by the absence of renal involvement and without alterations in the central nervous system, which is usually the most common presentation of the disease, without a triggering cause [5]. In addition, it makes known the importance of establishing a timely therapy with plasmapheresis, which allowed adequate clinical evolution and a favorable prognosis for the patient, which shows that it is essential to recognize the clinic as a valuable element for the diagnostic approach of this disease [6].
References
- Chandan J S, Thomas T, Lee S, Marshall T, Willis B, et al. (2018) The association between idiopathic thrombocytopenic purpura and cardiovascular disease: a retrospective cohort study. Journal of Thrombosis and Haemostasis 16(3): 474-480.
- Oved J H, Lee C S, Bussel J B (2017) Treatment of children with persistent and chronic idiopathic thrombocytopenic purpura: 4 infusions of rituximab and three 4-day cycles of dexamethasone. The Journal of pediatrics 191: 225-231.
- Ou Y, Yang Y, Xiang X, Wu Y (2020) Relationship between the IL-10 (-1082 A/G) polymorphism and the risk of immune/idiopathic thrombocytopenic purpura: A meta-analysis. Cytokine 125: 154820.
- Takase K, Kada A, Iwasaki H, Yoshida I, Sawamura M, et al. (2018) High-Dose dexamethasone therapy as the initial treatment for idiopathic thrombocytopenic purpura: protocol for a multicenter, open-label, single arm trial. Acta Medica Okayama 72(2): 197-201.
- Zhao X, Qi X, Wang C, Zhou Z, Cao H, et al. (2017) Idiopathic thrombocytopenic purpura: pathogenesis and potential therapeutic approach. Minerva médica 108(6): 502-506.
- Hatzistilianou M, Janoudaki M, Massaad M, Geha R, Kanariou M (2019) Idiopathic Thrombocytopenic Purpura. In Pediatric Immunology, Springer, cham, pp. 717-720.

 Case Report
Case Report