Abstract
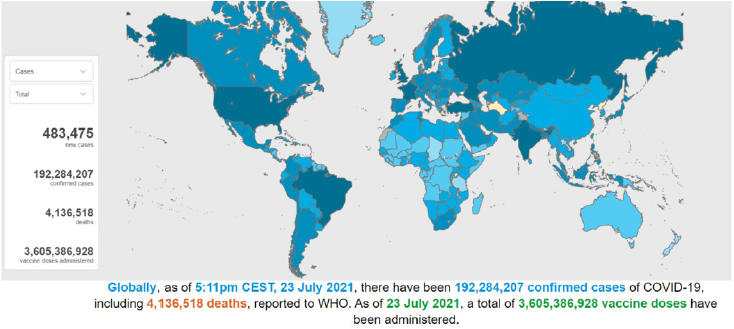
Background: In December 2019 COVID 19 originated in Wuhan, Hubei province, of
China, but as of 23july 2021 >192 million cases and >4 million deaths have been reported
globally. These dramatic figures have a profound, potentially long-lasting and extensive
effect on the delivery of surgical services worldwide.
Objective: Aimed to support surgical teams and health service by identifying key
domains that should be covered in pandemic preparedness plans.
Methods: The data and information is collected from various international journals
and electronic media published throughout the world.
Results: As regions with the highest volume of operations per capita are being hit, a
large number of operations are being postponed. Patients are being deprived of surgeries,
with uncertain loss of function and risk of adverse prognosis as a collateral damage by
the pandemic. No major entity has enlisted the difficulties faced by general public as
conditions for general surgeries are not on par with the ones required. Surgical services
need a backup plan for maintaining surgical care in an ongoing or post pandemic time
phase.
Conclusion: A pandemic is a rapidly changing scenario, requiring reorganization and
teamwork flexibility of the healthcare delivery. In future research required to study the
impact of COVID-19 infection on postoperative outcomes, identifying risk stratification
strategies, and determining whether prophylaxis using anti-COVID drugs and how to
reduces rates of hospital-acquired COVID-19 infection.
Keywords: COVID 19 Pandemic; Surgery
Introduction
Corona virus comprises of a large family coronaviridae sub
family coronavirinae of viruses that infect a large range of hosts
including human beings as well animals (camels, cattle, cats, and
bats).
There are four different strains of corona virus [1].
1. Alpha coronavirus- HCoV-22E and HCoV-NL63 (infect
humans), Pig,Cat,dog CoVs.
2. Beta coronavirus- HCoV-OC43, HCoV-HKU1, MHV,
a) HCoV-SARS (that causes severe acute respiratory syndrome, or
SARS)
b) MERS-CoV(that causes Middle East Respiratory Syndrome, or
MERS)
c) SARS CoV-2(novel coronavirus that causes the coronavirus
disease 2019, or also known as COVID-19)
3. Gamma corona virus-Chicken and turkey CoVs
4. Delta corona virus - Bird CoVs
Sometimes corona virus from animals infects humans and spread further via human to human transmission such as with MERS-CoV, SARS-CoV, and now with this COVID 19 (Corona disease 2019). The virus that causes COVID-19 is designated as severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) previously, referred to as nCoV-2019.In December of 2019, this novel corona virus was found to be a cause of upper and lower respiratory tract infections in Wuhan, a city in the Hubei Province of China. It rapidly spread throughout China and then gradually epidemic spreading to other parts of the world in pandemic proportions. It has spread almost every continent in this world. In February 2020, the World Health Organization designated the disease COVID-19, which stands for corona virus disease 2019 [2,3].
Mode of Transmission
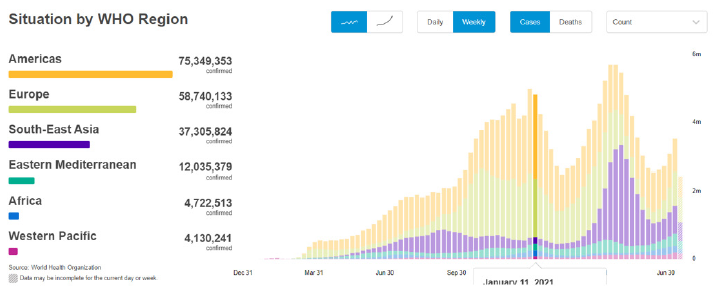
The virus is released along with the respiratory secretions when an infected person coughs, sneezes or talks. These droplets carrying the infection can spread infection to others if they make direct contact with the mucous membranes. Infection can also spread by touching an infected surface and followed by eyes, nose or mouth. Patients are thought to be most contagious when they show clinical symptoms of active disease. Some spread might be possible before symptoms appear, but this is not thought to be a common occurrence [4-6]. Asymptomatic carriers (also referred to as super spreaders) have been shown to spread the COVID-19. These are cases that have no symptoms and radiological manifestations but can transmit the virus to others [7]. Globally, as of 23rd july 2021, 17:11 GMT there have been 4,489,503 confirmed cases of COVID-19, 192,284,207 cases including 4,136,518 deaths, reported to WHO [8] Figure 1.
Figure 1: Countries, territories or areas with reported confirmed cases of COVID-19, 23 JULY 2021 [source -WHO].
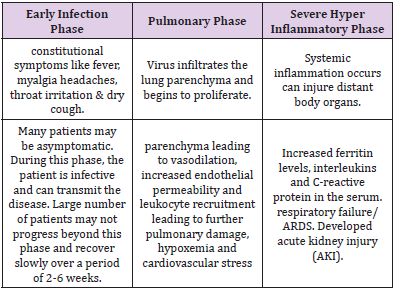
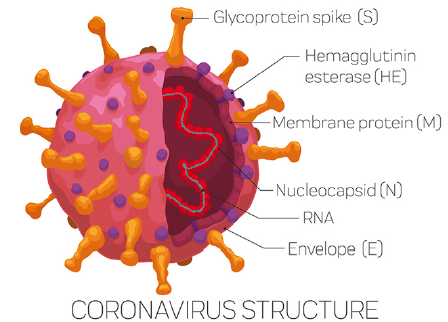
Pathophysiology of COVID-19
The Coronaviruses are a large family of single-stranded
RNA viruses (+ssRNA) that can be isolated in different animal
speciesSARS-CoV-2 belongs to the betaCoVs. It has a round or
elliptic and often pleomorphic form, and a diameter measuring
approximately 60–140 nm (Figure 2). According to recent research,
this spike mutation, which probably occurred around late November
2019, triggered transmission to humans. The disease progression
can be divided into below mentioned three distinct phases [9-11]
(Table 1).
a) Early infection phase
b) Pulmonary phase
c) Severe hyper-inflammatory phase
Clinical Features
a) Incubation period- approximately 4 to 14 days following
exposure [12,13]
b) Common clinical features at the onset of illness were [13,14].
c) Fever in 88-99 %
d) Fatigue in 38-70 %
e) Dry cough in 59-68%
f) Anorexia in 40 %
g) Myalgia in 15-35 %
h) Dyspnea in 19-31 %
i) Sputum production in 27-34 %
Laboratory Findings
Total number of peripheral white blood cells is normal or decreased, the lymphocyte count is reduced, and some children have increased liver enzymes, lactate dehydrogenase (LDH), muscle enzymes, and myoglobin some critically ill patients have increased troponin, D-dimer and ferritin and the number of peripheral blood lymphocytes have progressively decreased.
Radiology
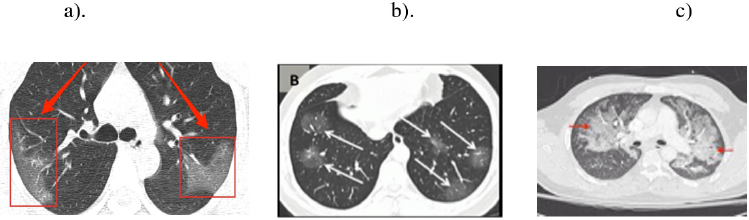
The most important finding in early stages is a single or multiple limited ground-glass opacity which is most commonly located under the pleura or near the blood vessel of the bronchus especially in the lower lobes. Severe period is very rare, manifested by diffuse unilateral or bilateral consolidation of lungs and a mixed presence of ground glass opacities [15]. Consolidation with surrounding halo seen in pediatric patients and was suggested as a typical sign in pediatric patients [16] (Figures 3 & 4).
Figure 4: CT thorax finding of COVID patient showing ground glass opacity in basal segment (a) diffuse consolidation with surrounding holo (b) and ground glass opacity with overlap of organizing pneumonia with diffuse alveolar damage(c)
Impact of COVID 19 Pandemic on Delivery of Surgical Care
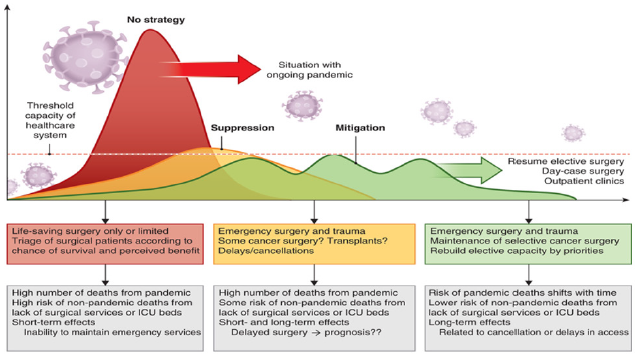
The pandemic of COVID-19 caused by the coronavirus SARSCoV- 2 is disrupting global health, social welfare and the economy in a proportion unparalleled in modern history [17]. In addition to the effects of the COVID 19 pandemic itself on public health, a collateral effect from panuniversal disruption and cancellation of operative interventions has emerged. The current pandemic has unprecedented implications for surgical services and patients with surgical conditions [18]. Surgical capacity may experience extreme challenges in pandemic zones [19,20]. The ability of surgical services to play a key role depends on the development of the peak of the pandemic, the spread of the infection and disease, the duration of societal regulations and implementation of societal laws, and the duration and temporal epidemic cycle repeats by which the disease burden will approach the threshold of maximum capacity of the critical care resources [21] (Figure 5).
Number of surgeries being put on a pause and how this
burden will be addressed in the fallout of the pandemic. Rough
estimates suggest that approximately 330 million operations are
done worldwide annually [22]. The vast majority in high-income
countries now following a strong policy of deferring of all nonemergency
surgeries (North America and European countries).
With a global average of about six million a per week, the total
numbers of patients who will be affected over the coming months
are growing rapidly .In the current pandemic, patients may prefer to
have elective surgery deferred due to fear of contracting the disease
during the hospital stay .However, this fear also leads to patients
not seeking timely care for conditions that would otherwise have
been correctable or curable by presenting at an earlier stage; loss
of function, reduced life expectancy and chronic debility may be the
result of delayed presentation and hence an untimely diagnosis.
This burden will only increase with the duration and severity of
the pandemic. When the destructive effects of natural or man-made
forces overwhelm the ability of a given area or community to meet
the demand for healthcare [23].
Trauma admissions still occur during a pandemic, although
there are unconfirmed reports of a reduction in acute and trauma
admissions due to social distancing and overall reduced activity
in society. Although trauma admissions may drop, so may the
recruitment of the regular bunch of blood donors, potentially
leading to a shortage of blood products in many systems. In
addition, coagulation may be affected in patients who are COVID-
19-positive, potentially adding to issues with bleeding injuries [24].
Patients who were admitted for an acute abdomen or any pathology
requiring acute surgery may be co-infected with COVID-19, and
hence represent a risk for infecting the healthcare personnel and
other patients, even when asymptomatic or experiencing severe
symptoms suggestive of COVID-19. One of the main concerns is
the ability asymptomatic patients may have to infect during the
incubation period [25].
Pandemic effects on organ transplantation is related to its
impact on the donor pool and the risk of transmission of infection,
risk to healthy living donors and overall access to scarce resources
[26,27]. The scenario of exposing a healthy donor to a major surgical
procedure in concordance with the risk of being infected with
COVID-19 must be considered and calls for caution, even if cases of
successful recovery exist [28]. As the overall strain of the pandemic
intensifies, this might dynamically change organ allocation and
prioritization of policies [26,27].
Material and Methods
The information and statistical data is collected from various international journals published worldwide and electronic media.
Results
Impacts of COVID pandemic on surgical services are profound
potentially long-lasting and extensive. Due to the cancellation
of surgeries, there is drastic effect not only on wellbeing of the
patient but also on emotional, psychological and physical health.
Surgeries which was planned in pre COVID week are cancellation
after lockdown because of that patients can experience feelings of
sadness, disappointment, anger, frustration and stress [29]. This
superimposes on the potential economic consequence (loss of
jobs, sick leaves or reduction in work availability) and impact on
family life. A complete neglect of certain surgical services can be
considered unwelcome collateral damage, and unwittingly increase
the number of deaths and life-years lost where the onus lies on the
COVID-19 pandemic. This can create ethical dilemmas at a time of
scarce resources and high pressure, burnout, guilt and unbearable
psychological pressure on health care workers. As elective surgery
has been cancelled on a scale never seen before in history of
modern medicine, the collateral damage to health and well-being,
maintenance of functionality, and risk of shortened lifespan is
present for patients in countries of all income and development
statuses. With a long-lasting lockdown and social distancing in
effect, there will be millions of operations cancelled, postponed or
simply not done at all over the times to come. The cancellation of
all elective operations creates a huge backlog of patients who have
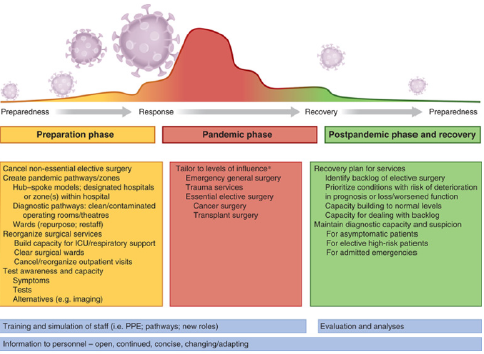
been, or would be, seen for planned surgery (Figure 6).
The effects of COVID-19 on surgical outcomes (and vice versa)
are not known. Pathological changes in blood coagulation [30],
inflammatory response [31], and co-morbidities added to single or
multiple organ failures, [32] may be considered as mechanisms for
added risk for surgery. Blood and blood products reserves could
be affected to a great extent as blood donations decrease due to
decrease in frequent (regular) blood donors, potentially leading
to as shortage of blood and blood products in some systems. In
addition, coagulation system may be deranged in patients who
are COVID-19-positive, potentially adding to issue in patients
undergoing major surgeries requiring blood transfusion and
traumatic bleeding injuries. Limiting access to transplantation is
associated with a significant fall in prognosis for most patients on the
transplant list, there is decreased donor pool, risk of transmission
of COVID infection to the healthy donor. Lung transplant recipient
have risk of getting infection via infected lungs. One of the main
concerns is the ability asymptomatic patients may have to infect
during the incubation period [33], and if large number of senior
surgeons is exposed to infected patients, the possibility for them
to become infected and requiring self-isolation is real and could
potentially result in a dangerous shortage of senior expertise
within surgical teams. The competition for scarce resources
related to hospital, ICU beds, health care workers, PPE and blood
transfusions mandates strict prioritization in several surgical
disciplines, notably transplantation, cancer surgery and other highrisk
procedures. As a result, some patients may unfortunately not
receive the treatment they would otherwise have received. The post
pandemic evaluation and future planning should involve strategies
to tackle shortage and include surgical services as an essential part
to maintain appropriate surgical care.
Abbreviations: PPE: Personal protective equipment; WHO: World Health Organization
Figure 6: Framework for surgical planning through pandemic phase.
Discussion
As elective surgery has been cancelled on a scale never before
seen in modern history, the collateral damage to health and wellbeing,
maintenance of function, and risk of shortened lifespan is
present for patients in countries of all income designation, poor
and marginalized will be affected most severely. In a situation
where resources are scarce, one should not treat or prioritize on a
first-come, first-served principle [34]. With a long-lasting lockdown
and social distancing in effect, there will be millions of operations
cancelled, postponed or simply not done at all over the times to
come. Surgery is already recognized as a scarce resource in much of
the world [35-36]. with a global challenge to provide safe surgery
and anesthesia as a recognized area of priority [37,38].
A strong advocacy agenda is needed that includes investigation,
planning research and communication for surgical services for
future pandemics. Surgical delivery before, during and after
a pandemic, owing to its cross-cutting nature and synergistic
effects on health systems at large needs to be addressed into the
WHO agenda for national health and planning. In this pandemic
situation mindful utilization of financial and human resources is
very important. Judicious utilization of resources and manpower
is of utmost importance in healthcare. It is important to ensure
the ability of surgeons, so we need to change the policies in the
country like construct surgical systems in terms of infrastructure,
workforce, care delivery, information management, financing and
governance so that we can combat the damage caused by this
pandemic. To inform COVID-19 surgical plans and address patients’
concerns effectively, there is an urgent need for high-quality multi
center research. Data on the effects of surgical cancellation on
patients’ complete well-being, including emotional and physical
health, are much required. In addition, the effect of the stacking
up of operations and the fallout of the pandemic will need to be
analyzed. Guidance is urgently needed on how to deliver surgical
services safely and effectively in the face of pressures placed by the
COVID-19 pandemic [17-19].
Conclusion
Surgical services need a contingency plan for maintaining surgical care in an ongoing or post pandemic phase. The current situation is unparalleled in history of modern medicine, and so no readily available information exists to compare or extrapolate the effect of disruption of surgical services and operations on public health during the global pandemic. To mount an effective response to the COVID-19 pandemic, hospitals should prepare detailed context-specific pandemic preparedness protocols and teams for surgical services and key domains for the same includes prepare a pandemic response plan for surgical services ,ensure staff are trained to deliver surgery safely during pandemic, hospital response to COVID-19,agree a team-based approach for running emergency services .Important areas for future research may include finding the impact of COVID-19 infection on postoperative outcomes, identifying risk stratification strategies, and determining whether prophylaxis using drugs for COVID (example HCQ) reduces rates of hospital-acquired COVID-19 infection. There is also a need to determine whether COVID-19 is present in abdominal fluids (urine, bile and peritoneal fluid) or aerosols created during introduction of pneumoperitoneum, in order to inform recommendations around the benefits and risks of open and laparoscopic surgery during the COVID-19 pandemic.
Conflict of Interests
The authors declare that they have no conflict of interest.
References
- National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases
- (2020) World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on 11 feb 2020.
- Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD (2010) Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol 76(9): 2712-2717
- (2020) WHO. Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (2019-nCoV) outbreak.
- Van Doremalen N, Bushmaker T, Morris D (2020) Aerosol and surface stability of HCoV-19(SARS-CoV-2) compared to SARS-CoV-1. medRxiv.
- Van Doremalen N, Bushmaker T, Morris D (2020) Aerosol and Surface Stability of SARS- CoV-2 as Compared with SARS-CoV-1. The New England Journal of Medicine.
- Bai Y, Yao L, Wei T (2020) Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020.
- WHO COVID-19 dashboard.
- Zhe Xu, Lei Shi, Yijin Wang, Jiyuan Zhang, Lei Huang, et al. (2020) Pathological findings of COVID-19 associated with acute respiratory distress syndrome. The Lancet (respiratory). Case Report 8(4): 420-422.
- Luciano Gattinoni, Silvia Coppola, Massimo Cressoni, Mattia Busana, Sandra Rossi, et al. (2020) Covid-19 Does Not Lead to a “Typical” acute respiratory distress syndrome. AJRCCM.
- XH Yao, TY Li, ZC He, YF Ping, HW Liu, et al. (2020) A pathological report of three covid-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49: E009.
- Li Q, Guan X, Wu P, Wang X, Zhou L, et al. (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med.
- Guan Wj, Ni Zy, Hu Y, Liang Wh, Ou Cq, et al. (2020) Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv.
- Wang D, Hu B, Hu C, Zhu F, Liu X, et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA.
- Ma HJ, Shao JB, Wang YJ (2020) High resolution CT features of novel coronavirus pneumonia in children[J]. Chin J Radiol.
- Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D (2020) Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol.
- WuY, Ho W, Huang Y, Jin DY, Li S, et al. (2020) SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet 395: 949-950.
- Spinelli A, Pellino G (2020) COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg.
- Ali HH, Lamsali H, Othman SN (2019) Operating rooms scheduling for elective surgeries in a hospital affected by war-related incidents. J Med Syst 43: 139.
- Bar-El Y, Reisner S, Beyar R (2014) Moral dilemmas faced by hospitals in time of war: the Rambam Medical Center during the second Lebanon war. Med Health Care Philos 17: 155-160.
- Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, et al. Feasibility of controlling COVID-19 outbreaks.
- Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, et al. (2020) Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 2016; 94:201F–209F.isolation of cases and contacts. Lancet Glob Health 8: e488-e496
- Goodwin J (2017) NAEMT National Survey on EMS preparedness for disaster and mass casualtyincidentresponse.
- Han H, Yang L, Liu R, Liu F, Wu KL, et al. (2020) Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med.
- Chang L, Yan Y, Wang L (2020) Coronavirus disease 2019: coronaviruses and blood safety. Transfusion Med Rev.
- Kumar D, Manuel O, Natori Y, Egawa H, Grossi P, et al. (2020) COVID-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant.
- Michaels MG, La Hoz RM, Danziger-Isakov L, BlumbergEA, Kumar D, et al. (2020) Coronavirus disease 2019: implications of emerging infections for transplantation. AmJ Transplant.
- Zhu L, Xu X, Ma K, Yang J, Guan H, et al. (2020) Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. AmJ Transplant.
- Herrod PJJ, Adiamah A, Boyd-Carson H, Daliya P, El-Sharkawy AM, Sarmah PB, et al. (2019) WES-Pi Study Group on behalf of the East Midlands Surgical Academic Network (EMSAN); WES-Pi Study Group. Winter cancellations of elective surgical procedures in the UK: a questionnaire survey of patients on the economic and psychological impact. BMJ Open 9: e028753.
- Han H, Yang L, Liu R, Liu F, Wu KL, et al. (2020) Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med.
- Qin C, Zhou L, Hu Z, Zhang S, Yang S, et al. (2020) Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis.
- Wang T, Du Z, Zhu F, Cao Z, An Y, et al. (2020) Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 395: e52.
- Chang L, Yan Y, Wang L (2020) Coronavirus disease 2019: coronaviruses and blood safety. Transfus Med Rev.
- Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, et al. (2020) Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med.
- Holmer H, Bekele A, Hagander L, Harrison EM, Kamali P, et al. (2019) Evaluating the collection, comparability and findings of six global surgery indicators. Br J Surg 106: e138-e150.
- McDermott FD, Kelly ME, Warwick A, Arulampalam T, Brooks AJ, et al. (2016) Problems and solutions in delivering global surgery in the 21st century. Br J Surg 103: 165-169.
- Søreide K, Winter DC (2019) Global surgery in an ecosystem for worldwide health. Br J Surg 106: e12-e13.
- Roa L, Jumbam DT, Makasa E, Meara JG (2019) Global surgery and the sustainable development goals. Br J Surg 106: e44-e52.

 Research Article
Research Article