ABSTRACT
Löfgren syndrome is an acute form of sarcoidosis with the classic triad of polyarthralgia, erythema nodosum (EN), and bilateral hilar lymphadenopathy (BHL). We present a case of a 29-year-old male who developed migratory polyarthralgia of large joints, fevers, and progressive rash after a camping trip. A chest CT revealed BHL. Joint aspiration did not demonstrate septic arthritis. Skin biopsy showed sarcoidal granulomatous septal panniculitis, most consistent with EN. He was diagnosed with Löfgren syndrome and successfully treated with dexamethasone.
Keywords: Löfgren Syndrome; Sarcoidosis; Migratory Polyarthralgia; Bilateral Hilar Lymphadenopathy; Erythema Nodosum; Mepolizumab; eGPA
Abbreviations: ANA: Antinuclear Antibody; ANCA: Antineutrophil Cytoplasmic Antibodies; CRP: C-Reactive Protein; ESR: Erythrocyte Sedimentation Rate
Introduction
Sarcoidosis is a systemic disease characterized by noncaseating granuloma formations in one or more organ systems. Löfgren syndrome is an acute form of sarcoidosis that presents with a classic triad of arthritis or periarthritis, erythema nodosum (EN), and bilateral hilar lymphadenopathy (BHL). The heterogeneous presentations of Löfgren syndrome, especially in the setting of additional rheumatologic diseases, requires high clinical suspicion and acumen for early diagnosis and treatment. We present a case of a 29-year-old male with Löfgren syndrome.
Case Report
29-year-old male with possible eosinophilic granulomatosis with polyangiitis (eGPA)) with severe persistent asthma controlled on mepolizumab presented with arthralgias, rash, and fevers a week after a camping trip. He denied any consumption of unfiltered water, tick bites, trauma, sick contacts, cough, diarrhea, dysuria, or vomiting. His polyarthralgias were asymmetric, present in large joints of all four extremities, and unresponsive to ibuprofen. The patient’s history was notable for a presumptive diagnosis of eGPA dating back to a systemic inflammatory illness at age 16, which manifested with eosinophilia, pericarditis, palpable purpura, pulmonary infiltrates, nephritis and asthma, although the diagnosis was never biopsy confirmed. He had been managed with daily prednisone (20 mg/day) for over a decade due to a lack of health insurance and had been unable to taper due to recurrent asthma, sinusitis, and rashes. Three months prior to presentation, the patient was started on mepolizumab 100mg sq monthly and was able to taper completely off of prednisone.
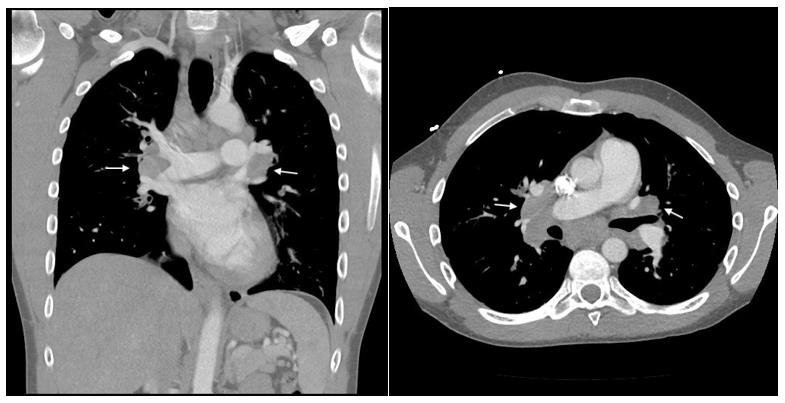
He was admitted to an outside hospital for severe right ankle swelling and underwent incision and drainage of his right posterior tendon tibial sheath for suspected septic arthritis. The aspirarate was clear, non-purulent and without growth on culture. Laboratory investigations were significant for WBC of 5.08 (ref 4.31-6.4 uL), normal absolute eosinophils, angiotensin converting enzyme (ACE) of 44 U/L (ref 9-67 U/L), negative chlamydia and gonorrhea PCR, and negative ANA and ANCA titers. He also had a negative quantiferon gold test four months prior to presentation. A chest CT demonstrated extensive, bilateral hilar and mediastinal adenopathy (Figure 1). He was started on vancomycin and discharged with cephalexin for right ankle cellulitis. His symptoms transiently improved on antibiotics but he was rehospitalized for progressive arthralgia, fevers, and new onset tender nodules on the left forearm four days later. On readmission, he was febrile to 38.1 C with otherwise normal vital signs.
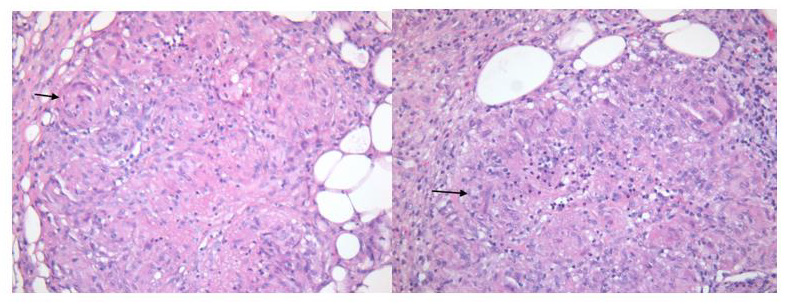
Physical exam was significant for pain with active and passive range of motion of large joints most pronounced in the right elbow, right wrist, right ankle and left knee. He had ill defined, pink erythematous patches on bilateral anterior lower extremities and 4 subcutaneous, slightly tender nodules on his upper and lower extremities. His laboratory analysis was significant for a WBC 9.52 K/cu mm (ref 3.5 - 10.8 K/cu mm) with 2% of eosinophil (ref 1-3%), creatinine of 1.32 (baseline of 1), ESR 58 mm/hr (ref 0-15 mmg/ hr), CRP 103 mg/L (ref <10 mg/L), and urine analysis without protein, blood, or WBC. Skin biopsy of the subcutaneous nodule on the left shin nodule demonstrated both sarcoidal and tuberculoid (intermittent central necrosis) granulomatous septal panniculitis without evidence of vasculitis (Figure 2). Although the presence of caseation and few eosinophils in his biopsy favored eGPA, his clinical presentation argued more for acute sarcoidosis.
Figure 2: Skin tissue biopsy of subcutaneous nodules demonstrate sarcoidal and tuberculoid granulomatous septal panniculitis.
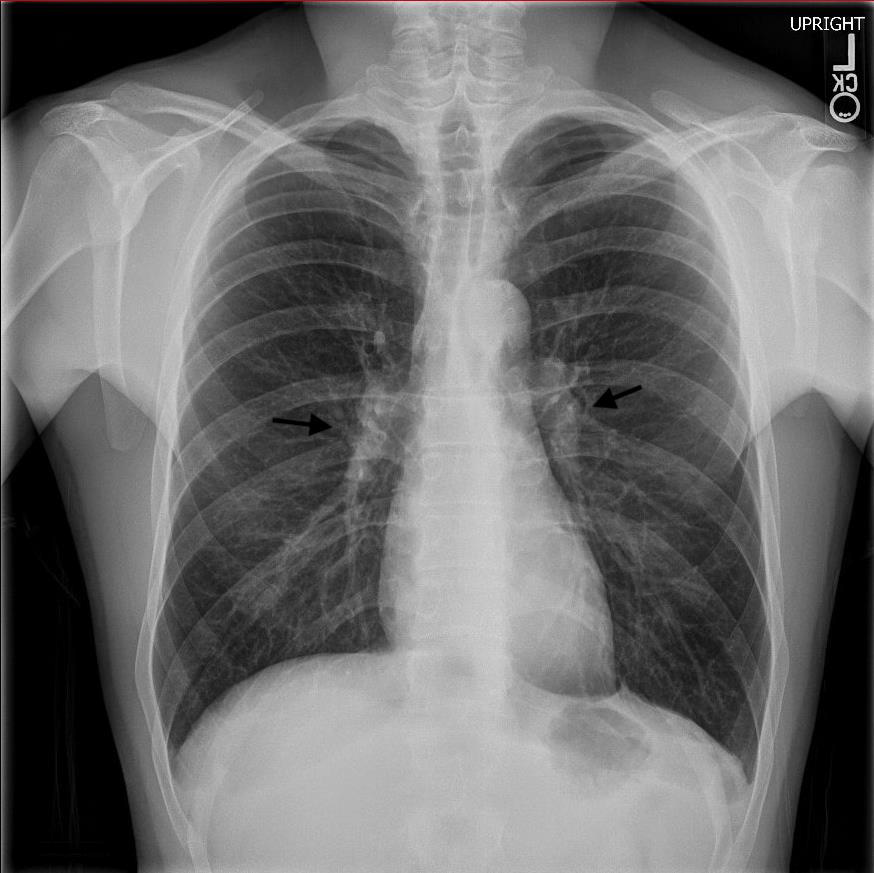
The differential diagnosis included infection, eGPA nodules, and Löfgren syndrome. Cultures and quantiferon were negative making infectious panniculitis less likely. EGPA nodules were considered, however this patient’s ankle arthritis, erythema nodosum, and hilar lymphadenopathy were most consistent with Löfgren syndrome. He was started on a dexamethasone 16-day taper starting at 6 mg daily and mepolizumab was continued. Post-discharge follow-up with rheumatology demonstrated resolution of arthritis, erythema nodosum, along with normalization of inflammatory markers. Three months post-treatment, his chest x-ray demonstrated decreased appearance of mediastinal and hilar lymphadenopathy when compared to prior CT (Figure 3). One year later, the patient continues to take mepolizumab without corticosteroids, and has had no recurrence of his symptoms.
Discussion
Sarcoidosis, first described by dermatologist Jonathan Hutchinson in 1877, is a systemic disease of unknown etiology resulting in noncaseating granuloma formation in any organ [1]. The diagnosis is likely in the presence of clinical symptoms of organ involvement with radiographic correlation, tissue biopsy with histological evidence of granulomas, and exclusion of other diseases with granuloma formation. Exclusion of other granulomatous diseases include granulomatosis with polyangiitis, exposures to particulates (beryllium, dust), and infections such as mycobacterium, coccidiomycosis, and syphilis are important considerations. Löfgren syndrome, first described by pulmonologist Sven Löfgren in 1946, is a subset of sarcoidosis with a distinct phenotype [2,3]. Unlike the chronic often insidious development of sarcoidosis, Löfgren syndrome presents acutely with the classic clinical triad of polyarthritis or periarthritis, BHL, and EN. Fever and uveitis may also be present.
The arthritis or periarthritis is most commonly observed at the ankles but can affect elbows, knees, and metacarpophalangeal joints. Articular symptoms usually precede or present concomitantly with development of tender, erythematous, subcutaneous nodules called EN. Of note, biopsy is not necessary to diagnose Löfgren syndrome. Our case of a 29-year-old male with a history for possible eGPA and severe asthma on mepolizumab who presented with migratory polyarthritis, EN, BHL, and fever is consistent with Löfgren syndrome. Infectious etiologies were considered but less likely given absent history of tick bites, negative sexually transmitted disease and quantiferon gold test, non-purulent right ankle aspirate, and absence of growth on cultures. His history of possible eGPA presented a unique clinical challenge to differentiate from Löfgren syndrome. EGPA, a rare medium size vasculitis, can present with fever, arthralgia, and rash [4]. EGPA can cause subcutaneous nodules on extensor surfaces, which show granuloma on biopsy and may also show eosinophilia and/or vasculitis. Although presence of fibrinoid changes and few eosinophils on skin biopsy made eGPA possible, lack of palpable purpura, necrotic plaques, or retiform purpura on skin exam and overall clinical presentation made a vasculitis etiology less likely.
Given the patient’s recent initiation of mepolizumab, an IL-5 humanized monoclonal antibody, drug-induced sarcoidosis-linked reaction (DISR) was also considered [5]. DISR is a multisystem, granulomatous reaction with an indistinguishable phenotype to sarcoidosis. The four most common classes of drugs to cause DISR include tumor necrosis factor-inhibitors, interferons, antiretroviral therapy, and immune checkpoint inhibitors (Chopra). DISR has a temporal association with initiation of the offending drug and often will self-resolve after the withholding of the suspected drug. Mepolizumab is an anti IL-5 therapy, which is relatively new, but thus far has not been reported to cause DISR. Because this patient remained on mepolizumab even after Löfgren syndrome was diagnosed and had clinical improvement, DISR secondary to mepolizumab is less likely. The diagnosis of Löfgren syndrome in our patient required a multidisciplinary team that recognized the clinical constellation of acute migratory polyarthritis, BHL, and EN. In a young patient with acute arthritis and skin lesions, acute sarcoid should be considered. Work-up should include a chest x-ray to identify BLH and skin biopsy may be helpful in recognizing erythema nodosum. Although Löfgren syndrome is a self-limiting condition, a course of systemic steroids may relieve symptoms and provide quicker recovery
Acknowledgement
No acknowledgements indicated.
Conflicts of Interest
The authors listed do not have any conflicts of interest.
Disclosures
• Marcia Friedman, MD
• Funding: KL2TR002370, OHSU Wheels Up Program
• MAF receives consulting fees for Revolo.
References
- R Handa (2021) Sarcoidosis: Rheumatological Considerations. in Clinical Rheumatology, Singapore: Springer Singapore, pp. 221-225.
- F Brown, P Modi, LS Tanner (2021) Lofgren Syndrome. in Stat Pearls.
- DA Rao, PF Dellaripa (2013) Extrapulmonary Manifestations of Sarcoidosis. Rheum Dis Clin North Am 39(2): 277-297.
- M Groh, Pagnoux C, Baldini C, Bel E, Bottero P, et al. (2015) Eosinophilic granulomatosis with polyangiitis (Churg–Strauss) (EGPA) Consensus Task Force recommendations for evaluation and management. Eur J Intern Med 26 (7): 545-553.
- A Chopra, A Nautiyal, A Kalkanis, MA Judson (2018) Drug-Induced Sarcoidosis-Like Reactions. Chest 154(3): 664-677.

 Case Report
Case Report