ABSTRACT
Purpose: The main study aim was to compare the validity of children sleep apnea data obtained from standard Polysomnography (PSG) to a Home Sleep Apnea Test (HSAT) accompanied by an attending online video technician.
Methods: Our study population was comprised of 100 children, 54 boys and 46 girls, ages 3-11 (average age 5.2, SD 1.2) assigned randomly either to in-lab full Polysomnography (PSG) or to a home apnea sleep test (HAST) with real-time, online technical support in order to rule out Obstructive Sleep Apnea (OSA). Results: A t-test comparison did not yield significant differences between data obtained from the in-lab PSG and HSAT with real-time, online, technical support for any of the following measures: Apnea Hypopnea Index (AHI), Oxygen Desaturation Index (ODI), baseline O2, or minimum O2 parameters. However, a significant difference was found for Time In Bed (TIB) and Total Sleep Time (TST), which was significantly longer in the HAST. Conclusion: Online HSAT can provide a safe, convenient and a reliable way to perform sleep studies in young children for diagnosing OSA in their familiar home environment.Keywords: Child; Polysomnography; HAST; OSA; Online
Abbreviations: AHI: Apnea Hypopnea Index, ODI: Oxygen Desaturation Index; TIB: Time In Bed; TST: Total Sleep Time; PSG: Polysomnography; OSA: Obstructive Sleep Apnea; EEG: Electroencephalography; EMG: Electromyography; EOG: Electro- Oculography; AHI: Apnea Hypopnea Index
Introduction
Obstructive Sleep Apnea (OSA) in children is a recognized
childhood health disorder with an estimated prevalence ranging
from 1% to 5% [1,2]. The clinical manifestations usually include
snoring, disrupted sleep, restlessness, sweating and salivation
during sleep, and excessive daytime sleepiness or hyperactivity and
irritation [3,4]. OSA in children is characterized by irregular, partial,
or complete obstruction of the upper airways during sleep, with the
disruption of normal ventilation and sleep patterns caused usually
by hypertrophy of the adenoids and tonsils. Risk factors include
obesity, neuromuscular disease, Down syndrome, and micrognathia
[3,5]. Continuous quality sleep is essential for growth, development,
good health, and well-being. Left untreated, OSA can lead to adverse
health, developmental, and behavioral outcomes [5-7]. Considering the high prevalence of OSA and its deleterious consequences, access
to early and accurate diagnosis is critical. Overnight, in-laboratory,
technician-attended Polysomnography (PSG) is considered the
gold standard for diagnosing OSA in children [2,8]. PSG provides
objective measures of sleep quality, sleep architecture, respiratory
parameters, and an index of the breathing disturbance during
sleep. However, the in-lab PSG test has some distinct limitations
and disadvantages, especially for diagnosing OSA in children.
In particular, in-lab PSG does not simulate the child’s sleep
in his or her familiar home environment. Moreover, placement
of multiple sensors and electrodes by an unfamiliar technician
in a strange room and bed can be stressful to young children and
many times impairs not only their cooperation but also the quality
of sleep that the PSG test purports to measure [9]. In addition -
hospital-based diagnostic testing limits access to families living far
from centrally-located medical diagnostic services. Beyond these
difficulties, the coronavirus (COVID-19) pandemic has reduced
access to in-lab PSG more generally, as healthcare providers
paused many non-urgent health care services in order to decrease
the risk of infection, especially in hospital environments. This led
to near-complete closure of sleep laboratories and clinics during
lockdowns around the world. As a result, concerns about lab-based
sleep studies now include not only questions of their efficacy, but
also of their safety. As a result, the Home Sleep Apnea Test (HSAT)
for children is increasingly considered as an alternative to in-lab
PSG. In contrast to adults, where home sleep tests for diagnosis of
OSA is the common practice, the clinical use of HSAT in children is
not well established. In particular, there are few studies comparing
the effectiveness of HSAT to PSG for diagnosing OSA in children.
This shortcoming is significant, as the use of HAST has the
potential to improve the validity of the sleep study, while reducing
possible exposure to infectious diseases during overnight hospital
stays. In addition, making HSAT more widely available can increase
access to needed sleep studies for children. The 2017 American
Academy of Sleep Medicine (AASM) Position Paper summarized
four published articles focusing on the technical feasibility of
HSAT for evaluating OSA in children. The paper concluded that the
validity of the home test depends on the training of the person who
places the sensors and is reduced when the sensors were placed
by untrained caregivers instead of trained professionals [8]. To
assess the validity of data obtained from HSAT, this study tested the
impact of providing home caregivers with prior training as well as
the support, in real time, of an attending online video technician on
the night of the sleep study. The technician guided them set up the
system, place the sensors, and then monitored the child throughout
the night using a web camera. Comparing the data obtained from
these assisted home sleep studies to those obtained in standard
PSG studies, we hypothesized that HAST with attending on-line
technician can provide valid and reliable way for diagnosis sleep
apnea in children.
Methods
Participants
100 children, 54 boys and 46 girls, ages 3-11 (average age 5.2, SD 1.2) assigned randomly either to in-lab full polysomnography or to a Home Sleep Apnea Test (HAST). All children were referred to a sleep study in order to rule out sleep apnea.
Polysomnography
For in-lab full polysomnography we used a standard inlab Somnoscreen-PSG type sleeping test device (Somnomedics, Germany). Sleep channels included: Electroencephalography (EEG), Electro-Oculography (EOG), leg and chin Electromyography (EMG), nasal flow, chest and diaphragm breathing, snoring, Electrocardiography (EKG), heart rate, blood oxygen saturation, body position, and video.
HAST
For the Home Sleep Apnea Test (HAST) we used a Somnotouch home sleep testing system (Somnomedics, Germany). Sleep channels included: nasal flow, chest and diaphragm breathing, snoring, heart rate, blood oxygen saturation, activity, body position, and online video recording using a Xiaomi 360 web-camera and portable Wi-Fi card.
Procedure
In-lab PSG: The sleep testing room was a standard test room at
the Sleep Medicine Research Center at Assuta Medical Center. The
child and his or her parents were invited to the sleep center at 8:00
PM. A skilled and trained technician interviewed the parents about
the medical history of the child and then connected the child to the
full PSG system in the sleep lab. The technician monitored the child’s
sleep throughout the night from the control center in the sleep lab.
The next morning, the parents completed a standard satisfaction
questionnaire. Sleep data were analyzed by a skilled and trained
sleep technician in accordance with the AASM guidelines (AASM,
2007). We calculated continuity and architecture sleep parameters
in addition to breathing and oximetry parameters, including the
number of apnea and hypopnea, Apnea Hypopnea Index (AHI),
baseline and minimum saturation, the number of desaturations, the
percentage of sleep time with O2 levels below 90% saturation, and
the percentage of time spent snoring.
HAST: The parents came without the child to the sleep center
at Assuta Medical Center on the evening of the sleep study to meet
a professional sleep technician for 20 to 30 minutes. During the
meeting, the technician reviewed the child’s medical history and
then taught the parents how to set up the system for conducting
the home sleep study. After practicing what they learned, the
parents returned home with the home sleep test system, including
a digital video camera. Using real-time video, the technician guided the parents at home while they set up the system and placed the
sensors on their child.
After the parents completed the setup, the technician
monitored the child’s sleep throughout the night using the digital
web camera. If there were any technical issues, such as a problem
with the attachment of a sensor, the technician telephoned the
parents and guided them as they made necessary corrections. After
the child woke up the next morning, the parents removed the sleep
system and returned it to the sleep center for analysis. The parents
were asked to complete a satisfaction questionnaire similar to that
filled out by parents after PSG. Sleep studies were included in data
analysis if at least 70% of the information collected during the study
was valid. For the HSAT studies, a professional scoring technician
calculated the Total Sleep Time (TST), Time In Bed (TIB), Sleep
Efficiency (SE), number of apnea and hypopnea, Apnea Hypopnea
Index (AHI), baseline and minimum saturation, the number of
desaturations, the percentage of time below 90% saturation, and
the percentage of time spent snoring.
Results
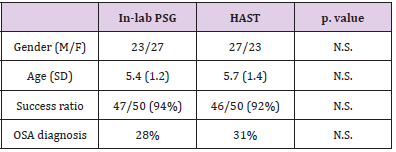
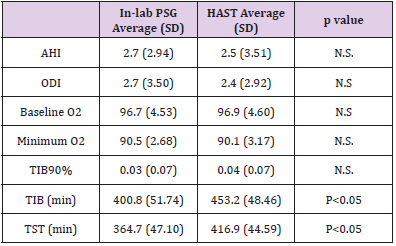
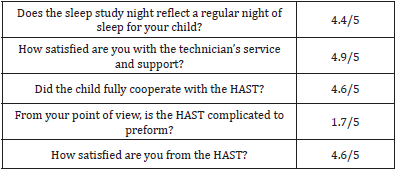
T-tests found no significant differences in the demographic profiles of the children in the PSG and HSAT groups (gender and age), in the success ratio, or in the OSA diagnosis between the sleep studies conducted with in-lab PSG and HAST (Table 1). Table 2 presents the Apnea Hypopnea Index (AHI), Oximetry Disorder Index (ODI), Baseline blood saturation (Baseline O2), minimum blood saturation (minimum O2), percentage time of blood saturation below 90% (TIB90%), Time In Bed in minutes (TIB), and Total Sleep Time (TST). Again, t-test comparisons found no significant differences between the in-lab PSG and HAST in any of these parameters with the exception of one: Time In Bed (TIB) and Total Sleep Time (TST) was significantly longer in the HAST group than in the PSG group. Survey results indicated that parents were very satisfied with HAST. In general, the parents gave high scores for the HAST. They reported that the night reflected a regular night of the child, the setup was friendly and easy, and the technician was available and pleasant (Table 3).
Table 2: Breathing disorder index (AHI), oximetry parameters (ODI), time in bed (TIB) and total sleep time duration (TST).
Discussion
This study found no significant differences between data
obtained from in-lab full PSG and HAST in all breathing and oximetry
parameters for diagnosis of Sleep Breathing Disorder (SBD) in
children. It is important to note that the majority of children are
referred to sleep laboratories in order to rule out sleep-related
breathing disorders [10], making it important that evaluations
focus on child breathing and oximetry channels and video (picture
and sound). These results support those from previous studies that
found no differences between HAST and in-lab PSG for evaluating
OSA in children. For example, Goodwin et.al report no differences
in PSG performed within two months after HAST in the respiratory
parameters [11]. Jacob et al. performed both a HAST and PSG
within one week for diagnosis of OSA in children and revealed
good correlation between the two types of studies [12]. Finally,
Alonso-Alvarez and colleagues compared simultaneous HAST to
PSG and found no significant differences in total number of apneas
or hypopneas between the HAST and the PSG, or in-laboratory
respiratory polygraphy studies [13]. However, these studies did not
address the concern that data validity can be affected by the training
of those who set up the home sleep system. This study addressed
this shortcoming by providing the attendance, supervision, and support of a real time online video technician, yielding reliable
data in a setting more favorable to the accurate diagnosis of OSA
in children.
The gold standard for the diagnosis of Obstructive Sleep Apnea
(OSA) in children is in-laboratory Polysomnography (PSG) [2,8].
One major reason for the preferability of in-lab sleep study is the
demand for a skilled technician during the setup phase and to
control the sleep study. In our HAST we used an online technician
that was an all-night attendant, using a web video camera, in order
to monitor the sleep study. We find that the parent’s guidance
before the sleep study and the technician’s online video supervision
during the set-up of the system on the child, and online monitoring
during the night, can replace the physical attendance of technician.
Additional support for the value of HAST comes from the fact that
there were no significant differences in the failure rate of sleep
studies between in-lab full PSG and HAST with an online technician,
indicating that there was no observed advantage for the physical
attendance of the technician over the online attendance. Finally,
significantly longer sleep times of the children in HAST with online
support indicates that sleep is better in a child’s natural environment,
improving the quantity and the validity of data obtained from the
home sleep study. This addresses one of the major challenges for
in-lab sleep studies for children. Although home sleep apnea testing
is widely used in adults to diagnose OSA [14], its use in children has
been much more limited, reflecting concerns about its validity for
accurately measuring the duration of sleep time. A major challenge
with HAST in children is the difficulty in determining the sleep time
without using EEG, EOG, and EMG channels.
Actigraphy is suggested as a reasonable technique for
measuring sleep due to its high accuracy (85-90%) and sensitivity
- the ability to correctly identify sleep (90-97%). Marino et al.
concluded that actigraphy is a useful and valid means for estimating
total sleep time with some limitation in specificity (the ability to
correctly identify alertness) [15]. Yet, specificity has been higher
in studies of nocturnal sleep-in children (54-77%) [16]. In our
data, the Time In Bed (TIB) and the Total Sleep Time (TST) were
significantly longer in HAST compared to in-lab PSG. In our HAST
we calculated Time In Bed (TIB) and Total Sleep Time (TST) using
two more channels besides activity: position and video. We believe
that the combination of these three channels is more sensitive and
specific than activity only. It needs to be evaluated in more studies.
A major question with in-lab full polysomnography is, “Does the
sleep study in the sleep lab reflect the regular sleep of the child?”
From our extensive experience in the Assuta Medical Center sleep
lab, some children will experience major problems sleeping in an
unfamiliar environment and not in their own bed. Moreover, even
when they succeed in falling asleep in the sleep lab, their sleep does
not simulate that experienced at home. The parents’ responses to
the study questionnaire supports our hypothesis that home sleep
studies improve the validity of sleep data collected to diagnose OSA
in children.
From the parent’s answers we observed a high rate of similarity
between the HAST night and a regular night for the child. Moreover,
parents report high cooperation from the child for the sleep
study at home and high satisfaction from the HAST in general.
Although the coronavirus pandemic (COVID-19) advanced the
use and legitimacy of telemedicine in many areas in medicine, its
advantages in diagnosing OSA in children are significant. With the
real-time online attendance of a sleep technician, this study showed
that home sleep studies can provide data of equal quality to in-lab
PSG while improving the quality and duration of a child’s sleep,
reducing in-hospital exposure to infectious disease, and improving
access to diagnostic services for families living far from centrallylocated
medical services. Taken together, these advantages of HAST,
when supervised by a real-time online technician, suggest that it
should be the first choice for diagnosing OSA in children.
Funding
No funding.
Conflicts of Interest
All authors declare no conflicts of interests and/or competing interest.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors Contribution
Not applicable.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Study number: ASMC 0092-20.
Consent for Publication
All authors gave consent for this publication.
References
- Bixler EO, Vgontzas AN, Lin HM, Liao D, Calhoun S, et al. (2009) Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep 32(6): 731-736.
- Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, et al. (2012) Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 130(3): e714-e755.
- (1996) Standards and indications for cardiopulmonary sleep studies in children. American Thoracic Society. Am J Respir Crit Care Med 153(2): 866-878.
- Budhiraja R, Quan S F (2009) Outcomes from the Tucson Children's Assessment of Sleep Apnea Study (TuCASA). Sleep Medicine Clinics 4(1): 9-18.
- Xu Z, Wu Y, Tai J, Feng G, Ge W, et al. (2020) Risk factors of obstructive sleep apnea syndrome in children. J Otolaryngol Head Neck Surg 49(1): 11.
- Carter KA, Hathaway NE, Lettieri CF (2014) Common sleep disorders in children. American Family Physician 89(5):68-377.
- Beebe DW (2006) Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep 29(9): 1115-1134.
- Kirk V, Baughn J, D Andrea L, Friedman N, Galion A, et al. (2017) American Academy of Sleep Medicine Position Paper for the Use of a Home Sleep Apnea Test for the Diagnosis of OSA in Children. Journal of Clinical Sleep Medicine 13(10): 1199-1203.
- Murata E, Kato Nishimura K, Taniike M, Mohri I (2020) Evaluation of the validity of psychological preparation for children undergoing polysomnography. Journal of Clinical Sleep Medicine 16(2): 167-174.
- Aurora RN, Zak RS, Karippot A, Lamm CI, Morgenthaler TI, et al. (2011) Practice parameters for the respiratory indications for polysomnography in children. Sleep 34(3): 379-388.
- Goodwin JL, Enright PL, Kaemingk KL, Rosen GM, Morgan WJ, et al. (2001) Feasibility of using unattended polysomnography in children for research-report of the Tucson Children's Assessment of Sleep Apnea study (TuCASA). Sleep 24(8): 937-944.
- Jacob SV, Morielli A, Mograss MA, Ducharme FM, Schloss MD, et al. (1995) Home testing for pediatric obstructive sleep apnea syndrome secondary to adenotonsillar hypertrophy. Pediatric pulmonology 20(4):241–252.
- Alonso Álvarez ML, Terán Santos J, Ordax Carbajo E, Cordero Guevara JA, Navazo Egüia AI, et al. (2015) Reliability of home respiratory polygraphy for the diagnosis of sleep apnea in children. Chest 147(4): 1020-1028.
- Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, et al. (2017) Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine 13(3): 479-504.
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, et al. (2013) Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 36(11): 1747-1755.
- Meltzer LJ, Walsh CM, Traylor J, Westin AM (2012) Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep 35(1): 159-166.

 Research Article
Research Article