Abstract
Background/Aim: Our aim is to explain the presence of pdl1 in nasal polyp by
immunohistochemical method. Detecting the PD-1 changes in nasal polyp tissue may
explain the development of chronic rhinosinusitis with nasal polyps and may help
develop new methods in the treatment of nasal polyps.
Methods: 20 patients who underwent endoscopic sinus surgery due to nasal
polyps and 20 patients who underwent surgery for functional and/or aesthetic reasons
and whose septum and turbinate mucosa were removed were included retrospectively.
Thick sections were taken from paraffin blocks for applying immunohistochemical
PDL-1 antibodies.
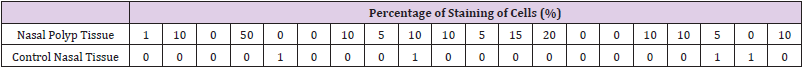
Results: PDL-1 positivity in nasal polyp tissues was significantly higher than
normal nasal mucosa epithelium (P=0.01). The recurrence rate was significantly
increased in patients with PDL-1 staining compared to other patients. (P=0.006)
Conclusion: PDL-1 was significantly increased in our patients with CRSwNP and
presence of PDl-1 is a predictive factor for recurrence in nasal polyposis.
Keywords: Nasal Polyps; PDL-1; Recurrens
Introduction
Chronic rhinosinusitis with nasal polyps (CRSwNP) are benign
inflammatory and hyperplastic outgrowths of the sinonasal
mucosa [1]. It is a disease that seriously affects the quality of life of
patients by causing nasal congestion, snoring, postnasal discharge,
nasal discharge, loss of sense of smell/taste. The prevalence of
CRSwNP is 1% to 4% in the general population [2]. CRSwNP is
observed more frequently in male patients between the 4th and
6th decades [3]. İn histologically, nasal polyposis is characterized
by respiratory epithelium covering oedematous stroma infiltrated
by inflammatory cells [2]. Eosinophilic infiltration is the most
common finding in polyp histopathology. In addition, there is an
infiltration of inflammatory cells such as lymphocytes, basophils
and macrophages.
Mucosal changes, including squamous metaplasia, secretory
hyperplasia and epithelial cell proliferation, are observed in polyp
tissues with the effect of chemical mediators secreted from these
cells. T-helper 2 (Th2) cell-directed eosinophilia develops as a
result of elevated immunoglobulin-E (IgE) and interleukin-5 (IL-5)
[4]. In Asians, the majority of patients with CRSwNP show features
of neutrophilic inflammation in addition to eosinophilia [5,6]. PD-1
(B7-H1,CD 274) is a protein-structured receptor belonging to the
immunoglobulin superfamily found on the surface of activated T
cells and antigen presenting cells. By binding to the PDL-1 ligand, T
cell inhibition occurs and escape from the immune system occurs.
PD-L1 works like a stop sign, inactivating the immune system’s T
cells. One of the ways in which sick cells escape from the immune system is to densely host the proteins called PD-L1 on the cell
surface. Studies have shown that PD-1 plays an important role in
immune tolerance and in the regulation of T cell function [7].
Genetic studies have found that PD-1 gene polymorphism
is associated with autoimmune diseases such as systemic
erythematosus and rheumatoid arthritis [8,9]. PD-1 and PDL-1
are expressed in many different tumors such as lung carcinoma,
lymphoma, pancreatic carcinoma, and renal cell carcinoma. It has
been reported that PD-1 expression is increased in T cells in patients
with CRSwNP with using flow cytometry [10]. This checkpoint led
to the development of immune checkpoint inhibitors, which are
the next generation immunotherapy drugs. These drugs prevent
the interaction of molecules such as PD-L1 and PD-1, thereby
activating the immune system against diseased cells. Among the
immune checkpoint inhibitors nivolumab and pembrolizumab act
by inhibiting PD-1 receptors, while atezolizumab and durvalumab
act by inhibiting PD-L1 receptors [11].
If the importance of pdl1 in nasal polyp becomes clear, these
immune checkpoint inhibitors drugs can be used in the treatment.
There are not enough studies in the literature regarding the presence
of PDL-1 in nasal polyps. In our study, our aim is to explain the
presence of pdl1 in nasal polyp by immunohistochemical method.
Detecting of the PDL-1 changes in nasal polyp tissue may explain
the development of chronic rhinosinusitis with nasal polyps and
may help develop new methods in the treatment of nasal polyps.
Materials and Methods
In our study, 20 patients who underwent endoscopic sinus surgery due to nasal polyps and 20 patients who underwent surgery for functional and/or aesthetic reasons and whose septum and turbinate mucosa were removed were included retrospectively, in Alanya Alaaddin Keykubat University Medical Faculty Hospital between 2010-2020. Previous sinus surgery, age is under 18 and nasal malignancies were exclusion criteria. 4 micron thick sections were taken from paraffin blocks for applying immunohistochemical PDL-1 antibodies. These sections were processed with Ventana PDL-1 (SP 263) monoclonal antibody on the fully automated Ventana Ultra Benchmark XT instrument. In the evaluation of PDL- 1 antibody applied immunohistochemically, the percentage of cells showing membranous staining with PDL-1 antibody was calculated among 100 tumor cells under light microscope. IHC staining results in groups were evaluated with Mann Whitney test using SPSS software version 22 (SPSS Inc., Chicago, IL, USA). P <0.001 was considered significant. Ethics committee approval was obtained from Alanya Alaaddin Keykubat University (no:2021/09-06).
Results
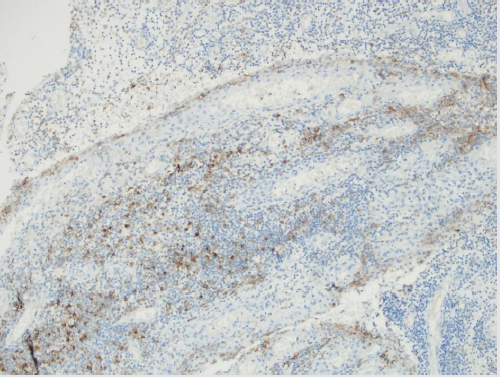
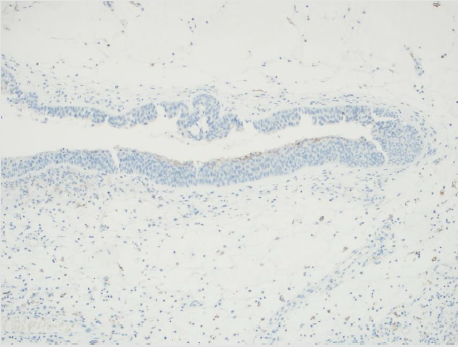
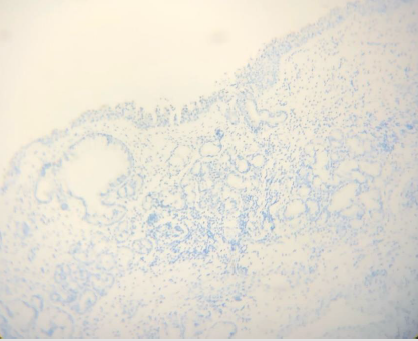
There were 2 female and 18 male patients in the study group, and 4 female and 16 male patients in the control group. The mean age was 37.4±8.6 years in the study group and 35.4±8.8 years in the control group. PDL-1 positivity in nasal polyp tissues was significantly higher than normal nasal mucosa epithelium. (P=0.000) (Table 1) (Figures 1-3) The recurrence rate was higher in PDL-1 positive cases with nasal polyps, and the recurrence rate increased as the staining rate increased, and it was statistically significant. (P=0.003).
Discussion
There are some hypotheses exist for how CRSwNP develops
but the aetiopathologenetic mechanism of it is still unclear [2,12].
The pathogenesis of it is thought to involve persistent inflammation
of the nasal mucosa due to infiltration by eosinophils, basophils,
lymphocytes, neutrophils and mast cells [2]. T lymphocytes act as
the main actor in this inflammation process. PDL1 İs a member
of the B7 family that regulate the T-cell response and a predictive biomarker. It is a cell-surface glycoprotein primarily expressed
by antigen-presenting cells. Studies on PDL 1 in the literature
are mostly about tumor cells. Different cut-off values have been
reported in these studies [13-16]. However, variable cut-off levels
create difficulties for researchers in making decisions during
evaluation. Determining a standard cut-off value for researchers
is important for the correct interpretation of the results and for
the consistency between the results of the studies. In our study,
we considered the presence of PDL-1 positive in staining of 1% or
more. Different companies have antibodies and subclones for PDL-
1. In the literature, there are studies reporting different results with
antibodies and clones of different companies in the same cell group
[17,18].
We used the SP263 clone of Ventana, which is frequently used
in studies in the literature, to increase the staining quality and
the reliability of the results. There are studies explaining that the
infectious process plays a role in the pathogenesis of CRSwNP
[19,20]. İt is reported that IFN-γ secretion increases after incubation
of lymphocytes with bacterial and fungal extracts [21,22]. IFN-γ is
an important cytokine thas is a strong inducer of PDL-1 expression
[23]. Before studies showed IFN-γ have been identified in nasal
polyposis [24,25]. PDL-1 levels in other cell membranes increases
by the IFN-γ charged by T-cells. Thus, it causes a negative feedback
in nasal polyposis by causing down-regulation of T-cell responses.
İn a study about mRNA expression of PDL-1 in patients with
CRSwNP, resarchers found mRNA levels of PDL-1 was increased in
nasal polypies epitel compared to healty nasal tissue epitel [26].
Although there are studies in the literature that measure
PDL1 level in nasal polyp tissue and blood cells by PCR and flow
cytometry, but there is not enough study in which the pDL1 level
in nasal polyp tissue is analyzed immunohistochemically. In a
small study in the literature using only 3 nasal polyp tissues and
3 nasal tissues as control, immunohistochemical evaluation was
made and PD-1+ cells were indeed increased in the submucosa of
NP tissue compared to control tissue [27]. İn our study we found
that the pdl1 level in CRSwNP tissue was significantly higher
than the pdl1 level in the control healthy nasal tissue, and it was
was statistically significant. (p:0.01). For this reason, the use of
monoclonal antibodies developed against PDL-1 as a target drug
as a non-surgical drug therapy in nasal polyps is a matter of debate.
Recurrence in surgical procedures is an undesirable situation for
the patient and the surgeon. Different researchers used several
markers for predicting nasal polyp recurrence.
Recurrence is frequently observed in nasal polyposis, and
recurrence is higher in eosinophilic polyps than in noneosynphilic
polyps [28]. Zhong et al. in their study, the relationship between
peripheral eosinophil count and recurrence was examined and
they found a significant correlation between high peripheral blood
eosinophil count and recurrence [29]. In another study showed
researchers that a tissue eosinophil proportion of >27% of total cells
was a marker for recurrence within 2 years after endocopic sinus
surgery in patients with CRSwNP [30]. In our study, recurrence rate
was high, and it was found in 10 (50%) patients. The recurrence
rate was higher in PDL-1 positive cases with nasal polyps, and the
recurrence rate increased as the staining rate increased, and it was
statistically significant. (P=0.003) These findings suggest that the
presence of PDL-1 may be a predictive factor for recurrence.
Limitations
The most important limitation of our study is that it was a retrospective study, and we could not reach sufficient patient material, since the operated patients took the operation materials to an external center for histopathological consultation. It will be possible to make a clearer comment on the fact that it is a determining factor in the development of recurrence.
Conclusion
PDL-1 was significantly increased in our patients with CRSwNP compared to normal nasal mucosa tissue. Presence of PDl-1 is a predictive factor for recurrence in nasal polyposis. Since there are not many studies explaining the presence of CRSwNP and PDL- 1 in the literature, we think that our study will contribute to the literature. New studies with a larger number of patients are needed to determine the presence and importance of PDL-1 in nasal polyps.
References
- Toro E, Portela J, Pearls S (2020) Nasal Polyps. PMID: 32809581 Bookshelf ID: NBK560746.
- Fokkens W, Lund V, Mullol J, et al. (2007) European position paper on rhinosinusitis and nasal polyps 2007. Rhinology Suppl 20: 1-136.
- Shi LL, Xiong P, Zhang L, Cao PP, Liao B, et al. (2013) Features of airway remodeling in different types of Chinese chronic rhinosinusitis are associated with inflammation patterns. Allergy 68: 101-109.
- Shi LL, Song J, Xiong P, Cao P P, Liao B, et al. (2014) Disease-Specific T-Helper Cell Polarizing Function of Lesional Dendritic Cells in Different Types of Chronic Rhinosinusitis with Nasal Polyps. Am J Respir Crit Care Med 190(6): 628-638.
- Baba S, Kagoya R, Kondo K, Suzukawa M, Ohta K (2015) T-cell phenotypes in chronic rhinosinusitis with nasal polyps in Japanese patients. Allergy Asthma Clin Immunol 11: 33.
- Ikeda K, Shiozawa A, Ono N, Kusunoki T, Hirotsu M, et al. (2013) Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 123: 1-9.
- McGee HS, Yagita H, Shao Z, Agrawal DK (2010) Programmed Death-1 antibody blocks therapeutic effects of T-regulatory cells in cockroach antigen-induced allergic asthma. Am J Respir Cell Mol Biol 43(4): 432-442.
- Belkhir R, Burel S, Dunogeant L, Marabelle A, Hollebecque A, et al. (2017) Rheumatoid arthritis and polymyalgia rheumatica occurring after immune checkpoint inhibitor treatment. Ann Rheum Dis 76(10): 1747-1750.
- Bertsias GK, Nakou M, Choulaki C, Raptopoulou A, Papadimitraki A, et al. (2009) Genetic, immunologic, and immunohistochemical analysis of the programmed death 1/programmed death ligand 1 pathway in human systemic lupus erythematosus. Arthritis Rheum 60(1): 207-218.
- Lee W, Chang L, Huang Z, Huang J, Yang L, et al. (2017) Retrospective Analysis of γδ T Cell Expression in Chronic Rhinosinusitis and Its Association with Recurrence of Nasal Polyps. ORL 79(5): 251-263.
- Vaddepally RK, Kharel P, Pandey R, Garje R, Chandra AB (2020) Review of Indications of FDA-Approved Immune Checkpoint Inhibitors per NCCN Guidelines with the Level of Evidence. Cancers (Basel) 12(3): 738.
- Rinia AB, Kostamo K, Ebbens FA (2007) Nasal polyps: a cellular-based approach to answering questions. Allergy 62(4): 348 -358.
- Chow LQ, Haddad R, Gupta S, Mahipal A, Mehra R, et al. (2016) Antitumor activity of pembrolizumab in biomarkerunselected patients with recurrent and/or metastatic head and neck squamous cell carcinoma: results from the phase Ib KEYNOTE- 012 expansion cohort. J Clin Oncol 34(32): 3838-3845.
- Ferris RL, Blumenschein G, Fayette J, Guigay J, Colevas AD, et al. (2016) Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med 375(19): 1856-1867.
- Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, et al. (2016) Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol 17(7): 956-65.
- Martinez Marti A, Martinez P, Navarro A, Cedres S, Murtra-Garrell N, et al. (2014) Concordance of PD-L1 expression by different immunohistochemistry (IHC) definitions and in situ hybridization (ISH) in squamous cell carcinoma (SCC) of the lung. ASCO Annual Meeting Proceedings.
- Hirsch FR, McElhinny A, Stanforth D, Ranger-Moore J, Jansson M, et al. (2017) PD-L1 immunohistochemistry assays for lung cancer: results from phase 1 of the blueprint PD-L1 IHC assay comparison project. J Thorac Oncol 12(2): 208-222.
- Hodgson A, Slodkowska E, Jungbluth A, Liu SK, Vesprini D, et al. (2018) PD-L1 immunohistochemistry assay concordance in urothelial carcinoma of the bladder and hypopharyngeal squamous cell carcinoma. Am J Surg Pathol 42(8): 1059-66.
- Ponikau JU, Sherris DA, Kern EB, Homburger HA, Frigas E, et al. (1999) The diagnosis and incidence of allergic fungal sinusitis. Mayo Clin Proc 74(9): 877-884.
- Van Zele T, Gevaert P, Watelet JB, Claeys G, Holtappels G, et al. (2004) Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J Allergy Clin Immunol 114(4): 981-983.
- Shin SH, Ponikau JU, Sherris DA, Congdon D, Frigas E, et al. (2004) Chronic rhinosinusitis: an enhanced immune response to ubiquitous airborne fungi. J Allergy Clin Immunol 114(6): 1369-1375.
- Douglas R, Bruhn M, Tan LW, Ooi E, Psaltis A (2007) Response of peripheral blood lymphocytes to fungal extracts and staphylococcal superantigen B in chronic rhinosinusitis. Laryngoscope 117(3): 411-414.
- Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, et al. (2002) Tumorassociated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med 8(8): 793-800.
- Sánchez-Segura A, Brieva JA, Rodríguez C (1998) T lymphocytes that infiltrate nasal polyps have a specialized phenotype and produce a mixed TH1/TH2 pattern of cytokines. J Allergy Clin Immunol 102: 953-960.
- Bernstein JM, Ballow M, Rich G, Allen C, Swanson M (2004) Lymphocyte subpopulation and cytokines in nasal polyps: is there a local immune system in the nasal polyp? Otolaryngol Head Neck Surg 130: 526-535.
- Krohn IK, Bobic S, Dooley J, Lan F, Zhang N, et al. (2017) PD-1 expression correlates with disease severity and IL-5 in Chronic Rhinosinusitis with Nasal Polyps. Allergy 72: 985-993.
- Krohn IK, Bobic S, Dooley J, Lan F, Zhang N, et al. (2017) Programmed cell death-1 expression correlates with disease severity and IL-5 in chronic rhinosinusitis with nasal polyps. Allergy 72(6): 985-993.
- Tokunaga T, Sakashita M, Haruna T, Asaka D, Takeno S, et al. (2015) Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 70(8): 995-1003.
- Zhong B, Yuan T, Du J, Tan K, Yang Q, et al. (2021) The role of preoperative blood eosinophil counts in distinguishing chronic rhinosinusitis with nasal polyps phenotypes. Int Forum Allergy Rhinol 11(1): 16-23.
- Lou H, Meng Y, Piao Y, Wang C, Zhang L, et al. (2015) Predictive significance of tissue eosinophilia for nasal polyp recurrence in the Chinese population. Am J Rhinol Allergy 29(5): 1-7.

 Research Article
Research Article