ABSTRACT
Blood flow restriction training (BFRT) is a technique used to restrict blood flow to a muscle group whilst undergoing a strengthening programme. This can be with the aim of improving strength and function or reducing muscle atrophy as part of a rehabilitation programme. However due to its limited use there is scant amount of studies evaluating its effects. We conducted a literature review within the PubMed database of all randomised controlled trials involving BFRT from the database’s inception to October 2021. There was evidence of BFRT resulting in improvements in one repetition maximum, timed stand tests and quadriceps cross-sectional area3, however there was minimal difference between BFRT and other training regimes used: high-intensity resistance training and low-intensity resistance training (LI-RT). BFRT also resulted in significant reductions in WOMAC pain scores, similar to LI-RT. We also set out to assess the value of BFRT in the context of degenerative conditions such as osteoarthritis, in which high-volume training is not possible. One trial in this area4 did not demonstrate a significant difference between the two but did show that BFRT is a viable alternative to moderate-intensity resistance training (MIRT).
Objectives: Find out if blood flow restriction training (BFRT) is effective at improving muscle strength and function and reducing atrophy for patients with knee osteoarthritis.
Introduction
BFRT involves restricting blood flow to a targeted muscle group whilst making it perform movements under low load resistance. The aim of this is to achieve the same effect that putting the muscle through high resistance training (HRT) would accomplish. HRT is often not possible in certain patients due to cases involving injury or conditions such as osteoarthritis. In individuals without injury, there is already evidence that noteworthy improvements have been made to muscular hypertrophy, muscle fibre recruitment and endurance with BFRT (Takarada, et al. [1]). For healthy individuals, the American College of Sports Medicine recommends training with loads of 60–70% of their one repetition maximum (RM) for 8–12 repetitions to maximise muscular strength. However, for patients with knee pathology, performing movements with loads of 60–70% of their one RM may not be possible and could cause further injury (Buckthrope, et al. [2]). Quadriceps and hamstring muscles often atrophy with chronic osteoarthritis. The intention of using BFRT with patients is to reduce the level of atrophy and weakness in muscles caused [2,3]. For individuals over 60, osteoarthritis is the most common cause of disability. With a growing ageing population, osteoarthritis is likely to only increase in prevalence.
Many factors contribute to reduced function in patients with osteoarthritis; muscle weakness, especially in the quadriceps muscles, is a major cause of functional decline. The current advice is that patients with osteoarthritis can only participate in low to moderate load and intensity training. Due to the inability of these patients to engage with higher load or high-intensity training without associated knee pain or injury, BFRT is a valid alternative. The goal of BFRT is to increase skeletal muscle and strength without causing further injury or knee pain (Ferraz, et al. [3]). This literature review intends to give the reader an insight into the effectiveness of BFRT for osteoarthritis patients. This study will discuss several papers and relate whether the evidence suggests that BFRT can be used more widely in practice for knee osteoarthritis.
Methods
Search design: Studies were chosen following a comprehensive search of the PubMed database by independent researchers. The database was filtered to highlight studies that included the following in their title or abstract: ‘blood flow restriction’, ‘KAATSU’ or ‘blood flow occlusion’. To further narrow the search criteria and suit the objectives, search filters for ‘osteoarthritis’, ‘rehabilitation’, ‘lower limb’, ‘injury’ or ‘recovery’ were included with an ‘AND’ function. The database was searched from its inception until 1st October 2021. The studies selected for further discussion were ‘randomised controlled trials’ only. Literature reviews were also assessed to search for more trials to be used for comparison.
Design Rationale: ‘Randomised controlled trials’ were solely chosen for their ability to provide clear, objective outcomes, which, when pooled together, would provide data from which to draw significant conclusions. No time limit was placed on the trials used as, after consideration, each of the content was still deemed relevant to the objectives of the review.
Inclusion and Exclusion Criteria: After a review of the available literature, the following conditions were proposed for the study to be considered suitable:
(a) Randomised controlled trial or technical note;
(b) Primary focus on blood flow restriction training;
(c) A patient group comprising individuals using BFRT as a form of rehabilitation or recovery following osteoarthritis diagnosis; and
(d) Sole focus on lower limb and concentration on studies about osteoarthritis.
Limitations of the Methodology Used: Only the PubMed database was used to search for studies. Limiting to the abovementioned search criteria also restricted the number of studies available, hence reducing the significance of the review’s findings. The authors recognised this but deemed that it was more important to keep the aims of the review concise and coherent.
Studies Reviewed
Methods
A randomised controlled trial 3 conducted in Sao Paulo, Brazil, between 2011 and 2013 included women between 50–65 years of age with a diagnosis of knee osteoarthritis based on the criteria of the American College of Rheumatology. Exclusion criteria included a) Physical exercise training over the last year
b) Cardiovascular disease
c) Musculoskeletal issues preventing exercise engagement
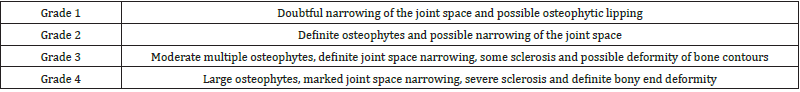
d) Kellgren–Lawrence radiological assessment of 1 or 4 (Table 1)
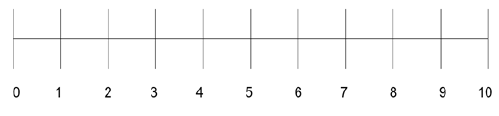
e) Knee pain with a score of less than 1 or more than 8 on the visual analogue scale (Table 2)
f) Non-Steroidal Anti-inflammatory Drug (NSAID) use over the last three months; and
g) Intra-articular infiltration with hyaluronic acid and corticosteroids infiltration over the past six months. Fortyeight patients met the requirements to be included in the trial. Patients were asked to rate their knee pain on a scale of 1–10 on a visual analogue scale and were split into three groups according to their 1-RM weight for the leg press exercise.
They were then randomly allocated into one of the three groups:
1. High-intensity resistance training (HI-RT)
2. Low-intensity resistance training (LI-RT)
3. Low-intensity resistance training with BFRT [3]
Patients were assessed at baseline and after 12 weeks of BFRT training relative to the HI-RT group. Their progress was measured based on the 1-RM leg press, knee extension, timed-stands test (TST), timed up and go test (TUG), quadriceps cross-sectional area and self-reported quality of life. The self-report was evaluated using a Short Form Health Survey (SF-36) and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) [3]. The women selected for this trial completed a twice-weekly resistance training exercise, which included bilateral leg press and knee extension, using strength training machines in a gymnasium. The LI-RT with BFRT group performed the exercises wearing an air cuff with a width of 175 mm and length of 920 mm that was placed at the inguinal fold and inflated to provide a pressure of 70% required for complete BFR. The restriction was maintained for all training sessions, including rest periods, and was immediately released after the session was complete. Cuff pressure was determined using a vascular doppler over the tibial artery that records the cuff pressure required at the inguinal fold for a complete loss of auscultatory pulse and then calculating 70% of that pressure [3]. The first-week training programme involved the HI-RT group performing four sets of 10 repetitions at 50% of their 1-RM. Comparatively, the LI-RT and LI-RT with BFRT groups performed four sets of 15 repetitions at 20% of their 1-RM.
From the second week onwards, the HI-RT group performed 80% of their 1-RM, while both the LI-RT and LI-RT with BFRT group’s intensity were increased to 30% of their 1-RM. After the fifth week, all groups raised the number of sets on both exercises from four to five. In between each set, all participants had a one-minute rest. Every four weeks, the participants’ 1-RM was reassessed, and the weight used for their training sets adjusted accordingly [3]. Based on the exclusion criteria, 48 patients were found for this study. They were divided equally into three groups, with 16 individuals per group. The HI-RT group had the most withdrawals at six, four of which were due to exercise-induced knee pain. Comparatively, the other two groups had fewer withdrawals, none of which was due to exercise-induced pain. Additionally, adherence to training protocols was 90% for HI-RT, 85% for LI-RT and 91% for BFRT [3]. Tests conducted to assess strength and functional movement: 1-RM for leg press and knee extension along with TST and TUG3. The TST records the number of times an individual can stand up from an armless chair, 45 cm in height, in 30 seconds. TUG tests record the time taken for a person to stand up from an armless chair, 45 cm in height, walk 3 metres, turn and return to the chair to sit down again. The patients in the study underwent familiarisation sessions for all tests so that learning rate did not affect the results.
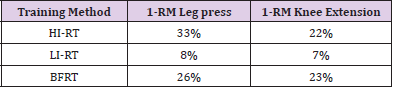
Coefficients of variation for all tests were under 10%, suggesting that it is unlikely that other factors are the source of the variation (Table 3) shows within-group increases in 1-RM for leg press and knee extension in both the HI-RT and BFRT groups. For the HI-RT group, there was a 33% increase in the patients’ 1-RM leg press weight and 22% increase for their 1-RM knee extension. For the BFRT group, there was an increase of 26% and 23% for their 1-RM leg press and knee extension, respectively. Both groups showed a significant increase in 1-RM tests. However, there was no significant difference between the groups which were compared to each other after training [3]. In the case of the LI-RT group, their 1-RM leg press and knee extension increased by 8% and 7%, respectively. This growth was not significantly different, with P = 0.22 for the leg press and P = 0.23 for the knee extension. Significant improvements were seen in the HI-RT and BFRT groups for TST; with an increase of 14% for HI-RT and 7% for BFRT. Comparatively, the LI-RT group had no significant improvement with their 5% increase. Again, no significant differences were noted between the groups after training. For the TUG test, there were no significant differences noted either within or between the three groups after training [3]. The quadriceps cross-sectional area (CSA) was assessed using Computerized Tomography (CT) at the midway point between the greater trochanter and the lateral epicondyle of the femur by a researcher who was blinded to the treatment.
Table 3: Within-group increases in 1-RM for leg press and knee extension after 12 weeks of training.
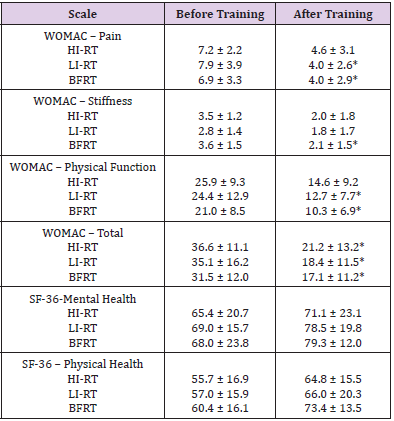
Therefore, it is unlikely that there was any bias affecting the measurements. However, there are reasons other than an increase in muscle mass, which could be the cause of an increased crosssectional area [3]. For the post-training quadriceps CSA assessment, the results showed that there was a CSA increase in the HI-RT group by 8% and in the BFRT group by 7%. However, with an increase of 2%, there was no significant increase in the LI-RT group. It should also be noted that although the CSA increased within the groups, the groups were still not significantly different from each other after training (P > 0.05). Additionally, the HI-RT and LI-RT with BFRT groups were not significantly different, indicating that the two may be equally effective at increasing quadriceps CSA [3]. The WOMAC and SF-36 scales were used to assess pain and quality of life. The WOMAC scale is widely used in the evaluation of hip and knee osteoarthritis; it is divided into three subscales: pain, stiffness and physical function. The individual domains of each scale were recorded separately as can be seen in (Table 4). The table displays the changes in the WOMAC and SF-36 scores before and after training. The data shows the mean result for each category followed by the ± standard deviation 3. *P < 0.05 for within group comparisons [3]. For all groups, their scores in all WOMAC categories were similar before training and therefore comparable (P > 0.05).
After training, the WOMAC pain score was significantly lower for both the LIRT and BFRT groups as can be seen in (Table 4). There was a decrease in score by 45% in the LIRT group (Effect Size (ES) = –0.79, P = –0.001) and a decrease by 39% in the BFRT group (ES = –0.79, P = 0.02). Comparatively, the HIRT group only had a decrease of 31% (ES = –0.54, P = 0.19). The WOMAC stiffness score was significantly lower after training in the BFRT group [3]. BFRT was shown to be equally effective in improving strength as can be seen by the within-group increases in 1-RM for leg press and knee extension after 12 weeks of training. The TST showed that HI-RT and BFRT were both effective. However, there was no significant difference in the TUG test score, suggesting that there is a potential for BFRT to aid with functionality in osteoarthritis patients. BFRT appears to be equally effective as HIRT at improving quadriceps CSA. The WOMAC scores indicate that BFRT would be preferred over HIRT to reduce pain and improve quality of life. However, there was no difference in the SF-36 [3]. As can be seen from the above results, BFRT is equally successful in improving strength and function and increasing muscle mass to prevent atrophy whilst causing much less pain or discomfort to the patient than HIRT. As the study excludes patients who scored 1 or 4 on the Kellgren– Lawrence scale, it cannot be argued that the same results will be achieved for all patients with osteoarthritis, especially those with a score of 1 and with mild osteoarthritis or those with a score of 4 and with severe osteoarthritis.
Although, those with a score of 4 will not be able to perform the activity required for this training [3]. Another disadvantage is that VAS, SF-36 and WOMAC are self-assessments; due to the nature of how arterial occlusion is obtained, participants will know when they are in the BFRT group. Additionally, only woman of a specific age range are included in this trial; thus, it is unclear if the same findings will occur in men or women outside the age range of 50–65, especially when numerous patients with osteoarthritis are older than 65. There is also the possibility that other medications taken by the patients could either positively or negatively affect their performance and skew the results. Furthermore, only a small sample size (48 patients) was used in this study. In the future, a study with a larger and more diverse population would need to be used to better determine the efficacy of BFRT. Despite its small sample size, this study showed that BFRT has similar efficacy in improving lower limb strength, quadriceps cross-sectional area and knee function as HI-RT. BFRT also presented greater improvement in WOMAC scores relative to HI-RT. Moreover, there were substantially fewer patients in the BFRT group who withdrew from the study. All of these suggest that BFRT could be used as a possible substitute for HI-RT in patients with osteoarthritis; thus, they do not need to undergo vigorous exercises that can cause pain, and yet still achieve positive muscular changes [3].
In Florida (USA), in a pilot randomised clinical trial of 35 patients with symptomatic knee osteoarthritis causing physical limitations, the patients performed 12 weeks of lower limb training comparing BFRT against moderate-intensity resistance training (MIRT). The study assessed changes in physical function, muscular strength and pain. There were 16 patients who undertook BFRT and 19 patients who did MIRT. The study’s aim was to assess the safety and effectiveness of BFRT for improving muscular strength in symptomatic older adults with knee osteoarthritis (Harper, et al [4]). Inclusion criteria required patients to be over 60 years of age, have objective functional limitations, not be partaking in regular resistance training and have symptomatic knee osteoarthritis. Exclusion criteria included contraindications to tourniquet use (such as peripheral vascular disease), a systolic blood pressure of over 160 or under 100 mm Hg and absolute contraindications to the training or medical conditions that deemed it unsafe. Patients were deemed to have osteoarthritis if they had radiographic evidence of osteophytes, scored > 0 on the graded chronic pain scale and had a Kellgren–Lawrence grade ≥ 2 for the affected knee on a bilateral standing anterior–posterior radiograph. Thirty-three patients completed the study; one patient from the BFRT group and one from the MIRT group withdrew their consent to continue.
Three patients from each group (six total) stopped further participation during the training phase but decided to remain in the trial. A total of 81.4% of patients adhered fully to the BFRT training regime and 83.0% adhered fully to the MIRT training regime. This suggests that BFRT is tolerated well by osteoarthritic patients, suggesting that continued use of BFRT should not be an issue for patients when compared to MIRT [4]. There were 14 reports of knee pain that seemed likely or possibly related to the training regimes. Three of these occurrences were reported in the BFRT group and 11 were in the MIRT group. The study suggests that there were two serious adverse events in the BFRT group, with just one of these events related or potentially related to the study; there were three serious adverse events in the MIRT group. However, the study does not expand on what deemed these adverse events to be classified as serious or what led them to believe it was related to the training. These are important points to note as the goal is to keep pain to a minimum whilst still increasing strength [4]. The training in both groups involved supervised resistance exercise training three times a week. After a warmup, patients performed lower body strength training followed by flexibility and balance training. Standard isotonic resistance training equipment was used for the resistance exercises. The lower limb exercises included leg press, leg extension, leg curl and calf extension.
Participants underwent a familiarisation session prior to the start of the official training. This was to ensure they were using proper techniques for the exercises and so they could become accustomed to the machines used. Starting weights were determined by establishing each patients’ one-repetition maximum (1-RM) for leg press, leg extension, leg curl and calf extension. At the last session of the third, sixth, ninth and twelfth week, the participants’ 1-RM was remeasured. The weight required for participants to use in their training was then recalculated [4]. In the MIRT group, the resistance exercises mentioned were performed at 60% of the patients’ 1-RM. The BFRT group performed the resistance exercises at 20% of their 1-RM but with compression applied at the patients’ proximal thighs using pneumatic cuffs. The cuff pressure for each participant was calculated with the equation:
The restriction was sustained throughout each training exercise including rest times between sets. However, the cuff restriction was alleviated for the rest period when switching from one exercise to another. All exercises were performed to volitional fatigue. The issue with this is that the number of repetitions and effort put in by patients differs on an individual basis, which could have had an effect on the level of improvement [4].
Patients’ improvement was assessed using several tools and questionnaires. These included:
Dynamometer to assess torque/strength.
Timed walking speed over 400 m (ten laps of a 40 m course).
Visual analogue scale (VAS) used immediately after walking 400 m to assess patients’ current pain.
Western Ontario and McMaster Universities Arthritis Index (WOMAC) to measure pain related to the knees.
Short Physical Performance Battery (SPPB) to assess lower limb physical function. The patient is asked to perform several tests to assess physical function including balance tests, the gait speed test and the chair stand test. A score is calculated out of 12 with a higher score suggesting better physical function.
The disability component of the Late Life Function and Disability Instrument (LLFDI). The LLFDI (disability component) aims to self-assess physical function using 16 questions to assess frequency of task performance and perceived limitations to provide good indicators of the patient’s level of disability. The questions establish how often a patient performs an activity as well as the extent to which they feel limited while doing the activity. Scores are recorded on a scale of 0–100 (recorded separately for frequency and limitation) with higher scores suggesting better physical function [4].
The results below are shown with 95% confidence intervals in brackets for the mean differences reported in this study. Using the dynamometer, the mean change calculated using both groups after undergoing training for knee extensor peak torque at 60 degrees, 90 degrees and 120 degrees was found to be 9.96 (5.76, 14.16) Nm. The mean change between groups at 12 weeks for mean composite knee extensor peak torque when comparing BFRT to MIRT was 1.87 (−10.96, 7.23) Nm less. Therefore, we can say that knee extensor strength improved for both groups over the 12-week period. However, MIRT appears to improve knee extensor power (torque) more than BFRT [4]. The mean change calculated using both groups in the 400 m walk gait speed test was a reduction of 0.03 (−0.08, 0.01) m/s. The post-training change between groups for the 400 m walk gait speed test was a reduction of only 0.01 (−0.11, 0.09) m/s (BFRT compared to MIRT), suggesting both training methods are equally non-effective at improving gait speed based on this test [4]. The mean change to the SPPB calculated using both groups after undergoing training was an increase of 0.47 (−0.03, 0.97) points. However, post-training, the score for BFRT was 0.66 (−1.74, 0.42) points less than for MIRT. Considering that the maximum possible score for the SPPB is 12 and the minimum 0, a difference of 0.66 points would not be considered to validate MIRT as significantly better than BFRT for improving physical performance [4].
The mean change calculated using both groups for the frequency total for the LLFDI after undergoing training was −0.14 (−2.23, 1.94) points. Comparing points after training between groups showed that BFRT had 0.79 less points than MIRT. This shows that neither group was particularly successful at improving physical function upon self-assessment. Although BFRT seems to have negatively affected the LLFDI score post-training, the difference of 0.79 (−6.76, 5.17) points between BFRT and MIRT is so small on a scale of 0–100 that it does not seem significant [4]. The mean change calculated using both groups for the limitation total for the LLFDI after undergoing training was 4.36 points (0.06, 8.72). Comparing points after training between groups showed that BFRT had 6.60 (−18.99, 5.79) points less than MIRT. This shows that MIRT was superior to BFRT in improving the limitation total for the LLFDI score. The mean change calculated using both groups for the WOMAC pain scale was a decrease of 0.81 (−2.04, 0.42). Comparing points after training between groups showed that BFRT had 0.24 (−2.51, 2.98) points more than MIRT. However, given this small difference, we cannot say that BFRT causes less knee pain than MIRT [4]. The mean change calculated using both groups for total lean mass before and after training was 0.40 kg (−0.61, 1.40). Comparing points after training between groups showed that BFRT had 1.10 kg less than MIRT.
This suggests that MIRT is more effective at increasing lean mass than BFRT [4]. The mean change calculated using both groups for change in lower lean body mass was 0.71 kg (1.07, 0.36). Comparing points after training between groups showed that the BFRT group had gained a mean of 0.44 kg (−1.26, 0.39) less than the participants in the MIRT group. This suggests that although BFRT aided an increase in lower lean body mass, it was not as effective as MIRT. The mean change calculated using both groups for total body fat percentage was a decrease of 1.02%. Comparing points after training between groups showed that the participants in the BFRT group had a mean total body fat 1.12% more than the MIRT group. However, it is not mentioned in the study which method was used to calculate the lean mass – total body fat percentage or lower lean body mass [4]. As being overweight is a risk factor for osteoarthritis, it would seem beneficial for patients to undergo the training regime that causes the most weight loss. However, it should be noted that weight loss will not be a goal for all patients as some may already be underweight or have other medical conditions causing weight loss. In this pilot study, it does not appear that BFRT is any better than MIRT at reducing body fat or increasing lean muscle mass. The results show that BFRT is a safe alternative to MIRT to improve pain and function in older osteoarthritic patients; however, this should not be over-analysed as it is a pilot study with a small number of participants. From the results above, it does not seem that BFRT is more effective than MIRT; indeed, many of the tests, such as the limitation total for LLFDI and knee extensor peak torque, suggest that MIRT shows a better outcome. A larger scale randomised control trial will be required to fully ascertain if BFRT is an alternative to MIRT [4].
Discussion
Both studies looking at BFRT in patients with osteoarthritis over a course of 12 weeks showed that BFRT was a safe and effective way to improve function and strength when compared to HIRT or MIRT, whilst limiting pain caused to the patient. However, these are both small studies: one has 48 patients with an age range of 50–65 years [3] and the other had 35 patients with a mean age of 67.2 years4. The 2019 Harper et al. study was only a pilot clinical trial; larger scale studies with a wide age range and for a longer period of time will need to be conducted to fully verify how effective BFRT is at improving function and strength in those with osteoarthritis. The efficacy of using BFR post-knee surgery and for osteoarthritis is uncertain as there is a scarcity of studies and the application of BFR often differs, for example, in regard to limb occlusion pressures, the timing of the initiation of BFR, the frequency of exercise and the angle at which certain exercises are performed with BFR. In the studies mentioned above, the training methods and use of BFR varied, making it difficult to directly compare the effectiveness of BFR. For example, when we compare the training methods used in each of the osteoarthritis studies, they show differences in the exercises used, the frequency of training per week, the occlusion pressures used, the number of repetitions per set and the time at which 1-RMs are reassessed. We believe that the advantages of being able to reduce muscle atrophy and improve muscle strength for individuals with osteoarthritis using only low-resistance exercises outweigh the risks of using BFR, especially as many of the risks associated with BFR can be reduced with the recommended tourniquet equipment and proper application of the devices (De Phillipo, et al. [5]).
Conclusion
BFRT when used correctly has the potential to prevent muscle atrophy as well as improving muscle strength for patients who have knee osteoarthritis. Using standardised training programmes with similar methods for acquiring occlusion would allow for direct comparison of studies against each other and help to identify whether BFRT is truly an intervention that will produce positive results. Further research with larger cohorts of patients is required to fully assess whether BFRT is a valid alternative to improve strength and function and reduce atrophy in patients with knee osteoarthritis. If further evidence supports the findings found in this paper then BFRT should be used more widely in practice for patients with osteoarthritis.
References
- Takarada Y, Takazawa H, Sato Y, Takebayashi S, Tanaka Y, et al. (2000) Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J Appl Physiol 88(6): 2097-2106.
- Matthew Buckthorpe, Giovanni La Rosa, Francesco Della Villa (2019) RESTORING KNEE EXTENSOR STRENGTH AFTER ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION: A CLINICAL COMMENTARY. Int J Sports Phys Ther 14(1): 159–172.
- Rodrigo Branco Ferraz, Bruno Gualano, Reynaldo Rodrigues, Ceci Obara Kurimori, Ricardo Fuller, et al. (2018) Benefits of Resistance Training with Blood Flow Restriction in Knee Osteoarthritis. Medicine & Science in Sports & Exercise 50(5): 897-905.
- Sara A Harper, Lisa M Roberts, Andrew S Layne, Byron C Jaeger, Anna K Gardner, et al. (2019) Blood-Flow Restriction Resistance Exercise for Older Adults with Knee Osteoarthritis: A Pilot Randomized Clinical Trial.
- Nicholas N De Phillipo, Mitchell I Kennedy, Zachary S Aman, Andrew S Bernhardson, Luke O Brien, et al. (2018) Blood Flow Restriction Therapy After Knee Surgery: Indications, Safety Considerations, and Postoperative Protocol. Arthrosc Tech 7(10): e1037–e1043.

 Research Article
Research Article