Abstract
Digital prosthetic workflows may significantly increase the efficiency, predictability, and patient acceptance of clinical protocols to transition failing dentitions into an implant-supported fixed complete rehabilitation. This report illustrates the application of a recently described advanced integrated prosthetic digital workflow (Sobczak Concept®) in a series of patients and indications. The workflow was based on prosthetic wax-ups built and updated throughout the workflow from multiple preand intra-surgical full-arch intraoral scans. A key feature was based on combining digitally smile-designed provisional wax-ups with post-placement anatomically driven waxing of the cervical prosthetic contours. This combination allowed designing and adapting aesthetic concepts based on well-established macro-and micro-aesthetic design principles, validating them directly with the patient, and delivering them in a natural-teeth-like, pink-free anatomically adapted prosthesis for a versatile range of indications.
Keywords: Immediate Placement; Immediate Loading; Full-Arch Restoration; Cad Cam Technology; Digital Implant Dentistry
Abbreviations: DSD: Digital Smile Design; CBCT: Cone-Beam Computer Tomography; IOS: Intraoral Scan; IFCDs: Implant-Fixed Complete Dentures; FCZ: Full-Contour Monolithic Zirconia
Introduction
Implant-fixed complete dentures (IFCDs) are well established for the immediate rehabilitation of edentulous patients [1]. Selecting an adequate treatment scheme represents one of the most important factors for the long-term clinical success of IFCDs [2]. This selection requires considering a wide range of objective clinical parameters, including anatomic, medical, technical, mechanical, and biological characteristics [2-4]. In addition, subjective patientperceived outcomes, including preferences and satisfaction, have recently gained equal importance in evaluating final treatment outcomes [5-7]. Depending on the interarch space and the dentogingival transition line, the overall prosthetic design of IFCDs has been traditionally broadly classified into crown-only white bridges or white–pink hybrid prostheses consisting of crowns and pink gingiva [8]. While this classification has proven useful to provide general guidance regarding prosthetic design and esthetics, more specific design guidelines and evaluation criteria for the aesthetic outcomes of IFCD treatments, remain pending [3]. The digitalization of prosthetic workflows and the introduction of new materials, e.g., full-contour monolithic zirconia (FCZ), have recently triggered a substantial transformation of prosthetic design approaches [3,9]. Digital smile design allows, e.g., to visualize the prosthetic design of IFCDs in context to the patient’s smile symmetry and modify and validate its esthetic aspects online and in real-time based on direct patient input [10,11]. Furthermore, techniques have emerged that allow adapting the cervical aspects of IFCDs with a high level of detail to the local soft and hard tissue anatomic preconditions.
Such approaches have been shown to deliver IFCDs with natural, teeth-like, and individually adapted designs [12,13]. In the absence of remaining dentition, these techniques can be used to fully redesign complete dental arches according to well-established functional and aesthetic design principles [10,14]. All of this may render the design approaches towards full-arch prosthesis more flexible and patient-centered when compared to the traditional approaches. In a recent publication by this group, an advanced digital workflow for accurate and efficient immediate full-arch restoration with an aesthetically and anatomically adapted natural tooth-like prosthesis has been presented [14]. This manuscript illustrates the application of this workflow to a range of anatomic conditions and indications. Specifically, its application in patients displaying varying levels of alveolar atrophy and with various dental restorative preconditions will be presented.
Materials and Methods
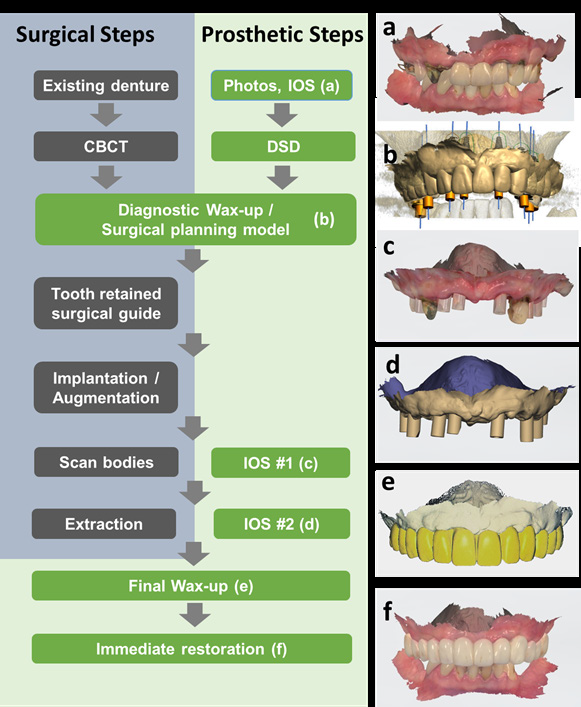
This case report describes the application of an integrated prosthetic workflow for the rehabilitation of four adult patients. All patients consented to IFCD treatment. None of the patients displayed any medical or psychological condition contributory to implant treatment. All patients displayed varying levels of remaining maxillary dentition indicated for extraction. Treatments were provided in a private clinic center (Sobczak Clinical Centre, Radosc, Poland) using the advanced, fully digital restorative protocol (Sobczak Concept®) illustrated in Figure 1. The detailed implant restorations were planned based on CBCTs scans (HyperionX9, MyRay, Imola, Italy) and diagnostic wax-ups (Implant studio, 3Shape A/S, Copenhagen, Denmark). The latter were derived from pre-treatment IOSs (3Shape TRIOS®, 3Shape A/S, København, Denmark) in close bite comprising the maxilla-mandibular relation (Figures 1a & 1b). The coronal and esthetic aspects of the diagnostic wax-ups were optimized based on frontal photographs using digital smile design (DSD) (in-CAD Smile Creator, exocad GmbH, Darmstadt, Germany). They were further used to examine the maxilla-mandibular relation and diagnose any required general or local soft or hard tissue augmentative or resective procedures. The prosthetic models were refined and finalized chair-side postimplant placement by using intra-surgical intraoral scans after mounting screw-retained abutments (SRAs) (titanium abutments, Institut Straumann AG, Basel, Switzerland) and scan bodies (CARES®, Institut Straumann AG, Basel, Switzerland). Residual dentition was strategically temporarily left in situ (Figures 1c & 1d) to facilitate the registration of individual IOSs and establish a geometric relationship between the diagnostic and final wax-ups (Exocad, DentalCAD, exocad GmbH, Darmstadt, Germany). The latter were finalized by adapting the soft-tissue interfacing cervical aspects of the prosthetic framework considering actual implant positions and the resulting post-placement soft-tissue contours and thickness [15]. Provisional restorations were chair-side printed and delivered on the day of implant placement (CARES® C Series, Institut Straumann AG, Basel, Switzerland). Final in-house milled (Ceramill®, motion2, Amann Girbach AG, Rankweil, Austria) multilayer zirconia bridges (IPS e.max ZirCAD Prime, Ivoclar Vivadent AG, Lichtenstein) were delivered at 6 months post-surgery.
Results
Case 1
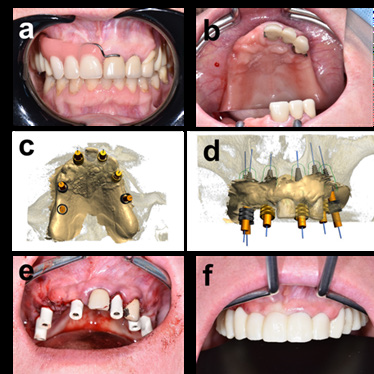
Case 1 illustrates the treatment of a young, 41-year-old male patient with failing maxillary dentition and malocclusion, who presented in our clinic with a chief complaint of poor aesthetics, pain, and progressive deterioration of masticatory function. Intraoral examination revealed multiple failing maxillary teeth affected by carious decay down to the root and pulpitis. CBCT scans indicated adequate overall bone quantity. As illustrated in Figure 1a, the patient displayed a lateral canine guidance-related malocclusion. Under consideration of the young age of the patient and expected elevated masticatory forces, a first-molar-to-first molar restoration supported by 8 implants was defined [16,17]. BLT (Positions 12, 15, 21, and 24) were combined with BLX implants (Positions 14, 17, 22, and 27) (Institute Straumann AG, Switzerland) for optimal immediate stability [18,19]. Implant lengths and implant diameters ranged from Ø3.3 x 12mm in anterior positions to Ø4.5 x 8mm in posterior positions and were defined based on locally available bone volumes. Figure 1C shows the clinical situation after tooth extraction and immediate implant placement with cuspids still left in situ to register individual scan and waxing model data sets [20,21]. Figure 1e illustrates the restored maxilla-mandibular relation and raised occlusal vertical dimensions after immediate provisionalization [12].
Note: DSD: digital smile design, CBCT: cone-beam computer tomography, IOS: intraoral scan.
Figure 1: Treatment scheme comprising the applied surgical and prosthetic steps. Individual steps of the prosthetic procedure are illustrated in green, and surgical steps are illustrated in grey. Pictures illustrate the individual prosthetic data sets, including
a) a: Pre-treatment IOS in close bite,
b) b: Diagnostic wax-up in relation to the planned implant restoration,
c) c, d: IOS#1 and IOS#2 after placement of implants, SRAs and scan bodies before and after strategic extraction of remaining teeth, respectively. These remaining teeth were used to register pre-treatment IOS, IOS#1, and IOS#2 and were used as landmarks to match diagnostic wax-ups and the actual implant restoration.
d) e: Final wax-up after chair-side adaption of the cervical contours of the prosthetic framework to the resulting postplacement soft-tissue contours.
e) f: IOS in close bite 1 week after delivery of the immediate provisional restoration.
Case 2
Figure 2: Case 1: Immediate maxillary full-arch restoration in a young patient with failing maxillary dentition and malocclusion.
a) Frontal photograph illustrating the esthetic situation and lip line prior to treatment,
b) Clinical intraoral situation of the patient without conventional partial denture prior to treatment.
c) Occlusal view after implant placement and restoration with screw-retained abutments (SRAs) and scan bodies. Canines were temporarily left in situ as landmarks to match individual intraoral scans
d) Frontal photographs after immediate delivery of the provisional restoration.
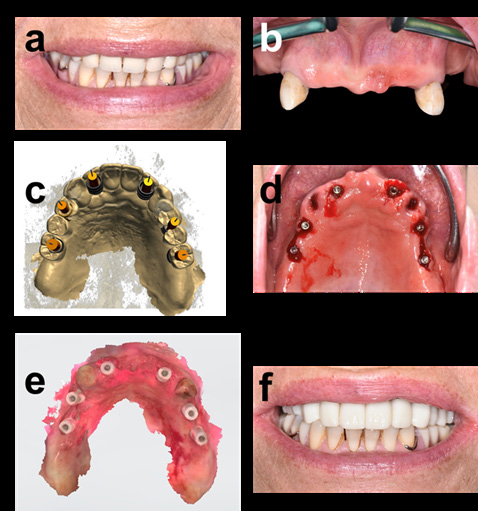
Figure 3: Case 2: Immediate full-arch restoration of a patient presenting posterior bone atrophy and antero-vestibular bone deficiency.
a) a: Retracted frontal view illustrating the situation with conventional removable partial prosthesis prior to treatment. b) b: Occlusal view on remaining dentition and atrophied distal alveolar crest. c) c,d: Occlusal and frontal view planned implant positions. d) e: Clinical situation at IOS#1, i.e., after implant placement, local bone augmentation in zone 11, and SRAs and scan bodies placement. Teeth 21 and 23 were temporarily left in situ. e) f: Frontal view 1 week after immediate provisionalization illustrating the overall anatomically and aesthetically driven restorative concept.Case 2 describes the treatment of a 53-year-old female with a moderately atrophied posterior maxilla and a local bucco-anterior bone deficiency. The patient presented with a chief complaint of poor aesthetics and fit of her upper conventional partial denture (Figure 2a). Dental examination and diagnostic CBCT revealed residual dentition in positions 21 to 23, a moderately atrophied posterior edentulous alveolar ridge, and a buccal bone deficiency in the anterior zone (position 11) (Figures 2b & 2d). The aesthetic evaluation indicated a regular smile line at the dento-gingival margin. A first-molar-to-first-molar restoration supported by 6 BLT implants (Institut Straumann AG, Switzerland) was planned (Ø3.3 mm, L:10, and 12 mm; positions 12, 14, 16, 22, 24, and 26). Distal implants were placed slightly medially to compensate for the posterior atrophy. Anterior implants were angulated to ensure adequate engagement with the cortical bone for optimum primary stability. Horizontal bone augmentation using Xenograft and a Collagen membrane (Cerabone/Collprotect, Institut Straumann AG, Switzerland) was performed to compensate for the anterovestibular bone deficiency [22,23]. Figure 2e illustrates the clinical situation after implant placement, bone augmentation, and placement of scan bodies with teeth 21 and 23 left temporarily in situ as landmarks for individual intraoral scan data registration [11]. The comparison of pre-and 1-week post-treatment situations in Figures 3a and f illustrates the applied changes and adaptions in teeth shape and form to the local soft and hard tissue anatomy. Specifically, teeth in the anterior and posterior positions were slightly prolonged to improve the soft tissue adaptation and compensate for the moderate posterior atrophy without disrupting the patient’s overall tooth phenotype.
Case 3
Figure 4: Case 3: Immediate full-arch restoration of a patient with a distally atrophied maxilla.
a) Aesthetic assessment indicating a low smile line below the dento-gingival margin.
b) Frontal view of the maxilla presenting 2 residual canines, signs of local denture-induced hyperplasia in the frontal alveolar aspect, and distal maxillary atrophy.
c) Prosthetic and surgical restorative plans of a first-molar-to-first-molar prosthetic framework supported by 6 implants in occlusal view.
d) Overlayed visualization of pre-and post-implant placement IOS and IOS#1 visualizing possible soft tissue anatomic contour changes for the cervical prosthetic contour planning.
e) Occlusal view after implant placement. Soft tissue incision between the distal implants and release of a mucoperiosteal flap before contour augmentation.
f) Frontal view of the patient 1-week post-treatment illustrating the improved smile and incisal lines providing the patient with a subjective younger smile typology.
Case 3 illustrates the treatment of a 61-year old female patient (64 years old) with local posterior maxillary atrophy. The patient addressed herself to the clinic, requesting a more permanent, natural teeth-like restoration without palatal coverage and with improved hold. As evidenced in Figure 3a, the patient presented a low smile line covering the dento-gingival margin. Oral examination indicated local signs of gingival denture-induced hyperplasia (Figure 4b). Osseous alveolar dimensions in the frontal aspects were adequate. However, distal aspects of her alveolar ridge were moderately atrophied with a sharp knife-edged morphology. Based on provisional wax-ups and virtual planning models, a first-molarto- first molar restoration on 6 implants in positions 12, 14, 16, 22, 24, and 26 was planned (Figure 4c). The implant restoration was based on 4 anterior BLT implants (Ø 3.3mm x 12mm) and 2 posterior short implants (position 16: BLT, Ø4.1x8mm; position 26:BLX, 3.75x6mm), avoiding prosthetic cantilevers [24-26]. Horizontal alveolar contours between the distal implants were bilaterally augmented to compensate for missing tissue support using Xenograft combined with a Collagen membrane (Cerabone/ Collprotect, Straumann, Switzerland) (Figure 4d). Overlays of preand immediate post-operative IOSs were used to identify changes in the overall soft-tissue anatomy to design the cervical prosthetic contours. Figure 4f shows the patient’s smile appearance 1 week after immediate provisionalization. The comparison between preand post-treatment photographs in Figures 4a & 4f illustrates the patient’s aesthetic smile line changes. Specifically, upper crowns were slightly lengthened, and lip support was increased. These modifications improved the ratio between revealed upper and lower crowns, which resulted in a typologically younger aesthetic smile phenotype.
Case 4
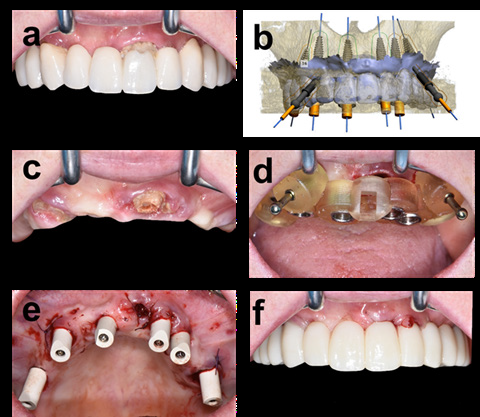
Figure 5: Case 4: Transitioning a failing conventional restoration into a fixed immediate full arch implant restoration.
a) Failing conventional restoration prior to treatment.
b) Digital wax-up of the planned restoration.
c) Frontal view after conventional restoration removal and abutment incisor fracture.
d) Frontal view after placement of surgical guide and
e) After placement of implants and restoration with scan abutments.
f) Frontal view after immediate provisionalization.
Case 4 illustrates the immediate transition of a failing conventional tooth-borne restoration into an IFCD. The patient, a 56-year-old female, was referred with a complaint of pain and increasing mobility of her restoration. Zones around abutment teeth 21 and 15 displayed acute inflammation and suppuration (Figure 5a). The existing restoration’s maxillomandibular relationship, OVD, and aesthetic aspects were evaluated as optimal. The design of the existing restoration was directly replicated in the fixed restoration after minimal adjustments to the emergence and angulation of the cuspid crowns (Figure 5b). The patient displayed adequate alveolar dimension to support a first-molar-to-firstmolar restoration on 4 straight anterior and 2 17°-tilted posterior implants (BLT, Ø3.3x12mm, Institut Straumann AG, Switzerland). Surgical guide placement was adversely affected by the fracture of the central incisor in position 11 upon removal of the existing restoration. This unforeseen event reduced the retention to two anchoring pins (Figure 5d). As indirectly verified by IOS#1 after removing tooth remnants, placing implants, and installing scan bodies, its positioning was not significantly compromised (Figure 5e). In this case, palatal rugae and posterior maxillary tuberosities were used as landmarks for the registration of individual IOSs. The resulting final wax-up was obtained by adjusting the cervical contours and connecting geometries of the prosthetic framework to the resulting soft-tissue anatomy and actual implant positions. This chair-side prosthetic planning allowed to efficiently transition the failing conventional restoration into an immediate implantborn fixed restoration with immediate passive fit despite the experienced intra-surgical complications.
Discussion
The presented clinical cases illustrate the capabilities of modern advanced digital workflows to accurately, efficiently, and robustly deliver aesthetically and anatomically adapted IFCDs in a wide range of indications [9]. The applied digital workflow has been recently described for the treatment of fully edentulous cases [14]. One of the most important features of the presented workflow is its capability to individualize the prosthetic framework to the patient’s micro-and macro-aesthetic appearance and local soft and hard tissue anatomic preconditions. This important capability is based on combining multiple individually described prosthetic techniques and directly integrating the resulting prosthetic procedures into the surgical workflow. The advantages of designing the visible coronal aspects of immediate IFCDs from a facial and aesthetic perspective have been brilliantly illustrated, e.g., by Coachman et al. [11]. The micro-and macro-aesthetic principles for defining teeth sizes, shapes, and positions and the overall form of the dental arch in relation to smile lines and face symmetries have been well established and represent the basis of digital smile design (DSD) [10,27].
One of the major advantages of modern DSD routines, when applied as part of IFCD treatments, is the possibility to redesign dental arches according to these principles fully. Virtualization further allows to directly visualize and modify the aesthetic concepts in real-time and in close cooperation with the patient himself. This direct patient feedback as part of DSD is routinely implemented as part of our procedures and approximately XY % of patients make active use of this possibility In addition, the immediate provisional itself was also actively exploited for patient feedback, and its transition into the final restoration was actively used to potentially adapt the aesthetic appearance of the prosthetic design for the final restoration. Despite this intrinsic possibility for aesthetic design changes, the evaluation of over 350 patient records indicated that 97% of treated patients in our clinics actively consented to directly transfer and replicate the aesthetic aspects of the provisional into the final restoration with little or no modification. With regards to adapting the cervical aspects of the prosthetic framework to the local soft and hard-tissue anatomy, Pozzi et al. and Salama et al. have presented digital techniques to plan and adapt soft and hard-tissue anatomical crestal contours to ideally support an anatomically designed pink free implant born restoration (FP-1 and FP-2) [13,15]. This approach was modified as part of our workflow by planning and modifying the cervical aspects of the prosthetic framework to the resulting post-placement 3D anatomical hardand soft tissue contours and implant positions. Specifically, the prosthetic contours of the prosthetic wax-up were planned for direct and tight soft tissue contact. Soft tissue thicknesses between the prosthetic contour and the underlying alveolar bone were planned at≥3 mm to prevent any soft tissue complications [15].
As further illustrated by case descriptions 2 and 3, local bone grafting was performed to improve the prosthetic framework tissue support. The requirement for such procedures was identified at the diagnostic wax-up stage and included in the surgical plans. Likewise, whenever possible soft tissue architectures were kept intact to facilitate the cervical prosthetic planning using guided, preferably flapless implant placement. Ideal planning of regenerative procedures and cervical soft tissue contours at the stage of the diagnostic waxing process also consistently considered post-extraction physiological alterations of the soft and hardtissue contours. The general typology of such changes and the factors influencing them, e.g., the crestal bone wall and soft tissue phenotypes, have been previously described [28,29]. To our knowledge, this is the first report that describes the combination of pre-treatment DSD and anatomically driven post-placement prosthetic contouring to IFCD treatments as part of a fully digital workflow. Regarding overall prosthetic design, it also needs to be acknowledged that the presented cases were classified as teethonly defects that allowed for a design of a white bridge (FP-1 and FP-2) [8]. However, the capability of advanced virtual prosthetic planning models as presented herein and its capability to fully redesign dental arches according to well-established functional and aesthetic design principles may also allow the delivery of white bridges to indications traditionally regarded as combined defects requiring pink esthetics (FP-3) [10].
Accurate scanning and an error-free combination of multiple direct digital full-arch scans were pivotal for the accurate planning of the final wax-up [9,30]. These scans spanned the entire arch and were required to derive a waxing model with accurate information on the soft tissue contour and actual implant positions. The anatomical characteristics of partially edentulous arches and the intrinsically associated relatively low number and relative distance between characteristic anatomic landmarks rendered the registration of individual pre- and post-placement scans and the diagnostic wax-up demanding [30]. In the presented procedures existing dentition was systematically left temporarily in situ as part of a strategic extraction protocol to overcome these limitations and provide distinct landmarks for scan alignment [20]. Further, Palatine rugae and tuberosities were also consistently used to ensure adequate scan alignment and verify individual scan accuracy. At the same time, precautions were taken to limit the impact of any factors affecting scan accuracies like tongue movement or the limited space in the distal scanning regions [9]. Another important feature of the workflow was the combination of pre-placement surgical planning and integrated post-placement verification of implant positions at the diagnostic and final wax-ups stages, respectively [21,31]. This feature rendered the immediate prosthetic fit accurate and the workflow robust towards intra-surgical adverse events. Due to the limited capability of CBCT scans to deliver quantitative bone density information, implant positions were mainly planned based on bone volume [32]. Primary stability was always simultaneously verified using insertion torque values. Further, the implant type was flexibly varied, between classical tapered bone level (BLT) implants for regular osseous conditions and novel BLX implants for immediate placement and in conditions with poor bone quality. This latter implant type displays a more pronounced protruding thread geometry for increased engagement with low-density bone [19]. To our knowledge, this is the first report illustrating the combined use and variation of implant types to maximize the primary stability of IFCD treatments. Finally, workflow robustness may be considered another important factor, specifically when considering the complex nature of IFCD treatments. Tahmaseb et al. reported that the rate of intraoperative and prosthetic complications of digital surgical procedures might reach 36.4% [33]. Although this relatively high rate seemed to be closely related to the technology learning curve, the successful and accurate restoration of patient 4 illustrates how the presented workflow may help mitigate even pronounced intrasurgical complications [34].
Conclusion
Advanced integrated prosthetic workflows based on pre-and post-placement direct digital impressions represent a powerful methodology to robustly deliver immediate chairside manufactured with optimal immediate passive fit in a wide range of indications. The combination of digital smile and anatomically driven cervical prosthetic design provides access to patient-centered, aesthetically optimized, natural pink-free restorative designs that may have been classically regarded as combined defects requiring pink esthetics.
Acknowledgment
The authors would like to thank Novonexile AG for its editorial support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pera P, Menini M, Pesce P, Bevilacqua M, Pera F, et al. (2018) Immediate Versus Delayed Loading of Dental Implants Supporting Fixed Full-Arch Maxillary Prostheses: A 10-year Follow-up Report. Int J Prosthodont 32(1): 27-31.
- Caramês JMM, Marques DN da S, Caramês GB, Francisco HCO, Vieira FA (2021) Implant Survival in Immediately Loaded Full-Arch Rehabilitations Following an Anatomical Classification System-A Retrospective Study in 1200 Edentulous Jaws. J Clin Med 10(21): 5167-5189.
- Schwarz F, Schär A, Nelson K, Tobias Fretwurst, Tabea Flügge, et al. (2021) Recommendations for Implant-Supported Full-Arch Rehabilitations in Edentulous Patients: The Oral Reconstruction Foundation Consensus Report. Int J Prosthodont 34: s8-s20.
- Chrcanovic BR, Kisch J, Larsson C (2020) Retrospective evaluation of implant‐supported full‐arch fixed dental prostheses after a mean follow‐up of 10 years. Clin Oral Impl Res 31(7): 634-645.
- Wittneben J, Wismeijer D, Brägger U, Joda T, Abou Ayash S (2018) Patient‐reported outcome measures focusing on aesthetics of implant‐ and tooth‐supported fixed dental prostheses: A systematic review and meta‐analysis. Clin Oral Impl Res 29(16): 224-240.
- Duong HY, Roccuzzo A, Stähli A, Salvi GE, Lang NP, et al. (2022) Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Periodontology 2000 88(1): 201-237.
- De Bruyn H, Raes S, Matthys C, Cosyn J (2015) The current use of patient-centered/reported outcomes in implant dentistry: a systematic review. Clin Oral Impl Res 26(11): 45-56.
- Bedrossian E, Sullivan RM, Fortin Y, Malo P, Indresano T (2008) Fixed-Prosthetic Implant Restoration of the Edentulous Maxilla: A Systematic Pretreatment Evaluation Method. Journal of Oral and Maxillofacial Surgery 66(1): 112-122.
- Michelinakis G, Apostolakis D, Kamposiora P, Papavasiliou G, Özcan M (2021) The direct digital workflow in fixed implant prosthodontics: a narrative review. BMC Oral Health 21(1): 37-61.
- Blatz MB, Chiche G, Bahat O, Roblee R, Coachman C, et al. (2019) Evolution of Aesthetic Dentistry. J Dent Res 98(12): 1294-1304.
- Coachman C, Calamita MA, Coachman FG, Coachman RG, Sesma N (2017) Facially generated and cephalometric guided 3D digital design for complete mouth implant rehabilitation: A clinical report. J Prosthet Dent 117(5): 577-586.
- Pozzi A, Arcuri L, Moy PK (2018) The smiling scan technique: Facially driven guided surgery and prosthetics. J Prosthodont Res 62(4): 514-517.
- Salama MA, Pozzi A, Clark WA, Tadros M, Hansson L, et al. (2018) The “Scalloped Guide”: A Proof-of-Concept Technique for a Digitally Streamlined, Pink-Free Full-Arch Implant Protocol. Int J Perio Res Dent 38(6): 791-798.
- Sobczak B, Majewski P (2022) An Integrated Fully Digital Prosthetic Workflow for the Immediate Full-Arch Restoration of Edentulous Patients-A Case Report. IJERPH 19(7): 4126-4137.
- Pozzi A, Arcuri L, S Block M, K Moy P (2021) Digital assisted soft tissue sculpturing (DASS) technique for immediate loading pink free complete arch implant prosthesis. J Prosthodont Res 65(1): 119-124.
- Mioche L, Bourdiol P, Peyron MA (2004) Influence of age on mastication: effects on eating behaviour. Nutr Res Rev 17(1): 43-54.
- Daudt Polido W, Aghaloo T, Emmett TW, Taylor TD, Morton D (2018) Number of implants placed for complete‐arch fixed prostheses: A systematic review and meta‐analysis. Clin Oral Impl Res 29(16): 154-183.
- Dard M, Kuehne S, Obrecht M, Grandin M, Helfenstein J, et al. (2016) Integrative Performance Analysis of a Novel Bone Level Tapered Implant. Adv Dent Res 28(1): 28-33.
- Francisco H, Finelle G, Bornert F, Sandgren R, Herber V, et al. (2021) Peri-implant bone preservation of a novel, self-cutting, and fully tapered implant in the healed crestal ridge of minipigs: submerged vs. transgingival healing. Clin Oral Investig 25(12): 6821-6832.
- Dada K, Pariente L, Daas M (2016) Strategic extraction protocol: Use of an image-fusion stereolithographic guide for immediate implant placement. J Prosthet Dent 116(5): 652-656.
- Vandeweghe S, Vervack V, Dierens M, De Bruyn H (2017) Accuracy of digital impressions of multiple dental implants: an in vitro Clin Oral Impl Res 28(6): 648-653.
- Chen ST, Buser D (2009) Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants 24: 186-217.
- de Azambuja Carvalho PH, dos Santos Trento G, Moura LB, Cunha G, Gabrielli MAC, et al. (2019) Horizontal ridge augmentation using xenogenous bone graft-systematic review. Oral Maxillofac Surg 23(3): 271-279.
- Silva GC, Mendonça JA, Lopes LR, Jr JL (2010) Stress Patterns on Implants in Prostheses Supported by Four or Six Implants: A Three-Dimensional Finite Element Analysis. Int J Oral Maxillofac Implants 25(2): 239-246.
- Calvo Guirado JL, López Torres JA, Dard M, Javed F, Pérez Albacete Martínez C, et al. (2016) Evaluation of extrashort 4-mm implants in mandibular edentulous patients with reduced bone height in comparison with standard implants: a 12-month results. Clin Oral Impl Res 27(7): 867-874.
- Tabrizi R, Arabion H, Aliabadi E, Hasanzadeh F (2016) Does increasing the number of short implants reduce marginal bone loss in the posterior mandible? A prospective study. Br J Oral Maxillofac Surg 54(7): 731-735.
- Davis NC (2007) Smile Design. Dental Clinics of North America 51(2): 299-318.
- Chappuis V, Araújo MG, Buser D (2017) Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol 2000 73(1): 73-83.
- Chappuis V, Engel O, Shahim K, Reyes M, Katsaros C, et al. (2015) Soft Tissue Alterations in Esthetic Postextraction Sites: A 3-Dimensional Analysis. J Dent Res 94(9): 187S-193S.
- Wulfman C, Naveau A, Rignon Bret C (2020) Digital scanning for complete-arch implant-supported restorations: A systematic review. J Prosthet Dent 124(2): 161-167.
- Derksen W, Wismeijer D, Flügge T, Hassan B, Tahmaseb A (2019) The accuracy of computer‐guided implant surgery with tooth‐supported, digitally designed drill guides based on CBCT and intraoral scanning. A prospective cohort study. Clin Oral Impl Res 30(10): 1005-1015.
- Papadimitriou D, Salari S, Gannam C, Gallucci G, Friedland B (2014) Implant-Prosthodontic Classification of the Edentulous Jaw for Treatment Planning with Fixed Rehabilitations. Int J of Prosthodont 27(4): 320-327.
- Tahmaseb A, Wismeijer D, Coucke W, Derksen W (2014) Computer Technology Applications in Surgical Implant Dentistry: A Systematic Review. Int J Oral Maxillofac Implants 29: 25-42.
- Fang Y, Fang JH, Jeong SM, Choi BH (2019) A Technique for Digital Impression and Bite Registration for a Single Edentulous Arch: Virtual Bite Registration. Journal of Prosthodontics 28(2): e519-e523.

 Case Report
Case Report