ABSTRACT
Wernicke’s encephalopathy is an often-unrecognized disease that usually results from chronic alcoholism. Up to 50% of cases could be attributed to either prolonged parenteral nutrition, malignancy, AIDS, chronic malnutrition, or gastrointestinal tract surgery. We describe a case of a patient who presented with 3 days history of blurred vision and gait disturbance. On examination, she was moderately emaciated. There were no detectable lymph nodes. Abdominal, pulmonary, and cardiac examination was normal. Central nervous system examination revealed bilateral abducens nerve palsy, right-sided complete oculomotor nerve palsy, and left-sided partial oculomotor nerve palsy. She had horizontal diplopia of vision of near and far objects. The patient had an unstable gait with ataxia. CT angioscan of the brain was normal. Cerebral MRI of the brain was normal. The patient had a history of gastric sleeve surgery 3 months before presentation. Thiamin level was requested, and she was given thiamin supplement with multivitamin B supplement. Her symptoms improved and subsided by the second day of treatment. It is important to consider Wernicke’s encephalopathy in patients with neurological symptoms and a history of gastric sleeve surgery.
Keywords: Wernicke’s Encephalopathy (WE); Thiamine; Ophthalmoplegia; Mental Status Changes
Introduction
Wernicke’s encephalopathy is an often-unrecognized disease that usually results from chronic alcoholism [1]. Up to 50% of cases could be attributed to either prolonged parenteral nutrition, malignancy, AIDS, chronic malnutrition, or gastrointestinal tract surgery [2]. Because this disease may be less recognized and diagnosed by physicians in non-alcoholic patients, we report this case.
Case Presentation
We present the case of a 14 years old teenager reporting vision and gait disturbances. The patient reported blurred vision and unstable gait, which have started 3 days before presentation. At presentation, the patient was conscious, cooperative, and oriented swaying from side to side upon ambulation. Vital signs were normal with blood pressure 120/75 mmHg, O2 saturation of 98% on room air, a pulse of 86 bpm, and HGT of 105 g/dl. The patient denied any fever, gastrointestinal, respiratory, or urinary symptoms. She denied the occurrence of similar symptoms with any of her close contacts or relatives earlier. She denied any drug abuse and was assured she has had never consumed alcohol. The patient reported having several medical conditions: she has diabetes mellitus, hypothyroidism and has a history of gastric sleeve surgery for morbid obesity since 3 months before admission. The patient is on daily metformin 1000 mg daily and thyroxin 100 mcg daily. The patient reported being on a strict diet and losing about 23 kgs of her body weight since the operation. On the physical exam, she had horizontal diplopia on the vision of objects at short and long distances. The left pupil was non-reactive to light. Bilateral abducens nerve palsy was evident.
Complete oculomotor nerve (CN III) palsy was evident at the left eye while the right eye exam revealed partial oculomotor nerve palsy. The patient was ambulatory with an unstable gait and ataxia. No Babinski sign was evident. The patient had normal motor control of her upper and lower limbs and axial muscles. The examination of sensation was normal. The initial diagnosis was a possible aneurysm or tumor-induced compression of the optic chiasma and oculomotor nerves. ACT angioscan of the brain revealed no tumor, hemorrhage, or ischemia. A cerebral MRI with gadolinium proved normal with no clue of aneurysms, tumor compression, and hemorrhage. An EEG revealed normal brain activity. The patient denied any signs of epileptic seizures and headache. Laboratory workup showed normal complete blood count and differential except for hemoglobin of 11 g/dl and hematocrit of 34 %. Renal and liver function tests were normal. Chest X-ray was normal. Thiamin level was 0.3 ng/ml. The patient was given 1g of thiamin intravenous drip over 2 hours. The patient has been prescribed 100 mg of thiamin intramuscular injections for 2 days with multivitamin B tabs 3 times a day. The patient’s symptoms started to subside by the second day of treatment. The patient was kept on thiamin and multivitamin supplements for ten days. Her symptoms subsided.
Discussion
Thiamin is a cofactor for several enzymes in the Krebs cycle [3]. It is vital for carbohydrate metabolism in the pentose phosphate pathway [3]. A decrease in the activity of these enzymes due to lack of thiamin leads to increased build-up of toxin intermediate metabolites in areas of the brain. This induces damage to the brain and causes Wernicke’s encephalopathy. The acute onset and fast progression of symptoms to coma and death justify the urgency of such condition, and the need for fast diagnosis and treatment [4]. Although Wernicke’s encephalopathy is mainly diagnosed in alcoholic patients, nearly 50% of WE cases occur in non-alcoholics. In addition, to alcohol consumption, malnutrition, gastrointestinal tract surgeries, and malignancies such as acute leukemia, malignant lymphomas, gastric adenocarcinomas, and breast cancer have been associated with WE [5]. The diagnosis of WE is mainly clinical and can be confirmed by laboratory and radiological examinations. Symptoms of WE are mainly neurological and of acute onset. Although only seen in 16% of patients, a triad of gait unsteadiness, ophthalmoplegia, and mental status changes characterizes WE [6].
Mental status changes can range from acute confusion to apathy and inability to concentrate. Progression with no treatment leads to coma and death [6]. A thiamine blood concentration or measurement of the erythrocyte transketolase activity can confirm a presumptive diagnosis of WE [7]. MRI remains the most valuable method to confirm a WE diagnosis [8]. Findings on MRI usually include bilateral and symmetric involvement of Paramedian thalamic nuclei, mammillary bodies, periaqueductal grey matter, and periventricular region of the third ventricle. Most commonly, patients with WE show signal hyperintensities on FLAIR, diffuseweighted and T2-weighted sequences within the posteromedial thalami and surrounding third ventricle [9]. In this case, our patient revealed normal findings on MRI. The diagnosis was mainly clinical with no radiological findings. The immediate response to presumed WE is the parenteral administration of thiamine. Intravenous thiamine of 500mg infused over 30 minutes trice per day for 2 days with vitamin B supplements must be initially given. For additional five days, 500 mg of thiamine must be given intravenously or intramuscularly in combination with a vitamin B supplement [10]. Although rare, WE remains a medical emergency that demands the earliest possible diagnosis and treatment. Clinicians in nonalcoholic patients overlook it, which results in delayed treatment and symptoms’ progression into coma and death. The prognosis of WE with early diagnosis is favorable, as shown in this case where complete remission was attained with early treatment.
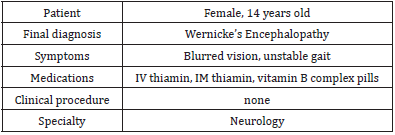
Summary of the Case
(Table 1).
Consent
The patient has signed a clear consent allowing the usage of the data related to her condition and the publication of this case report.
Ethical Consent
Ethical approval is not required to publish anonymous case reports.
Conflict of Interest
The authors have no conflict of interest regarding the publication of this case report.
Funding
None.
References
- Patel S, Topiwala K, Hudson L (2018) Wernicke's Encephalopathy. Cureus 10(8): e3187.
- Heye N, Terstegge K, Sirtl C, McMonagle U, Schreiber K, et al. (1994) Wernicke's encephalopathy-causes to consider. Intensive Care Med 20(4): 282-286.
- Bubber P, Ke ZJ, Gibson GE (2004) Tricarboxylic acid cycle enzymes following thiamine Neurochem Int 45(7): 1021-1028.
- Flynn A, Macaluso M, D'Empaire I, Troutman MM (2015) Wernicke's Encephalopathy: Increasing Clinician Awareness of This Serious, Enigmatic, Yet Treatable Disease. Prim Care Companion CNS Disord 17(3): 10.4088/PCC.
- Choi EY, Gomes WA, Haigentz M Jr, Graber JJ (2016) Association between malignancy and non- alcoholic Wernicke's encephalopathy: a case report and literature Neurooncol Pract 3(3): 196-207.
- Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, et al. (2020) Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol 38(9): 809-820.
- Leigh D, McBurney A, McIlwain H (1981) Erythrocyte transketolase activity in the Wernicke- Korsakoff syndrome. Br J Psychiatry 139: 153-156.
- Sparacia G, Anastasi A, Speciale C, Agnello F, Banco A (2017) Magnetic resonance imaging in the assessment of brain involvement in alcoholic and nonalcoholic Wernicke's encephalopathy. World J Radiol 9(2): 72-78.
- Sullivan EV, Pfefferbaum A (2009) Neuroimaging of the Wernicke-Korsakoff syndrome. Alcohol Alcohol 44(2): 155-165.
- Nishimoto A, Usery J, Winton JC, Twilla J (2017) High-dose Parenteral Thiamine in Treatment of Wernicke's Encephalopathy: Case Series and Review of the Literature. In Vivo 31(1): 121-124.

 Case Report
Case Report