SUMMARY
Septic arthritis consists of inflammation of a joint due to a generally bacterial infection, and to a lesser extent fungal or viral. The most commonly affected areas are the knee and hip. Early diagnosis (clinical and microbiological) is essential for the proper treatment of septic arthritis, since it can constitute a medical emergency, given its tendency to joint destruction [1,2]. The fundamental examination consists of the study of synovial fluid, with Gram staining, culture and antibiograma [3-8]. Blood cultures are also recommended, as they are profitable in nongonococcal arthritis, and in the diagnosis of arthritis of axial location, for the difficulty of taking the sample directly. If septic arthritis is suspected, the patient should be admitted, and treatment should be started immediately. Although treatment is variable, it usually focuses on systemic antibiotic administration and drainage of the affected articulation [5,6,9,10]. There is the case of a sanitary woman who, after an accidental puncture with a contaminated needle, develops septic arthritis. In the diagnostic process, the synovial fluid is not examined, and the patient is subjected to numerous changes in antibiotic treatment due to her poor clinical progress. Early diagnosis and proper management of septic arthritis cases is essential in the functional recovery of patients and in the prevention of possible complications [2-8]. Implementing standardized and evidencebased protocols for dealing with septic arthritis can be a very useful tool for healthcare professionals, allowing them to combine criteria and avoid undesirable consequences in the patient [11-19].
Keywords: Septic Arthritis; Complications; Antibiotic; Resistance; Clostridium
Introduction
Septic arthritis is an infectious process of the joint, secondary to colonization by a microorganism, with a tendency to suppuration and joint destruction [1-3]. The most frequent route of infection in any age is hematogenous, as the vascularization of the synovial membrane favors colonization in case of bacteremia [4,12]. Less common are: extension from a neighboring infection (osteomyelitis, bursitis), or by direct external inoculation (intraarticular infiltration, open fractures, surgery, etc.) [7].
• The most frequent germ in all age groups, and regardless of risk factors, is Staphylococcus aureus (50-60% of cases), with increasing importance of methicillin-resistant S.aureus (MRSA) in the context of nosocomial infection.
• The second globally most important microorganism is Streptococcus sp.
• S.epidermidis is the first microorganism in prosthetic infections and second after S.aureus in those associated with direct inoculation.
• In case of fractures, polymicrobial infection is common and, if associated with human bites, decubitus ulcers or intraabdominal abscesses, the involvement of anaerobes is common.
• Cat scratches or bites can cause arthritis by Pasteurella multocida.
• Gram-negative bacilli, including Pseudomonas, should be considered in elderly or patients with comorbidities (diabetes, immunosuppression, chronic corticosteroid therapy...) [4,7,12].
Depending on the Age
• Infants under 1 year of age: they become particularly important (apart from S.aureus): group B streptococci (agalactiae) and enterobacteria.
• Under 5 years: predominant S.aureus, group A streptococci and in case of not having been vaccinated, H.influenzae. • Adults: in addition to S.aureus and streptococci, Neisseria gonorrhoeae should be considered, but with decreasing importance in Europe [7,12].
Septic arthritis usually manifests as monoarticular arthritis. It most often affects lower limb load joints: first the knee, followed by the hip [1-3]. The main symptom is pain, with inflammation of the affected joint, limited mobility and frequent fever and general discomfort. In children younger than 1 year, the predominant symptomatology is sepsis, rather than local inflammation. Gramnegative arthritis may be more indolent and therefore harder to diagnose. Patients ADVP (addicted to drugs by parenteral route), present septic arthritis in the context of staphylococcal bacteremia, and it is common the involvement of the axial skeleton: vertebral joints, sternocllavicular and sacroiliac. The study of synovial fluid, resulting from infectious characteristics is essential for the diagnosis of septic arthritis [1,3,4,7,9,12].
- Turbidity or purulence
- Cell count usually >50,000 leukocytes/mm3, polymorphonuclear predominant
- Consumption of glucose
On the other hand, the cut-off point of 50,000 cells does not allow differentiating between microcrystalline and septic arthritis, since the former can frequently exceed this threshold. For etiological diagnosis, a Gram stain must be performed, which is positive in 75% of gram-positive cocos arthritis, but in less than 50% for gramnegative bacilli. The culture of the liquid is diagnostic in >90% and allows, by means of antibiogram, to specifically direct the treatment. Blood cultures are also recommended: they have a profitability of around 40-50% in the febrile process in nongonococcal arthritis, and in arthritis that affect the axial skeleton (so difficult to take a sample directly).
With regard to imaging tests [8]:
• Conventional Radiology: Although it is not used initially, it may be useful for the follow-up of the process (appearance of erosive lesions).
• Ultrasound: Allows to evaluate the presence of fluid in deep joints of difficult access, and guide arthrocentesis.
• CT and MRI: Allow, apart from the diagnostic evaluation, to determine the presence of osteitis or abscesses and, consequently, to evaluate the need for surgery.
• Isotopic Techniques: They are used less, due to their lower specificity, but they also have their usefulness in deep joints and help to make an early diagnosis in the first 24-48 h, especially in dubious diagnoses.
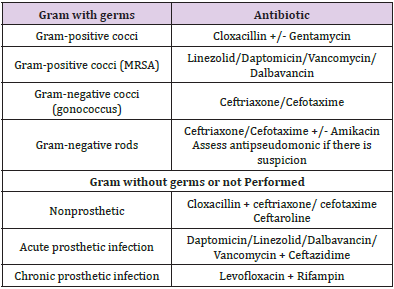
If septic arthritis is suspected, the patient should be admitted, and treatment should be started immediately, without waiting for the results of the joint fluid analysis. Treatment focuses on systemic antibiotic therapy and drainage of the infected joint [5,6,11,13,19]. If the joint is easily accessible, such as in the knee, daily arthrocentesis may be performed to drain the purulent material while the spill persists. Sometimes, it is advisable to resort to surgical drainage, by means of arthrotomy or arthroscopy, if the joint is not accessible (such as the hip), or if the clinical evolution is unfavorable and there are complications (abscess, septic material...) or persistently positive cultures at 5-7 days of correct antibiotic treatment. The choice of antibiotic is based on the result of Gram staining of the joint fluid and, failing that, empirical according to the characteristics of the patient. In these cases, antistaphylococcal and streptococcal treatment with Cloxacillin and Ceftriaxone is usually initiated. Gonococcal arthritis is usually treated for 7-10 days, streptococci or Haemophilus for 2-3 weeks, staphylococcus for 4 weeks and gramnegative bacilli for up to 6 weeks. Treatment should be intravenous for at least the first 2 weeks. Joint prosthesis infection usually requires removal of the prosthesis, cement and necrotic bone. However, if the infection is early (<3 months after implantation of the prosthesis) and the joint is stable, surgical cleaning (without prosthetic replacement) and prolonged antibiotic treatment may be performed (Table 1). There are other types of infectious arthritis, which have a clinical presentation with characteristics such as: gonococcal arthritis, virus, bone tuberculosis, brucellosis, spirochete arthritis [5,6,11,13,19].
Clinical Case
We present the case of a 23-year-old woman, a nurse, who draining a panadizo to a newborn along with another companion of the service, accidentally pricked, with a needle infected with pus, in the metacarpal joint-phalanx of the second finger of the right hand. They go to Occupational Health, which studies the background of the newborn and its parent, without finding relevant data; and activate the biological accident protocol, with blood analysis and relevant serology. On physical examination: the patient presents intense pain, inflammation of the finger and heat to palpation, with progressive functional impotence that limits the flexo-extension (Figure 1). The diagnosis is established by clinical suspicion and the treatment prescribed is: Enantyum+ Urbason 40 MG IM. It is recommended to come back for warning signs. The patient came after 48 hours due to worsening of the general condition, febrile fever and increased swelling and bloating of the index finger. Handheld RX is requested in PA and Oblicua projection and is diagnosed with arthritis and signs of cortical bone involvement. An ultrasound is performed to confirm the diagnosis of septic arthritis. As a treatment, Amoxicillin/Clavulanic 875 mg oral, passive movements and protection of the joint against blows are recommended. He came last 1 week for review, without improvement of the picture. The antibiotic is changed to Levofloxacin 500 mg orally, and the patient is re-summoned for review next week.
Again, he comes with the erythematous finger, perceiving improvement in inflammation, but not in pain to mobilization. The antibiotic is replaced by Cloxacillin 500 mg. After 5 days it begins with liquid stools with “strands” (12-14 stools/day) and blood content, together with a severe urticarial reaction with habones in soft tissues (lips and eyelids) and angioedema, without dyspnea or chest pain (Figure 2). He has no abdominal pain or vomiting. He has good oral tolerance, but diarrhea as soon as he swallows something. No syncope or dizziness. He went to the emergency room with a severe picture of dehydration and when suspected of “Clostridium Difficile Enteritis” a sample was sent to the micro laboratory. Angioedema and urticaria are controlled with the administration of Urbasón 80 MG IM and Polaramine 5mg/ml IM. Dacortin + Ebastel forte oral regimen. Fluid therapy is given. He is admitted to the Infectious plant and has a blood test that shows anemia, leukocytosis with left deviation and elevated CRP. The culture result is positive for Clostridium Difficile toxin, so Metronidazole is recommended. Last 1 week, when the number and consistency of stool improves, along with the inflammatory and painful signs of septic arthritis, is replaced by oral Vancomycin.
Antihistamine and corticosteroid doses are also progressively reduced to control hives, which manifest as pruritic erythematous lesions on the neck, face and trunk episodically or alternately during admission. Valued by Dermatology, it is diagnosed with “Toxicodermia secondary to antibiotic treatment”. When clinical stability is achieved, hand MRI (to corroborate the disappearance of the collection of purulent fluid and the signs of active arthritis) and colonoscopy (to rule out pseudomembranous colitis) are performed, and she is discharged from hospital. Later consultation is requested in the Allergology service.
Discussion
Infectious arthritis is an urgent pathology that requires an early diagnosis and an adequate antibiotic choice to reduce the risk of complications and accelerate the healing process [1-3,9,10,13,18]. In this clinical case it could be debated where should have started to act differently, to avoid the chain of events that complicate the septic arthritis suffered by the nurse. Perhaps she herself, at the time of the accidental puncture, should have taken a smear for culture, from that purulent liquid of the panadizo that was draining the newborn. Maybe she could have been helped by the partner holding the baby in the meantime. The Occupational Health Unit could have relapsed into the same smear, collecting data from the polluting source, rather than merely examining possible serologies. Or we could think that they themselves could have requested the puncture of the joint fluid to ensure the inoculated germ and the corresponding antibiogram, even if empirical treatment had been scheduled. Not even on his first visit to the emergency room he receives the Antibiotic Starter, but he is given a corticosteroid and an intramuscular analgesic. At no time is the patient aware of the exact infectious etiology of her septic arthritis, because she has not been tested for joint fluid.
The change of more than 4 antibiotics in approximately 6 weeks is the trigger of diarrhea due to Clostridium Difficile and as a final event, of a urticaria-like toxicodermia (probably secondary to Cloxaciline). We must insist that antibiotics are not safe, and we must raise awareness about the proper use of antibiotics. The misuse or abuse of these drugs can produce resistance, that is, the pathogens that cause the diseases (bacteria, fungi, viruses or parasites) become immune to the effect of these drugs, endangering the efficacy of treatment [10,13,18,19]. As a result, drugs become ineffective and infections persist in the body, increasing the risk of spreading to others. New coping mechanisms are emerging, threatening our ability to treat common infectious diseases, resulting in increased disability and deaths, and prolonged disease. This means that without effective antimicrobials to prevent and treat infections, interventions such as organ transplantation, cancer chemotherapy, diabetes treatment or major surgery (for example, caesarean sections or hip prostheses) will become very high-risk procedures.
If the microbial agent and antibiotic to which she was sensitive had been known from the beginning, the patient would probably have had an optimal and much earlier recovery. On the other hand, the incidence of Clostridium difficile infection has been increasing progressively in recent decades and is currently considered the most frequent cause of antibiotic-associated colitis, and the first cause of nosocomial diarrhea in developed countries; with great difficulty in its eradication in the hospital [14-17]. The changes induced by antibiotics in the gastrointestinal flora are the main predisposing factor. Although most antibiotics have been involved, the following pose the greatest risk:
- Cephalosporins (especially the 3rd generation)
- Penicillins (in particular Amphonin and Amoxicillin)
- Clindamycin
- Fluoroquinolone
Currently the treatment of choice is vancomycin or fidaxomycin by mouth. Metronidazole is no longer recommended as firstline therapy for C.difficile induced diarrhea, however, it may be used if Vancomycin or Fidaxomycin are not available. In addition, C. difficile infection leads to an increase in health expenditure in relation to the increase in hospital stay, with a higher morbidity and mortality, with all the diagnostic and therapeutic aspects that this implies. Hospitals should develop strategies for the prevention and control of C.difficile infection, which should include appropriate use of antibiotics. Finally, remember that the delay in establishing treatment in septic arthritis, may involve the evolution to osteomyelitis, the spread of germs and infection (potentially lethal sepsis), ankylosis, or the irreversible destruction of articular cartilage [18,19].
Conclusion
Septic arthritis is a medical emergency, which poses a potential risk to the patient’s life. Its rapid diagnostic and therapeutic approach are the pillars for an appropriate functional joint recovery, a fundamental objective of treatment [1-3,13]. Establishing protocols of action, with unified, standardized and evidencebased criteria, will help healthcare professionals manage septic arthritis cases and prevent the development of complications [18]. The fundamental points to consider in the management of septic arthritis in emergencies are: [5,6,13].
• Septic arthritis should be suspected in all acute monoarthritis until proven otherwise.
• Performing arthrocentesis should not be deferred as soon as the suspicion has been established. In this way we can analyze the joint fluid and submit it to culture and antibiogram.
• Unless a diagnosis of septic arthritis has been reasonably ruled out, the patient should receive empirical antibiotic therapy.
• Surgical cleaning should be performed as soon as possible on subjects in which needle joint drainage is incomplete or not feasible.
A clean-up in the operating room should be indicated if after conservative management there is no clinical improvement in the short term. In addition, we must attend to each patient with a holistic vision, which takes into account possible adverse drug reactions that may disturb the evolution of the disease and control the warning signs and symptoms that may arise [11,18]. Antibiotic resistance is one of the greatest public health challenges of our time. It is our job to raise awareness about the proper use of these [11]. This will also prevent and control Clostridium Difficile infections, reducing stay and health costs [11,14].
References
- Bolaños SMF (2017) Artritis septica. Revista Medica Sinergia 2(01): 22-25.
- Mateo Soria L, Olivé Marqués A, García Casares E, García Melchor E (2009) Artritis séptica politópica: analisis de 19 casos. Reumatol Clinic 5(1): 18-22.
- Real Delor RE, Martínez Giménez EM (2020) Características clínicas de las artritis sépticas de pacientes adultos internados del Hospital Nacional entre los años 2015 y 2019. 12(1): 14-27.
- Echeverri-Toro LM, Castañeda L, Agudelo CA (2019) Artritis septica por Streptococcus equi: reporte de un caso y revisión de la literatura. Infect 23(4): 402-404.
- Wang J, Wang L (2021) Novel therapeutic interventions towards improved management of septic arthritis. BMC Musculoskelet Disord 22(1): 530.
- Boff D, Crijns H, Teixeira MM, Amaral FA, Proost P, et al. (2018) Neutrophils: Beneficial and Harmful Cells in Septic Arthritis. Int J Mol Sci 19(2): 468.
- Jin T, Mohammad M, Pullerits R, Ali A (2021) Bacteria and Host Interplay in Staphylococcus aureus Septic Arthritis and Sepsis. Pathogens 10(2): 158.
- Fatima F, Fei Y, Ali A, Mohammad M, Erlandsson MC, et al. (2017) Radiological features of experimental staphylococcal septic arthritis by micro computed tomography scan. PLoS One 12(2): e0171222.
- Pyo JY, Kim DS, Jung SM, Song JJ, Park YB, et al. (2017) Clinical significance of delta neutrophil index in the differential diagnosis between septic arthritis and acute gout attack within 24 hours after hospitalization. Medicine (Baltimore) 96(30): e7431.
- Long B, Koyfman A, Gottlieb M (2019) Evaluation and Management of Septic Arthritis and its Mimics in the Emergency Department. West J Emerg Med 20(2): 331-341.
- Singh JA, Yu S (2017) The burden of septic arthritis on the U.S. inpatient care: A national study. PLoS One 12(8): e0182577.
- Volzke J, Schultz D, Kordt M, Müller M, Bergmann W, et al. (2020) Inflammatory Joint Disease Is a Risk Factor for Streptococcal Sepsis and Septic Arthritis in Mice. Front Immunol 11: 579475.
- D'Angelo F, Monestier L, Zagra L (2021) Active septic arthritis of the hip in adults: what's new in the treatment? A systematic review. EFORT Open Rev 6(3): 164-172.
- Burke KE, Lamont JT (2014) Clostridium difficile infection: a worldwide disease. Gut Liver 8(1): 1-6.
- Elliott B, Androga GO, Knight DR, Riley TV (2017) Clostridium difficile infection: Evolution, phylogeny and molecular epidemiology. Infect Genet Evol 49: 1-11.
- Eckert C, Barbut F (2010) Infections à Clostridium difficile [Clostridium-difficile-associated infections]. Med Sci (Paris) 26(2): 153-158.
- Czepiel J, Dróżdż M, Pituch H, Kuijper EJ, Perucki W, et al. (2019) Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis 38 (7): 1211-1221.
- Sahu KK, Tsitsilianos N, Moselle L, Mishra AK (2020) Septic arthritis of hip joint and its devastating complications. BMJ Case Rep 13(2): e233909.
- Jiang JJ, Piponov HI, Mass DP, Angeles JG, Shi LL, et al. (2017) Septic Arthritis of the Shoulder: A Comparison of Treatment Methods. J Am Acad Orthop Surg 25(8): e175-e184.

 Case Report
Case Report