Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yáñez N1*, Bravo M2 and Pinedo F3
Received: January 24, 2023; Published: February 08, 2023
*Corresponding author: Yáñez N, Dental surgeon in Centro Odontológico Padre Mariano, Santiago, Chile
DOI: 10.26717/BJSTR.2023.48.007657
The aim of this study is to present a case report of a patient who presents a lower third molar associated with a dentigerous cyst, whose lesion displaced the tooth until it was immersed within the lower alveolar canal. Case: Patient asks for treatment of a dentigerous cyst associated with a displaced third molar towards the inferior alveolar nerve and basilar border. A cyst’s decompression in addition to a traction of the tooth with orthodontics were performed in order to later the tooth could be extracted in a secure way. Conclusion: Traction of the third molar offers a good choice in cases such as the one presented in this article. Although the evolution of the patient is favorable, there is a lack of evidence that demonstrates its efficacy.
Keywords: Third Molar; Dentigerous Cyst; Orthodontic Extraction
Third molar surgery is one of the most common practices in maxillofacial surgery [1]. These teeth have a variable anatomy, position and location, thus determining the way in which each procedure will be performed [1-3]. There are noble anatomical structures in relation to the third molars that must be preserved, including, for example, the inferior alveolar nerve (NAI) [4]. The most common complication of neurosensory alterations is due to the extraction of lower third molars, a product of the proximity that the tooth can present with this structure [2]. The damage can be temporary (4 to 6 months) or permanent [5], manifesting symptoms such as reduced sensation (hypoesthesia), abnormal (paresthesia) or unpleasant (dysesthesia) [6]. On the other hand, there are pathologies associated with the third molar that increase the complexity of the procedure, such as infections, mandibular fracture, damage to the mylohyoid nerve, tumor or cystic lesions [2,7]. Dentigerous cysts are lesions that develop due to the expansion of the dental follicle around an unerupted tooth [8], with the lower third molar being the tooth most involved [9-11]. It is the second most frequent lesion associated with teeth and has a prevalence of between 11-33% within all odontogenic cysts [9,10]. The general indication of this pathology is the enucleation of the cyst and the resection of the tooth, however, there are cases in which the size of the lesion could generate a pathological fracture [10]. The objective of this study is to present a case report of a patient who presents a lower third molar associated with a dentigerous cyst, whose lesion displaced the tooth until it was immersed within the inferior alveolar canal. An unconventional technique that could offer a safer and more conservative alternative to these cases will be described.
A 48-year-old male patient comes to the Santa María Clinic due to a long-standing increase in volume (investigated 3 years ago) in relation to the lower right mandibular area, which has not received treatment since it has not generated symptoms over time. The patient has no morbid history, does not report medication consumption, no smoking or use of other substances. Extraoral clinical examination shows no volume increases or lymphadenopathy. There is no paresthesia of the right NAI. Intraoral examination shows no soft tissue abnormalities. The piece 4.8 is clinically absent, when palpating the area there is no presence of bulging of boards. In the panoramic radiography in which the finding was made (Figure 1), a radiolucent, rounded image of defined boundaries in relation to the crown of tooth 4.8, which is included, is observed. In the cone beam computed tomography, taken upon entering our service, progression of the lesion is observed, with displacement of the tooth to the mandibular basilar border.
Figure 1 Panoramic radiograph when the lesion is investigated. An extensive radiolucent area is observed, with clear margins, associated with an included third molar. Based on the clinical and radiographic characteristics of the lesion, the time of progression and location, the diagnostic hypothesis of tooth-associated dentigerous cyst is elaborated 4.8.
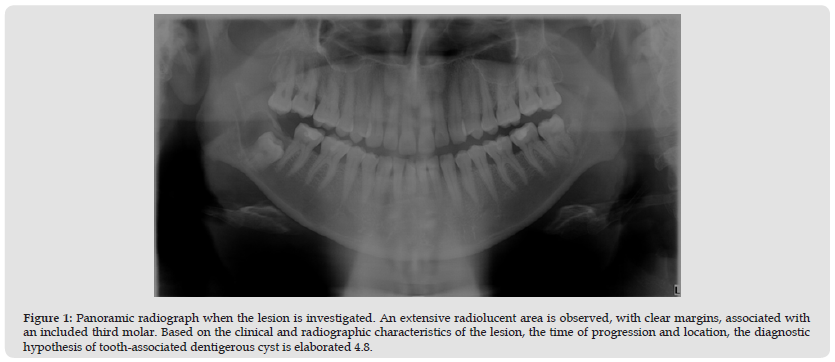
Figure 2 Cone beam computed tomography showing the lesion in all three senses of space. Note piece 4.8 displaced to the basilar rim, in addition to an advance of the lesion reaching the distal root of tooth 4.7.
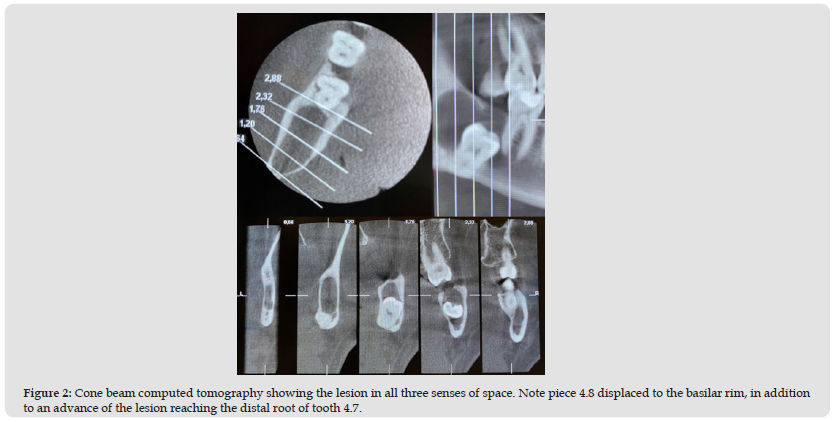
Figure 3 A. Triangular flap with osteotomy to achieve an opening of the cystic lesion. B. Location of the part 4.8.
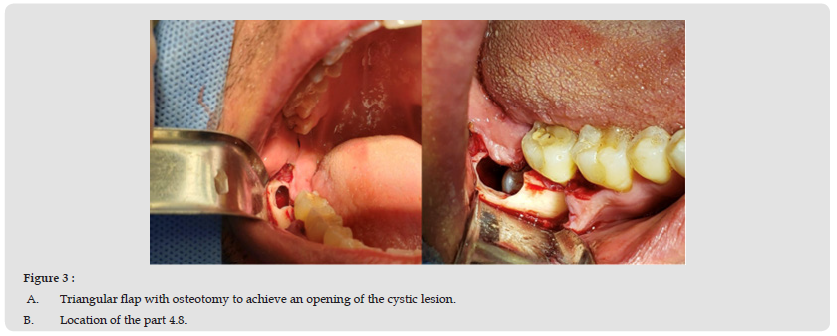
Figure 4 Control 7 days after installation of the cannula and resin button to pull the piece 4.8. The opening fulfills the function of connecting the bracket to the third molar as well as decompressing the cyst.
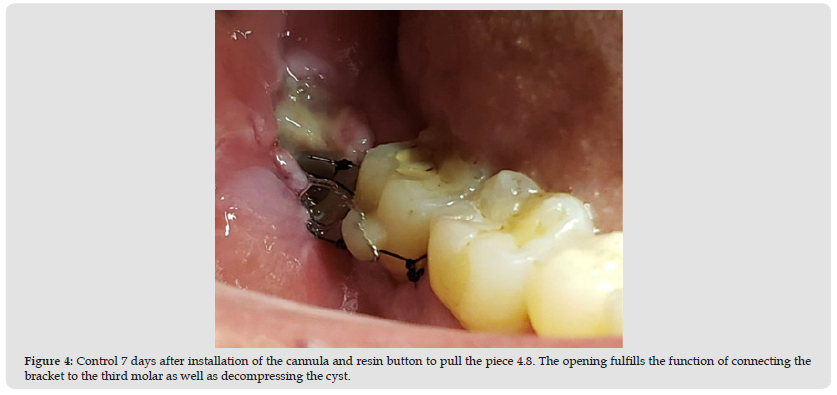
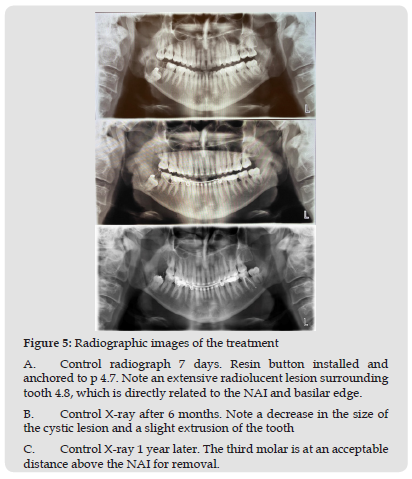
It is also possible to observe that this increase in volume respects the mandibular anatomy, does not perforate tables and there is no evidence of rhizolysis (Figure 2). Treatment alternatives are explained to the patient. The first option would be the enucleation and immediate extraction of the tooth, which although it would be a more immediate treatment, presents a treatment prognosis reserved for the high risk of a neurosensory alteration of the NAI and a mandibular fracture. On the other hand, you can do a decompression of the lesion, pull the third molar by fixed orthodontics in order to move the tooth away from the alveolar canal and later, extract it in a safer way, however, it will require follow-up with periodic controls. Due to the high risk of damage to the NAI and size of the lesion, in addition to a great interest on the part of the patient to solve the case, it is decided together to perform a decompression of the cyst plus an extrusion of the third molar by means of an orthodontic button. The patient does not have any economic, geographical or cultural impediment to perform this treatment. First, a sample of the cystic lesion is taken (Figure 3) and a resin button is cemented to tooth 4.8. In addition, a cannula is installed to decompress the lesion, passing the wire of said button through the cannula for future traction. After having controlled the patient 7 days later, he is referred to the orthodontic specialty for fixation and traction of the third molar (Figure 4). The sample is sent to biopsy for histopathological study, which confirms the diagnosis of dentigerous cyst. The patient was followed weekly for the first month, then monthly until completing 12 months. In each control, the state of the connection, presence or absence of infection and the permanence of the resin button in the third molar were evaluated. In case of wire breakage, it was reinstalled in the periodic checks (Figure 5). After 12 months of follow-up, it is possible to observe a sufficient extrusion to perform disinclusion of the third molar with a low risk of damage to the NAI, a procedure which is carried out without complications (Figure 6).
Figure 5 Radiographic images of the treatment A. Control radiograph 7 days. Resin button installed and anchored to p 4.7. Note an extensive radiolucent lesion surrounding tooth 4.8, which is directly related to the NAI and basilar edge. B. Control X-ray after 6 months. Note a decrease in the size of the cystic lesion and a slight extrusion of the tooth C. Control X-ray 1 year later. The third molar is at an acceptable distance above the NAI for removal.
There are several techniques to protect NAI, such as coronectomy, however, this technique can bring complications such as apical periodontitis, infection, pathological migration of the roots, among others [12,13]. In this case, this technique is excluded, due to the fact that the tooth was associated with an extensive cyst, which would not allow a correct sealing of the apical portion. Another option would be to extract the tooth immediately. This not only presents an obvious risk of injury to the NAI as explained above, but there would be the need to reinforce the mandibular massif with a reconstruction plate plus bone graft, to avoid a pathological fracture. Immediate enucleation of the cyst is not indicated in any case, since it would leave a considerable bone defect. In the literature there are variations of this technique, such as changing the force vector from the maxilla [14] or even through the use of microscrews15. All agree that this alternative is simple, safe and cost-effective, highlighting the patient’s adherence to the treatment plan. An open cavity with a fixed apparatus is a predisposing factor to develop biofilm and, therefore, an increased risk of infection. That is why the patient was instructed to irrigate the access with CHX to maintain proper access hygiene. On the other hand, patient commitment, interdisciplinary management with orthodontics and adherence to treatment are key to the success of this type of technique. Our patient attended practically all the controls, getting involved in the treatment plan. Orthodontic extrusion of the third molar has been shown to be effective in reducing the risk, however, it is not without complications, moreover, although our case has been successful, there is still not enough evidence to show that orthodontic traction significantly reduces damage to the inferior alveolar nerve [14,15].
Orthodontic traction of the third molar offers a good alternative to these cases. The cooperation of the patient, a correct follow-up and analysis of the clinical case are key to success. Although the patient’s evolution towards this treatment is favorable, there is a lack of evidence that significantly demonstrates its effectiveness.
The authors declare that they have no conflict of interest , nor any funding sources.


