Abstract
This article is a continuation of a series of studies on the optimization of techniques and methods of surgical operations for hernias of the esophageal aperture of the diaphragm and is based on the use of the author’s development of a model of a two-layer biocarbon mesh implant. The purpose of this study is to highlight the immediate and long-term results of using a double-layer biocarbon mesh implant in comparison with the standard method of using a polypropylene implant when operating patients with large and giant hiatal hernia.All patients were divided into 2 research groups that underwent alloplastic with various implants: Group I of 221 patients who underwent alloplasty with a polypropylene mesh implant (171 patients with large hernias of 10-20 cm2) and 50 patients with giant hernias of the esophageal orifice with the area of the hernial defect is more than 20 cm2); Group II of 79 patients who underwent an original alloplastic with a bi-layer biocarbon mesh implant (50 patients with large hernias and 29 patients with giant hernia of the esophageal orifice). Postoperative complications were classified according to the Clavien-Dindo scale.The index «De Meester» was used as a comparison criterion. The article discusses the results of operations of 300 patients for large and giant hernias of the esophageal aperture of the diaphragm, of which 79 were operated on using a prototype biocarbon double-layer mesh implant according to the author’s patent. The paper presents immediate and long-term results. The results of surgical treatment are pilot and representative, which determine the further tactics and direction of improving operations to remove large and giant hernias of the esophageal opening of the diaphragm. For the first time, data on the use of the author’s development of a bi-layer biocarbon mesh implant are presented and compared with a polypropylene mesh implant during an «on-line» plastic repair of large and giant hiatal hernia. Significant differences were obtained in relapses of all types in favor of a biocarbon mesh implant (5,6 versus 22,8%; p < 0,0001; Fisher’s exact test).
Keywords: Large herniasof the esophageal aperture of the diaphragm; Giant hernias of the esophageal aperture of the diaphragm; Alloplasty; Onlay; Plastic;Biocarbon double - layer mesh implant; Polypropylene mesh implant; Surgery technique
Introduction
This article is a continuation of a series of studies on the optimization of the technique and methodology of surgical operations for hiatal hernias and is based on the use of the author’s development of a model of a two-layer biocarbon mesh implant [1- 4].The aim of this study is to highlight the immediate and long-term results of using a two-layer biocarbon mesh implant in comparison with the standard technique of using a polypropylene implant when operating on patients with large and giant hiatal hernias. The classical technique of “onlay” plasty with a polypropylene implant involves the use of a standard or lightweight mesh with its fixation over the sutured legs of the diaphragm [1,5-9]. In this case, coarse scar tissue is formed, a significant wrinkling of the mesh occurs, the contact of the implant with the esophagus remains, which leads to the development of anatomical recurrence [5,8]. The developed technique of laparoscopic two-layer plasty using a two-layer biocarbon mesh implant has two key advantages.Firstly, the implant used is not only lightweight, but also partially consists of biocarbon fibers, which are a super-strong material, which reduces the likelihood of recurrence, as well as monoaryl, which dissolves over several months. At the same time, soft scar tissue forms around the implant, and the mesh shrinks to a small extent. Secondly, the mesh implant is closed by the legs of the diaphragm, which prevent its contact with the esophagus. Thus, the implant does not cause a “sawing” effect during breathing movements of the diaphragm. These benefits dramatically reduce the risk of esophageal complications.
Material and Research Methods
In total, 300 patients were operated on for large and giant hiatal hernias from 2014 to 2018. Of 300 patients, 221 were installed with a polypropylene mesh, and 79 patients were operated on using a prototype of a two-layer biocarbon mesh implant according to the author’s patent (registration No. 20181 dated July 16, 2018). All patients were divided into 2 study groups, which underwent alloplasty with various implants:
I. Group I of 221 patients who underwent alloplasty with a
polypropylene mesh implant (171 patients with large hernias
with an area of 10-20 cm2 and 50 patients with giant hiatal
hernias with an area of more than 20 cm2 hernias).
II. Group II of 79 patients who underwent original alloplasty
with a two-layer biocarbon mesh implant (50 patients with
large hernias and 29 patients with giant hiatal hernias).
Postoperative complications were classified according to the
Clavien-Dindo scale, according to which:
I. I degree - any deviations from the normal postoperative
course that do not require drug treatment (except for
antipyretics, analgesics, antiemetics) or surgery.
II. II degree - complications that do not threaten life, which
require drug treatment, including blood transfusion and
parenteral nutrition.
III. III degree - complications that are not life threatening and
require surgical, endoscopic, or radiological intervention:
a. III a degree - without general anesthesia, III b degree -
under general anesthesia.
b. IV degree - life-threatening complications, including
cerebrovascular complications, which require treatment in an
intensive care unit:
c. IV a degree - dysfunction of one organ, including dialysis,
IV b degree - multiple organ failure.
d. V degree - death.
The “De Meester” index was used as a comparison criterion, in the norm it is equal to 14.7.
Research Results and Discussion
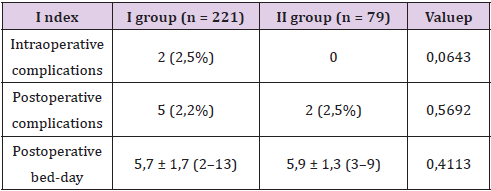
Immediate Results
There were no intraoperative complications in group I.In group II, there were 2 cases (2.5%) of pneumothorax, which required drainage of the pleural cavity.There were no significant differences in the incidence of intraoperative complications between the groups (0.0 versus 2.5%, respectively, p = 0.0643, Fisher’s exact test).Postoperative complications in group I occurred in 5 patients (2.2%): 3 cases of atelectasis with fever and 1 case of trocar wound infection. These cases were classified as grade II according to the Clavien - Dindo classification. There was also 1 case of subphrenic hematoma, which required puncture drainage, which belonged to grade III a according to the Clavien-Dindo classification.Postoperative complications in group II occurred in 2 patients (2.5%): atelectasis with fever, which belonged to the II degree according to the Clavien - aDindo classification.There were no significant differences in the incidence of postoperative complications between the groups (2.2% versus 2.5%, p = 0.5692, Fisher’s exact test). The average postoperative bed-day was 5.7 ± 1.7 (2-13) days in group I and 5.9 ± 1.3 (from 3 to 9) days in group II. There were no significant differences between the groups in postoperative bed-days (5.7 ± 1.7 versus 5.9 ± 1.3, p = 0.4113, Mann-Whitney test) (Table 1).
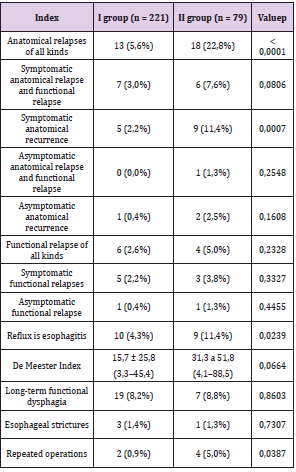
In group I of 221 patients, anatomical relapses of all types were found in 13 patients (5.6%). They were distributed as follows: symptomatic anatomical relapse and functional relapse were detected in 7 patients (3%), symptomatic anatomical relapse - in 5 patients (2.2%), asymptomatic anatomical relapse and functional relapse were absent, asymptomatic anatomical relapse was detected in 1 patient (0.4%). Functional relapses of all types were detected in 6 patients (2.6%). Of these, symptomatic functional relapses were detected in 5 patients (2.2%), asymptomatic functional relapse - in 1 patient (0.4%).Reflux esophagitis was detected in 10 patients (4.3%). The average De Meester index measured in 162 patients was 15.7 ± 25.8 (3.3-45.4). Long-term functional dysphagia occurred in 19 patients (8.2%). Strictures occurred in 3 cases (1.3%). Reoperations were performed in 2 patients (0.9%): both for symptomatic anatomical recurrence and functional recurrence.
In group II, of 79 patients, anatomical relapses of all types were
detected in 18 patients (22.8%). They were distributed as follows:
symptomatic anatomical relapse and functional relapse were
detected in 6 patients (7.6%), symptomatic anatomical relapse - in 9
patients (11.4%), asymptomatic anatomical relapse and functional
relapse - in 1 patient (1, 3%), asymptomatic anatomical recurrence
- in 2 patients (2.5%). Functional relapses of all types were found
in 4 patients (5%). Of these, symptomatic functional relapses were
detected in 3 patients (3.8%), asymptomatic functional relapse - in
1 patient (1.3%).
Reflux esophagitis was detected in 9 patients (11.4%). The
mean De Meester index measured in 60 patients was 31.3 ± 51.8
(4.1-88.5). Long-term functional dysphagia occurred in 7 patients
(8.8%). Stricture occurred in 1 case (1.3%). Reoperations were
performed in 4 patients (5%): in 2 patients for symptomatic
anatomical relapse and functional relapse, in 1 patient for stricture
and in 1 patient for symptomatic anatomical relapse.In terms
of the frequency of anatomical relapses of all types, a significant
difference was found in favor of group I (5.6% versus 22.8%, p
<0.0001, criterion x2). There was no significant difference in the
frequency of symptomatic anatomical recurrence and functional
recurrence (3% versus 7%, p = 0.0806, criterion x2). In terms of
the frequency of symptomatic anatomical recurrence, a significant
difference was found in favor of group I (2.2% versus 11.4%, p =
0.0007, criterion x2). There was no significant difference in the
frequency of asymptomatic anatomical relapses and functional
relapses (0.0 versus 1.3%, p = 0.2548, Fisher’s exact test). There
was also no significant difference in the frequency of asymptomatic
anatomical relapses (0.4% versus 2.5%, p = 0.1608, Fisher’s exact
test). There was no significant difference in the frequency of
functional relapses of all types (2.6 versus 5.0%, p = 0.2328, Fisher’s
exact test). There was no significant difference in the frequency of
symptomatic functional relapses (2.2% versus 3.8%, p = 0.3327,
Fisher’s exact test). There was also no significant difference in the
frequency of asymptomatic functional relapses (0.4 versus 1.3%, p
= 0.4455, Fisher’s exact test). According to the frequency of reflux -
esophagitis, a significant difference was revealed in favor of group I
(4.3% versus 11.4%, p = 0.0239, criterion x2).
There was no significant difference in the average De Meester
index (15.7 ± 25.8 versus 31.3 ± 51.8, p = 0.0664, Mann-Whitney
test). There was no significant difference in the frequency of longterm
functional dysphagia (8.2 versus 8.8%, p = 0.8603, Fisher’s
exact test). There was also no significant difference in the frequency
of esophageal strictures (1.3 versus 1.3%, p = 0.7307, Fisher’s
exact test). In terms of the frequency of reoperations, a significant
difference was found in favor of group I (0.9 versus 5.0%, p =
0.0387, Fisher’s exact test) (Table 2). Based on the analysis of
relapse rates using a polypropylene and biocarbon implant, a twolayer
plastic technique was proposed, which was recommended
to be performed according to the developed method. - the splenic
ligament and mobilization of the esophagus with the elimination
of its shortening by paraoesophageal mediastinal dissection. Then
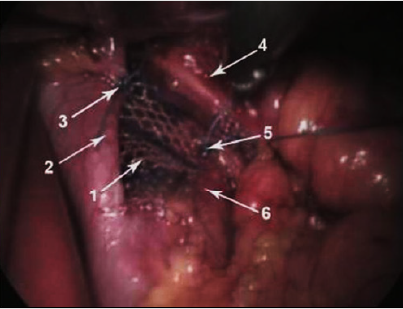
you should perform the actual plastic. First, the edges of a two-layer
biocarbon mesh implant in the form of an isosceles triangle with a
side length of 4 cm and a base length of 3 cm should be fixed to each
of the diaphragm legs behind the esophagus with 2-3 interrupted
non-absorbable sutures (Figure 1). In this case, the upper edge of the
implant in the form of the base of the triangle should not reach the
esophagus, which is completely raised upward by 1 cm to exclude
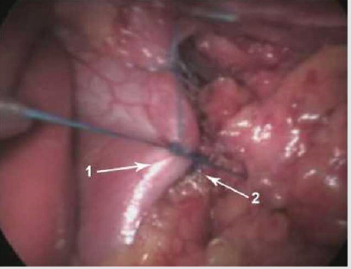
contact. Thus, the “first layer” will be created. Then 2-3 interrupted
sutures of the diaphragm legs are sutured together, which leads to
complete closure of the implant (Figure 2). In this case, the upper
suture should not reach the esophagus, which is completely raised
upwards by 0.5-1 cm. Thus, a “second layer” will be created. Plastic
should be performed with a 30 Fr calibration tube inserted into
the stomach. The next step is a Nissen fundoplication with a cuff
length of 3 cm, as well as non-absorbable suture material using a
calibration probe.
Figure 1: Fixation of the implant to the stems of the diaphragm.
A. Mesh implant,
B. Right leg of the diaphragm,
C. Suture fixing the implant to the right leg of the
diaphragm,
D. Oesophagus,
E. Suture fixing the implant to the left leg of the
diaphragm,
F. Left leg of the diaphragm.
Figure 2: Suturing the legs with closure of the implant.
A. Right leg of the diaphragm,
B. Left leg of the diaphragm.
Conclusion
In terms of the frequency of anatomical relapses symptomatic anatomical relapses, alloplasty gave significantly worse results in the II study group.Similar results were obtained for the frequency of reflux esophagitis and reoperations. There were no significant differences between the compared groups in terms of the frequency of anatomical recurrences.The results of alloplasty in group II with the use of a biocarbon implant can be considered close to satisfactory, but they require improvement due to the use of a special technique for performing operations.The results of using this technique of operations will be statistically compared in the author’s further publications.
References
- Grubnik VV, Malinovskij AV (2015) Kriticheskie aspekty laparoskopicheskoj hirurgii gastroezofageal'noj reflyuksnoj bolezni i grizh pishchevodnogo otverstiya diafragmy. Odessa VMV-tipografiya: 106.
- Rozenfeld II, Akopyan VA (2018) Klassifikaciyanegativny`hrezul`tatovlaparoskopicheskihoperacij pri gry`zhahpishhevodnogootverstiyadiafragmy. Proceedings of the XII International Scientific and Practical Conference of Students and Young Medical Scientists «Youth for Practical Health Care». — Tver: FSBEI of Tver State Medical University of the Ministry of Health of Russia. Council of YoungScientists and Students 856-858.
- Rozenfeld II, Chilikina DL (2018) Ocenkarezul`tatov ispol`zovaniya setchaty`himplantatov pri alloplastikegry`zhpishhevodnogootverstiyadiafragmy. Issledovanie i praktika v medicina 5(4): 156-158.
- Rozenfeld II, Chilikina DL (2018) Problema bol`shix i gigantskix gry`zh pishhevodnogo otverstiya diafragmy` i rezul`taty` osnovny`x metodov ix plastiki [The problem of large and giant hiatal hernia and the results of the main methods of plastics]". Annaly` xirurgii 3: 74-79.
- Antoniou SA, Koch OO, Antoniou G A (2012) Mesh - reinforcedhiatalherniarepair: a review on the effect on postoperative dysphagia and recurrence. Langenbeck'sarchives of surgery 397(1): 19-27.
- Frantzides CT, Carlson MA, Loizides S (2010) Hiatal hernia repair with mesh: a survey of SAGES members. Surgical endoscopy 24(5): 1017-1024.
- Furnée E, Hazebroek E (2013) Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surgical endoscopy 27(11): 3998-4008.
- Granderath FA, Schweiger UM, Kamolz T, M Pasiut, CF Haas, et al. (2002) Laparoscopic antireflux surgerywithroutine mesh – hiatoplasty in the treatment of gastroesophageal reflux disease. Journal of gastrointestinal surgery 6(3): 347-353.
- Targarona EM, Grisales S, Uyanik O, Carmen B, Junal Carlos P, et al. (2013) Long-term outcome and quality of life after laparoscopic treatment of large paraesophageal hernia. World journal of surgery 37(8): 1878-1882.

 Research Article
Research Article