Opinion
Currently, there is no effective vaccine and treatment for COVID-19. Global public health community: governments, research institutions, private sector, WHO and other international organizations are working hard to urgently coordinate the development of medical countermeasures. The socio-economic development, level of development of health system, availability of testing facilities, stage of epidemics and population affected directly affect the crud mortality rate and widely varies among the countries. [1]. The crude clinical case fatality rate is currently over 3%, increasing with age and rising to approximately 15% or higher in patients over 80 years of age. Underlying health conditions that affect the cardiovascular, respiratory, and immune systems confer an increased risk of severe illness and death [2]. It took just months for a localized outbreak of COVID-19 in Wuhan, China to evolve into a global pandemic [1]. Afghanistan, bordering the Islamic Republic of Iran - an early hotspot for COVID-19 - is at a heightened risk of large-scale community transmission in the initial stage of the pandemic. Since January 2020, approximately 300,000 Afghans have returned from Iran. Protracted conflict, high poverty rates, a challenged health system and public services contribute significantly to the COVID-19 epidemic in country [3]. The first case of COVID-19 in Afghanistan was reported on February 24. As of 15 Sep, there are 38,802 confirmed COVID-19 cases in Afghanistan across all 34 provinces, and 1,425 people have died [4]. Initially there was no testing capacity in country. Laboratory testing sites have now been established in 14 locations with a capacity of doing around 5,000 tests per day. Until now (15 Sep) around 110,000 tests have been conducted with an average of 3,000 test per million people [4]. The actual number of COVID-19 positive cases is likely to be substantially higher, reflecting the limited testing capacity in country. The recent seroprevalence survey indicated that more than 30% of the total population is infected. Men between the ages of 40 and 69 represent more than half of all COVID-19-related deaths (COVID PS 2020). The CDC Flu surge software fluSurge2.0 was used to assess various scenarios and predicate the potential burden of diseases for Afghanistan for guiding the control measures. The model was initially designed by the United States Centers of disease Control and Prevention to estimate the impact of influenza pandemic on hospital surge capacity [5].
The following scenarios were considered for Afghanistan:
a) The best-case scenario: estimates the fewest possible
number of hospitalizations
b) The most likely scenario estimates the number of
hospitalizations most likely to occur
c) The worst-case scenario
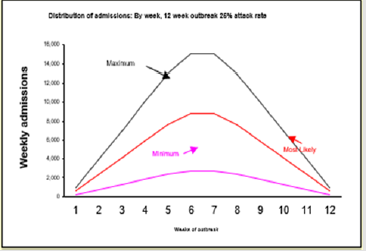
Palwasha Anwari in her paper indicated that “its most likely to have 83,000 hospital admission, and 13,000 deaths over the course of 12 weeks” [6]. Considering the existing capacity of health system, ongoing fragility, limited domestic resource allocation for health sector, growing burden of diseases, low level of literacy and global shortage of essential supplies, the ministry of public health and partners may adopt one the following options for controlling COVID-19 pandemic in Afghanistan (Figure 1).
Firstly, strengthening and expanding control measures including coordination and planning, surveillance, rapid response, case investigation and management, lab capacity, screening at the points of entry (PoE), infection prevention and control (IPC), risk communication and community engagement and continuation of essential health services. In addition, early planning, and arrangement for the introduction of effective vaccine and treatment when becoming available. Moreover, reinforce the continuation of all non-pharmaceutical interventions: practicing frequent hand washing, following respiratory etiquettes, social distancing, closing all public and private schools and universities and ban on all public gatherings. On the contrary, strictly enforcing lockdown seems extremely challenging as around 55% of the population live under the poverty line and 66% of the population are engaged in informal employment and survive on daily wages [7]. In the absence of social protection, the continuation of lockdown significantly increases poverty, malnutrition, and hunger that may cause more mortality in the long term than COVID-19.
Secondly, its strongly recommended to strengthen and expand all interventions under OPTION I and gradually end lockdown. A survey conducted in Kabul indicated a higher level of COVID-19 antibodies in the blood (52% with RDT while 31% with PCR) [8], this could be a positive sign indicating rapid development of herd immunity as compared to the countries enforced complete lockdown and reduce the risk of a potential second wave of disease with additional morbidity and mortality [9]. A relaxation in lockdown will help 66% Afghan population engaged in informal employment to resume their work and lessen the risk of increasing poverty. At the same time with relaxation in lockdown in the short term, we may have increased COVID-19 related morbidity and mortality but it seems less likely as the current lockdown was not effective and to a large extend extensively violated. In addition, the survey findings indicate that a large proportion of the population already have asymptomatic infection. Moreover, as Afghanistan has a younger population (more than 67% is under the age of 25) will expected to experience mild diseases with minimum mortality. Exposure, particularly of the young population, to more infection may induce herd immunity. However, the WHO has condemned the “dangerous” concept of herd immunity for managing the COVID-19 pandemic [10].
Lastly, strengthening and expanding all interventions under OPTION I and immediately end the lockdown. All the points discuss under second option are applicable here as well. In addition, we may need to consider the differences in the context of various provinces and deeply analyze the available data from Afghanistan, region, and the rest of the world on immediate termination of lockdown. Return to normal economic life might help and most likely will avert excessive morbidity and mortality due to poverty, malnutrition, and associated diseases in in long term and reduce cumulative morbidity and mortality due to COVID-19 and other communicable diseases. Considering the rapid spread of diseases across the country, widespread cross border movement with Iran (the regional hotspot of COVID-19) and Pakistan, fragile health system, low level of literacy, minimum investment in public health, poor infrastructure, shortage of qualified health workforce, extreme poverty, and overall inadequate response capacity, the modest approach is strongly recommended. It is believed that with gradual termination of lockdown and strengthening health system the level of morbidity and mortality will be kept to minimum in Afghanistan.
References
- (2020) World Health Organization.
- (2020) World Health Organization. COVID 19 STRATEGY UPDATE, Geneva: World Health Organization.
- (2020) OCHA. Humanitarian Response Plan, Afghanistan, Kabul: OCHA.
- (2020) MoPH. COVID-19 Dashboard.
- (2020) Center for Diseases Control and Prevention.
- Palwasha Anwari NS (2020) COVID-19 morbidity and mortality, estimation for Afghanistan, Kabul.
- (2017) National Statistics and Information Authority. Afghanistan Living Condition Survey, Kabul: NSIA.
- (2020) BBC Persian.
- Borja Andrino, D GK LEGS (2020) Antibody study shows just 5% of Spaniards have contracted the coronavirus, Madrid: ELPAIS.
- Prasad R (2020) Aiming to achieve herd immunity naturally is ‘dangerous’, WHO warns, Delhi: The Hindu.

 Opinion
Opinion