Abstract
Introduction: Pancreatic cancer is being known for his aggressiveness and surgical resection is the only potentially curative treatment. Effective analgesia in pancreatic surgery is required for early recovery and healing.
Methodology: We have undertaken a retrospective study on 81 patients who underwent pancreatic resections for pancreatic cancer over 5 years with intravenous and epidural perioperative analgesia.
Results: Sixty-two patients with pancreatoduodenectomy and 19 patients with distal pancreatectomy for malignant tumors, aged 31 to 79 years were included. The epidural analgesia was applied mostly for pancreatoduodenectomy (33 patients) and only in 1 patient with distal pancreatectomy. The median operative time was similar for patients with intravenous analgesia and those with epidural. There was no statistically significant difference in the incidence of postoperative complications between the two groups, but epidural analgesia was associated with a longer stay in intensive care unit (median 5 days vs 4 days, p=0.141).
Conclusions: Both intravenous and epidural analgesia provide a successful pain control in the immediate postoperative period, with no significant difference concerning the rate of postoperative complications.
Keywords: Pancreatic Cancer; Epidural; Analgesia
Introduction
Pancreatic cancer is the seventh leading cause of cancer mortality in industrialized countries, being known for its aggressiveness and poor prognosis [1]. Surgical resection is the only potentially curative therapy for pancreatic cancer. Epidemiological data indicate that only 20% of patients with early-stage disease are suitable for radical surgical resection [2]. Pancreatoduodenectomy (PD) is considered to be the only curative treatment for malignant lesions of the pancreatic head region [3]. Since first described by Whipple et al., despite multiple technical improvements and variants, the morbidity of PD remains as high as 40% [4,5]. Distal pancreatectomy is indicated for tumours of the body and tail of the pancreas and usually requires spleen removal along with the tail of the pancreas, because of the close proximity between the two organs and the necessity of proper lymphadenectomy [6,7]. Postoperative pain is the most feared symptom for most patients and its management might be difficult [8]. Effective analgesia after pancreatic surgery is required for early mobilisation, optimal respiratory function, and prevention of thromboembolic complications [9]. Epidural analgesia is often use for intraoperative and postoperative pain management in pancreatic surgery. This procedure is associated with effective postoperative analgesia, decreasing in pulmonary or cardiac complications, earlier restart of gut motility and a cutback in thromboembolic complications [9,10]. The continuous local analgesia by wound infiltration was reported as a pain management procedure as effective as epidural analgesia [10]. As an alternative, opioids-based analgesia is the most frequently used [9,11].
Materials and Method
Eighty-one pancreatic resections for pancreatic cancer, performed at the Surgical Clinic 2, “St.Spiridon” Emergency Hospital from Iasi, Romania, from January 2014 to December 2018 were included in this study. A database was created with all patient characteristics, including demographic data, clinical data, laboratory data, imaging data (diagnosis and follow-up), surgical protocols, histopathological reports, and postoperative data, including analgesia. Patients with perioperative and postoperative thoracic epidural analgesia were identified and two groups were created: A = patients with intravenous analgesia alone; B = patients with epidural analgesia. The two groups were matched in terms of demographic data.
Results
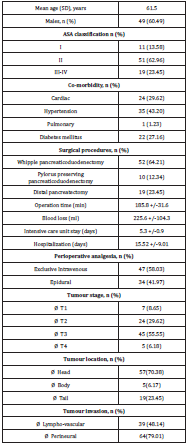
Eighty-one patients with radical pancreatic resections for
malignant tumours were included in this study, aged 31 to 79 years
(mean age: 61.5 years). PD was performed in 62 patients and distal
pancreatectomy in 19 patients, under general anaesthesia. During
PD, the pancreato-jejunal anastomosis was reconstructed as an endto-
side duct-to-mucosa protected with a catheter anastomosis or
a two-layer pancreato-jejunal anastomosis. Patient characteristics
and tumor features were presented in Table 1. Before surgery, 34
patients were initially submitted to thoracic epidural analgesia
placed within a T7–T9 interspace level according to standard
procedures. A continuous epidural infusion was initiated 20 min
before surgical incision and consisted of bupivacaine 0.1% 1 mg/
ml, continued during the surgical procedure, and up to 4 days
postoperatively.
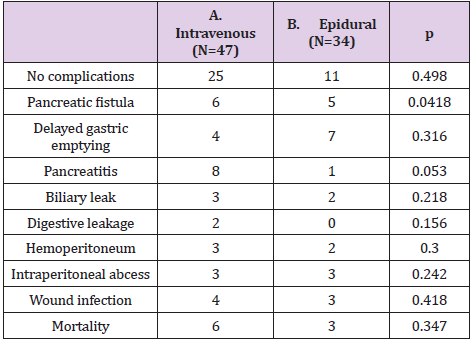
The epidural analgesia was applied mostly for PD (33 patients)
and only in 1 patient with distal pancreatectomy. The median
operative time was similar for patients with intravenous analgesia
and those with epidural. There was no statistically significant
difference in the incidence of postoperative complications between
the two groups, but epidural analgesia was associated with a longer
stay in intensive care unit (median 5 days vs 4 days, p=0.141)
(Table 2).
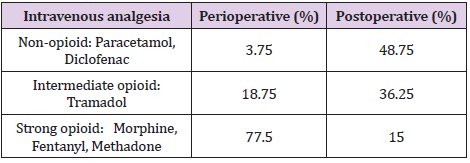
In our group study, non-steroidal anti-inflammatory drugs
are the first-line agents most used for the control of mild pain in
postoperative recovery time (Table 3). The switch to another class
of pain control drugs was made after the assessment of the dosage
at regular time intervals. Strong opioids were used only in intensive care unit for patients with moderate and severe pain with no
response at non-opioids.
Discussion
Pancreatic resections are major surgical abdominal procedures,
associated with high morbidity rate. There is a correlation
between inflammation and cancer development and recurrence,
as well as between the postoperative inflammatory response and
the development of persistent pain syndromes [12]. Epidural
analgesia can mitigate the inflammatory response by creating a
sympathetic blockade [13]. Besides its role as an effective tool for
anesthesiologists in acute pain management, there are studies
suggesting that epidural analgesia decreases the postoperative
morbidity in pancreatic surgery, reducing the incidence of
cardiovascular, respiratory and thromboembolic complications or
ileus [14,15]. In the early postoperative period, the use of epidural
analgesia can also improve patient recovery. By producing a
sympathectomy, it allows the dominance of the parasympathetic
system, thus accelerating the return of gut motility [16]. This
benefit of epidural analgesia is particularly valuable for one of the
most common complication after PD, delayed gastric emptying [17].
The use of the thoracic epidural analgesia increased in the last
10 years in our department but is still not included in the routine
protocol for major surgery. Our study found no significant difference
concerning the complications rate for the patients with epidural
analgesia and intravenous analgesia. Similar results regarding
gastrointestinal complications after pancreatic resections were
found by a randomized clinical trial recently published [18]. In our group with epidural analgesia, a better pain control was achieved
in the immediate postoperative time. Intensive unit care stay was
longer, but with no impact on the hospitalization period. The
period of postoperative pain control obtained by epidural analgesia
compared to intravenous analgesia was highly discussed and a
randomized trial revealed a better pain management with epidural
analgesia in the first 48 hours after hepato-pancreato-biliary
surgery [18,19]. Concern is raised by the hemodynamic instability
associated with pancreatic surgery. It can occur independently of
the type of analgesia, but also as a side effect of epidural analgesia,
prompting the closure of the epidural infusion [20].
Also, the necessity of fluid resuscitation increases the risk
of pulmonary or bowel wall oedema and may contribute to a
higher incidence of pancreato-jejunal anastomotic leakage and
subsequent pancreatic fistula [21]. Several prospective, single
blind, randomized control trials are still investigating the benefits
of epidural analgesia in pancreatic resections, including patient
recovery and healing, serum inflammatory markers, and tumour
recurrence and overall survival [22]. Limitations of this research
are its retrospective design, the fact that is a single centre study,
with small sample size and an uneven number of procedures
between the two groups.
Conclusion
Even if an improvement of the long-term outcome after pancreatic surgery was not correlated with the type of peri- and postoperative analgesia, both intravenous and epidural analgesia provide a successful pain control in the immediate postoperative period. The choice between intravenous and epidural analgesia is based on complex clinical and biological pre-operative assessment, both procedures being effective and safe for postoperative pain management.
References
- (2018) SEER Cancer Statistics Review. National Cancer Institute.
- Siegel RL, Miller KD, Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1): 7-30.
- Kuhlmann KF, de Castro SM, Wesseling JG, F J W ten Kate, G J A Offerhaus, et al. (2004) Surgical treatment of pancreatic adenocarcinoma; actual survival and prognostic factors in 343 patients. J Cancer 40(4): 549-558.
- Riediger H, Makowiec F, Fischer E, Adam U, Ulrich T Hopt, et al. (2006) Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg 10(8): 1106-1115.
- Dolay K, Malya FU, Akbulut S (2019) Management of pancreatic head adenocarcinoma: From where to where? World J Gastrointest Surg 11(3): 143-154.
- Jing W, Zhu G, Hu X (2013) Distal pancreatectomy with en bloc celiac axis resection for the treatment of locally advanced pancreatic body and tail cancer. Hepatogastroenterology 60: 187-190.
- Chandrasegaram MD, Goldstein D, Simes J, V Gebski, J G Kench, et al. (2015) Meta-analysis of radical resection rates and margin assessment in pancreatic cancer. Br J Surg 102(12): 1459-1472.
- Puleo F, Marechal R, Demetter P, Bali MA, Calomme A, et al. (2015) New challenges in perioperative management of pancreatic cancer. World J Gastroenterol 21(8): 2281-2293.
- Pratt WB, Steinbrook RA, Maithel SK, Vanounou T, Callery MP, et al. (2008) Epidural analgesia for pancreatoduodenectomy: a critical appraisal. J Gastrointest Surg 12(7): 1207-1220.
- Mungroop T, Veelo D, Besselink M, van Dieren S, M van Gulik T, et al. (2016) Continuous wound infiltration versus epidural analgesia after hepato-pancreatobiliary surgery (POP-UP): a randomised controlled, open-label, non-inferiority trial. Lancet Gastroenterol Hepatol 1(2): 105-113.
- Kasivisvanathan R, Abbassi-Ghadi N, Mallett S, Prout J, Clevenger B, et al. (2014) A prospective cohort study of intrathecal versus epidural analgesia for patients undergoing hepatic resection. HPB (Oxford) 16(8): 768-775.
- Katz J, Seltzer Z (2009) Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother 9(5): 723-744.
- Zhang JM, An J (2007) Cytokines, inflammation, and pain. Int Anesthesiol Clin 45(2): 27-37.
- Sanford DE, Hawkins WG, Fields RC (2015) Improved peri-operative outcomes with epidural analgesia in patients undergoing a pancreatectomy: a nationwide analysis. HPB (Oxford) 17(6): 551-558.
- Amini N, Kim Y, Hyder O, Spolverato G, Wu CL, et al. (2015) A nationwide analysis of the use and outcomes of perioperative epidural analgesia in patients undergoing hepatic and pancreatic surgery. Am J Surg 210(3): 483-491.
- Leslie JB, Viscusi ER, Pergolizzi JV, Panchal SJ (2011) Anesthetic routines: the anesthesiologist’s role in GI recovery and postoperative ileus. Adv Prev Med 2011: 976904.
- Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, et al. (2012) Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg 256: 529-537.
- Klotz R, Larmann J, Klose C, Bruckner T, Benner L, et al. (2020) Gastrointestinal complications after pancreatoduodenectomy with epidural vs patient-controlled intravenous analgesia: a randomized clinical trial. JAMA Surg 155(7): e200794.
- Aloia TA, Kim BJ, Segraves-Chun YS, Juan P Cata, Mark J Truty, et al. (2017) A randomized controlled trial of postoperative thoracic epidural analgesia versus intravenous patient-controlled analgesia after major hepatopancreatobiliary surgery. Ann Surg 266(3): 545-554.
- Shah DR, Brown E, Russo JE, Chin-Shang Li, Steve R Martinez, et al. (2013) Negligible effect of perioperative epidural analgesia among patients undergoing elective gastric and pancreatic resections. J Gastrointest Surg 17(4): 660-667.
- Axelrod TM, Mendez BM, Abood GJ, James M Sinacore, Gerard V Aranha, et al. (2015) Peri-operative epidural may not be the preferred form of analgesia in select patients undergoing pancreaticoduodenectomy. J Surg Oncol 111(3): 306-310.
- Pak LM, Haroutounian S, Hawkins WG, Worley L, Kurtz M, et al. (2018) Epidurals in Pancreatic Resection Outcomes (E-PRO) study: protocol for a randomised controlled trial. BMJ Open 8(1): e018787.

 Mini Review
Mini Review