Abstract
Isolated osteochondral fractures of the articular surface of the metatarsal head are rare injuries. To the best of our knowledge, there are less than ten reported cases of an acute isolated osteochondral metatarsal head fracture in the literature and no consensus has been reached regarding the best treatment. Both conservative treatment, through manipulation and close reduction, as well as open reduction and internal fixation were performed with good outcomes. We present a rare case of an isolated slipped-retroverted osteochondral fracture of the second metatarsal head treated by open reduction and internal fixation with a Herbert screw with an excellent outcome. The postoperative period was uneventful, and an excellent outcome was achieved. This case highlights the importance of a careful clinical and radiological evaluation for these rare lesions in order to avoid the undesirable sequelae of a missing diagnosis.
Keywords: Metatarsal Head; Isolated Osteochondral Fracture; Metatarsophalangeal Joint
Introduction
Metatarsal head fractures are uncommon lesions and reports of isolated osteochondral fractures of the metatarsal head are extremely rare, with few cases described in the literature [1-9]. Usually reported as secondary to fatigue [10], stress fractures [11,12], or Frieberg’s disease [13,14], there are few reports of a traumatic cause. Patients normally report sharp pain associated with painful weight bearing, tenderness and swelling over the metatarsal head [1-9]. Treatment is still controversial with both open and close methods being used with success [1-9]. Despite the treatment option, the major prognostic factor is the anatomical reduction of the articular surface and the progression to avascular necrosis, leading to a better outcome and faster return to normal function [4,5,8]. Here we present a rare case of an isolated slippedretroverted osteochondral fracture of the second metatarsal head.
Case Report
A 19-year-old male presented at our emergency department with a history of left foot trauma when landing from a jump, with the toes in hyperextension. He reported immediate onset of acute pain and inability to perform weight bearing as well as dorsal swelling over the second metatarsophalangeal joint. He denied any significant past medical history or any current medications. Physical examination revealed swelling, bruising and pain over the left second metatarsal head. He presented painful mobilization of the second metatarsophalangeal joint as well as crepitation on palpation and had no neurovascular impairment. Plain radiographs, with oblique and anteroposterior views, of the left foot revealed an osteochondral fracture of the second metatarsal head (Figure 1). Due to the nature of the lesion and fracture pattern, a CT scan was preformed, showing a slipped retroverted osteochondral fragment (Figure 2).
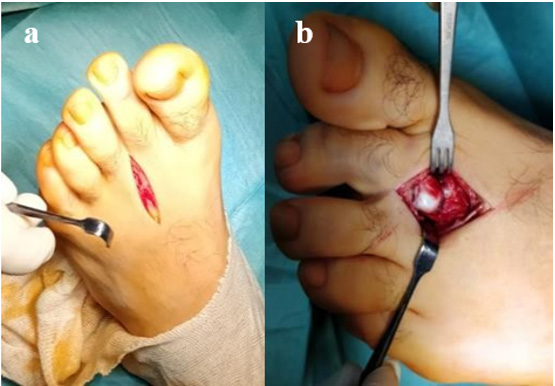
Due to the intraarticular pattern of the fracture and the risk of additional trauma to the osteochondral fragment no attempt of close reduction was performed. A surgical intervention was proposed in order to obtain an anatomic reduction and rigid internal fixation. A longitudinal dorsal approach over the second metatarsophalangeal joint was performed and the extensor tendon was retracted (Figure 3a). After careful dissection and longitudinal capsulotomy, the fracture was exposed and the retroverted osteochondral fragment was visualized (Figure 3b). The metatarsal head showed none of the typical pathological features that could suggest underlying bone pathology such as Freiberg’s disease. Anatomical reduction of the fracture was achieved followed by internal fixation with a single Herbert screw (Figure 4). The stability of the joint was tested, and the integrity of the collateral ligaments was confirmed. The quality of reduction and screw position were assessed by X-ray image intensifier and, after careful hemostasis, the capsule and the skin were closed (Figure 5).
Figure 1: (a) Anteroposterior and
(b) Oblique plain radiographs of the left foot showing
the osteochondral fracture of the second metatarsal head.
Figure 2: CT scan images in the axial, coronal and sagittal planes showing the intraarticular slipped retroverted osteochondral fragment.
Figure 3: (a) Intraoperative view showing the longitudinal dorsal
approach and
(b) The retroverted osteochondral fragment.
Figure 4: Intraoperative view showing anatomical reduction of the fracture and temporary fixation with K-wires, followed by internal fixation.
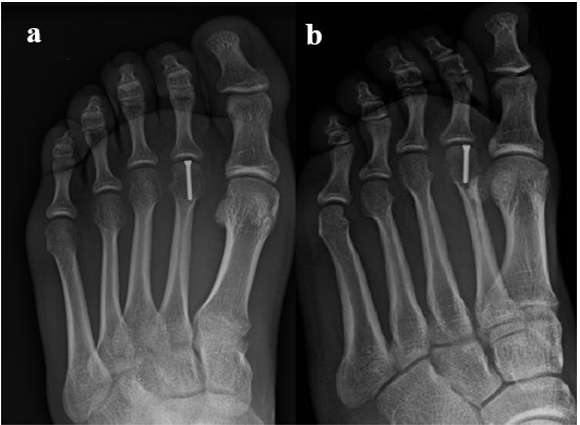
The postoperative period was uneventful, and the patient was discharged the day after surgery. Partial weight bearing was allowed with a Barouk type shoe for the first 4 weeks and gradually progressing to full weight bearing. Active and passive mobilization of the joint was encouraged immediately. The patient presented a good clinical and imagiological evolution, with serial follow-up radiographs showing good screw position with complete bone healing after 8 weeks (Figures 6 & 7). At final follow-up examination, 12 months after surgery, the patient presented no pain and full range of active and passive motion of the second metatarsophalangeal joint. Radiographs showed complete union of the fracture with no evidence of avascular necrosis or arthritic changes of the second metatarsal head (Figure 8). He had resumed sports and daily life activities with no limitations.
Figure 6: (a) Anteroposterior and
(b) Oblique postoperative radiographs at 4 weeks
showing good bone healing evolution.
Figure 8: (a) Anteroposterior and
(b) Oblique postoperative radiographs at 12 months
follow-up showing complete union of the fracture with no
evidence of avascular necrosis or arthritic changes of the
second metatarsal head.
Discussion
Reports of an isolated osteochondral fracture of the metatarsal head are rare, with 12 cases described in literature [1-9]. Only seven were acute fractures [2-8] while the other five corresponded to delayed presentations [1,7,9]. As uncommon injuries, isolated osteochondral fractures of the metatarsal head can easily be missed. Heckman [1] first reported a case of an isolated osteochondral fracture of the fourth metatarsal head, which was not initially diagnosed and therefore was not treated. Despite that, the patient went well, but remained with a persistent dislocation of the metatarsal articular surface. The mechanism of injury is still debated and was first reported as the result of a direct trauma by Heckman [1]. Later, Dutkowsky and Freeman [2] reported a case of fracture of the 3rd metatarsal head as a result of a shear force. Both mechanisms have been argued since that [3-9]. In this case we consider that the fracture occurred as result of shear force due to the longitudinal stress transmitted to the toe, which forced the base of the proximal phalanx against the dorsal aspect of the metatarsal head when the second toe was in hyperextension at the metatarsophalangeal joint.
Regarding any underling cause, such as Freiberg´s disease, the metatarsal head showed none of the typical pathological features, when evaluated in terms of bone pathology, which leads us to think in favor of a traumatic cause [6,13,14]. Management of osteochondral fracture of the metatarsal head is still controversial and the best treatment is not clear. In the 12 reported cases, four of them underwent initial conservative treatment [1,2,5,7] and the remaining eight went through surgical treatment [3,4,6,9], all with good global outcomes. Regarding conservative treatment through closed reduction and immobilization, Dutkowsky and Freeman [2] reported a loss of 10° active flexion of the third metatarsophalangeal joint on his patient. Liddle, et al. [5] reported failure of the conservative treatment of an osteochondral fracture of the second metatarsal head. After 5 months, open reduction and internal fixation was performed with a good clinical and radiological result. The first description of an open reduction and internal fixation was reported by Tanaka, et al. [3]. They described a good outcome for an isolated osteochondral fracture of the second metatarsal head treated by open reduction and internal fixation with a Herbert screw. A different fixation technique, with two cross Kirschner wires was described by Atik, et al. [6].
In one of his four cases, Lui [7] has reported a plantar protrusion of the screw tip after a surgical treatment of an osteochondral fracture of the second metatarsal head. The screws were removed after 10 months with improvement of the patient’s symptoms. Although some of these fractures could be treated by closed reduction, the potential need for surgical intervention should remain as an option and performed when there is significant dislocation or rotation of the fragment. In such cases, forced closed reduction maneuvers can damage tissues and vascularization, as the lesser metatarsal heads have a precarious blood supply at risk from injury [15]. In this case, as we were in the presence of a retroverted osteochondral fragment, no attempt of close reduction was performed, in order to protect the osteochondral fragment. Open reduction and internal fixation with a single Herbert screw was preformed, achieving and excellent clinical outcome with no pain and full range of motion. Although a longer follow-up is needed, no clinical or radiological evidence of avascular necrosis or arthritic changes of the second metatarsal head were found at the final 12 months screening. As in all intra-articular fractures, we believe that the major prognostic factors are anatomical reduction and prevention of avascular necrosis [4,5,8].
Conclusion
This case highlights the importance of a careful clinical and radiological evaluation of these rare lesions in order to avoid the undesirable sequelae of a missing diagnosis. The viability and the position of the fragment should be taken into account when deciding the treatment. Our case suggests that open reduction and rigid internal fixation can lead to a better outcome and faster return to normal function.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Heckman JD (1991) Fractures and dislocations of the foot. In: Rockwood CA, Green DP, (Eds.). Fractures. 3rd (Edn.). Philadelphia, PA: J.B. Lippincot, pp. 2155.
- Dutkowsky J, Freeman BL (1989) Fracture-dislocation of the articular surface of the third metatarsal head. Foot Ankle 10(1): 43-44.
- Tanaka Y, Takakura Y, Kamei S, Tamai S (1995) An unusual osteochondral fracture of the second metatarsal head. The Foot 5(1): 47-49.
- Mereddy PK, Molloy A, Hennessy MS (2007) Osteochondral fracture of the fourth metatarsal head treated by open reduction and internal fixation. J Foot Ankle Surg 46(4): 320- 322.
- Liddle AD, Rosenfeld PF (2008) Locked second metatarsal head fracture: a case report. Foot Ankle Int 29(10): 1054-1056.
- Atik A, Ozyurek S, Cicek EI, Kose O (2013) Isolated slipped-retroverted osteochondral fracture of second metatarsal head. Foot (Edinb) 23(4):176-179.
- Lui TH (2015) Isolated osteochondral fracture of the metatarsal head of lesser toes. Foot Ankle Surg 21(2): e40-e44.
- Temiz A, Atici T (2015) An Unusual Osteochondral Articular Surface Fracture of Second Metatarsal Head: A Case Report. Journal Of Medical Cases 6(6): 251-253.
- Kurashige T, Suzuki S (2016) An Isolated Chronic Osteochondral Fracture of the Third Metatarsal Head Treated With Bioabsorbable Pins: A Case Report. Foot Ankle Spec 9(6): 555-559.
- Tsujii M, Hasegawa M, Hirata H, Uchida A (2008) Subchondral insufficiency fracture of the second metatatarsal head in an elderly woman treated with autologous osteochondral transplantation. Arch Orthop Trauma Surg 128(7): 689-693.
- Lechevalier D, Fournier B, Leleu T, Crozes P, Magnin J, et al. (1995) Stress fractures of the heads of the metatarsals. A new cause of metatarsal pain. Rev Rhum Engl Ed 62(4): 255-259.
- Chowchuen P, Resnick D (1998) Stress fractures of the metatarsal heads. Skeletal Radiol 27(1): 22-25.
- Love JN, O'Mara S (2010) Freiberg's disease in the Emergency Department. J Emerg Med 38(4): e23-25.
- Kenny L, Purushothaman B, Teasdale R, El Hassany M, Parvin B (2017) Atypical Presentation of Acute Freiberg Disease. J Foot Ankle Surg 56(2): 385-389.
- Petersen WJ, Lankes JM, Paulsen F, Hassenpflug J (2002) The arterial supply of the lesser metatarsal heads: a vascular injection study in human cadavers. Foot Ankle Int 23(6): 491-495.

 Case Report
Case Report